Last Updated on November 20, 2025 by Ugurkan Demir
Pre B cell acute lymphoblastic leukemia (pre-B ALL) is the most common cancer in children. At Liv Hospital, we aim to provide families with accurate information and compassionate support. Understanding pre B cell acute lymphoblastic leukemia, its signs, diagnosis, treatment options, and ongoing care is vital for parents and caregivers.
With proper treatment, pre B cell acute lymphoblastic leukemia is highly treatable, and survival rates are very encouraging. In this article, we’ll share seven key facts about this common childhood cancer to help families navigate the journey with confidence and knowledge.
Key Takeaways
- Pre-B ALL is the most prevalent form of childhood leukemia.
- Advanced care and patient-centered providers improve survival rates.
- Understanding symptoms and diagnosis is key to effective treatment.
- Treatment options vary based on the child’s condition and medical history.
- Long-term care is essential for managing the disease’s impact.
What is B-Cell Acute Lymphoblastic Leukemia in Children?
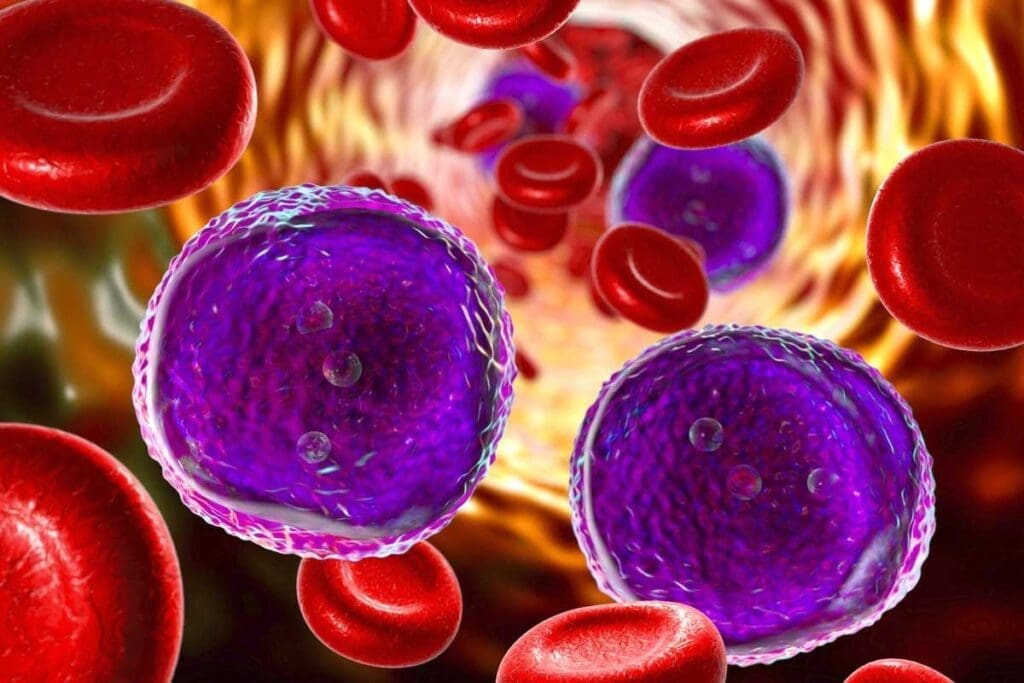
We will look into B-cell acute lymphoblastic leukemia, a cancer found in children’s immature B cells. B-cell acute lymphoblastic leukemia (B-ALL) is marked by the unchecked growth of lymphoblasts in the bone marrow and blood.
Definition and Classification of B-ALL
B-ALL is a cancer that affects the blood and bone marrow. It’s classified based on certain genetic traits and the B cells’ maturity. The World Health Organization (WHO) system is often used to sort B-ALL into various subtypes.
How B-Cell Leukemia Differs from Other Types
B-ALL is different from other leukemias due to its unique genetic and molecular features. Unlike T-cell acute lymphoblastic leukemia, B-ALL starts in immature B cells. This difference is key to finding the best treatment.
Overview of Childhood Leukemia Types
Childhood leukemia includes acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). B-ALL is the most common ALL subtype in kids. Knowing the different leukemia types is vital for accurate diagnoses and treatment plans.
In summary, B-cell acute lymphoblastic leukemia is a serious and aggressive disease that needs quick diagnosis and treatment. By understanding its definition, classification, and differences from other leukemias, we can better manage it in children.
Fact 1: Pre-B Cell Acute Lymphoblastic Leukemia is the Most Common Childhood Cancer
Pre-B cell acute lymphoblastic leukemia (pre-B ALL) is the top cancer in kids. It makes up about 40% of all cancers in children. This is a big deal for kids’ health.
Statistical Prevalence in Pediatric Oncology
Pre-B ALL is a big worry in kids’ cancer. It happens in about 3 to 4 kids out of 100,000 each year. Doctors and healthcare workers really focus on this.
Key statistics include:
- Pre-B ALL makes up 80% of all acute lymphoblastic leukemia in kids.
- Most cases happen between 2 and 5 years old.
- It’s more common in kids under 10.
Age Distribution and Peak Incidence
Pre-B ALL mostly affects kids between 1 and 10 years old. Most cases are seen between 2 and 5 years. Knowing this helps doctors catch it early.
The highest number of cases in early childhood hints at something. It might be linked to how kids develop. More research could help prevent it and improve treatment.
Knowing how common and when pre-B cell acute lymphoblastic leukemia happens helps us help kids. This knowledge is key to making kids’ cancer care better.
Fact 2: The Biology Behind B-ALL Development
B-Cell Acute Lymphoblastic Leukemia (B-ALL) starts with genetic changes in young B lymphocytes. It’s a blood and bone marrow cancer where lymphoblasts grow out of control.
Origin in Immature B Lymphocytes
B-ALL comes from young B cells, or lymphoblasts, which are on their way to becoming mature B lymphocytes. These cells get genetic mutations that stop them from growing properly. This leads to cancer.
Proliferation of Lymphoblasts in Bone Marrow
The cancer cells grow in the bone marrow, taking over and pushing out normal cells. A notable hematologist said,
“The bone marrow gets too full of bad cells, making it hard to make healthy blood.”
This is a key part of B-ALL and helps it spread.
Genetic and Molecular Characteristics
B-ALL has specific genetic and molecular changes, like chromosomal shifts and gene mutations. These changes help doctors diagnose and plan treatment. Some changes mean a patient might face a higher risk of coming back or not responding well to treatment.
Knowing how B-ALL starts is key to finding better treatments. By looking at the genetic and molecular signs of B-ALL, doctors can make treatments more personal. This can help patients live longer and avoid serious side effects.
Fact 3: Recognizing Symptoms of Pre B Acute Lymphocytic Leukemia
It’s important to know the symptoms of pre-B acute lymphocytic leukemia early. This type of leukemia shows different signs that can be hard to spot. Early detection is key to treatment.
Common Clinical Presentations
Children with pre-B ALL often feel fatigued, have fevers, and bruise easily. These signs happen because the bone marrow fills with cancer cells. This reduces the number of healthy blood cells.
A pediatric oncologist says, “The first signs of ALL can be tricky. They might look like common childhood illnesses. So, it’s vital for parents to watch for symptoms that don’t go away.”
“The early signs of ALL can be subtle and may resemble common childhood illnesses, making it essential for parents to be vigilant about persistent symptoms.”
– As noted by experts.
Rapid Onset Characteristics
Symptoms of pre-B ALL can appear quickly. Some kids get worse fast. This is because the disease is aggressive and can cause a lot of white blood cells.
High White Blood Cell Count Manifestations
A high white blood cell count is a big sign of pre-B ALL. It can cause enlarged lymph nodes, a big spleen, and bone pain. These problems come from cancer cells building up in these areas.
Knowing these symptoms can help families get help fast. This could make a big difference for kids with pre-B ALL.
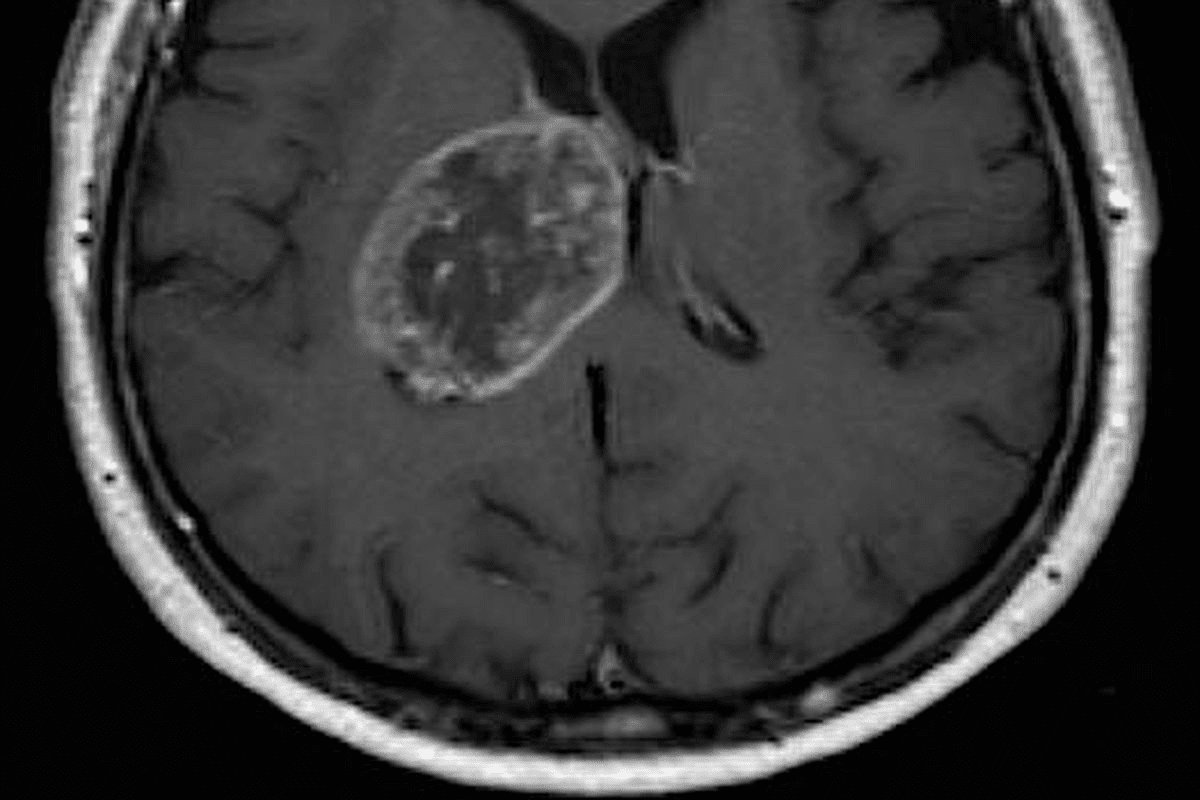
Fact 4: Diagnosis and Classification of B-Cell ALL
Understanding the B-cell acute lymphoblastic leukemia diagnosis is key to treatment. It involves several steps. These steps include various tests to confirm the disease’s presence and type.
Initial Evaluation and Blood Tests
The first step is an initial evaluation and blood tests. These tests check for abnormal blood cell counts. They look at white blood cells, red blood cells, and platelets.
Bone Marrow Examination
A bone marrow examination is vital for diagnosing B-ALL. It takes a bone marrow sample, usually from the hip. This sample is checked for leukemia cells.
Immunophenotyping and Genetic Testing
Immunophenotyping identifies the type of leukemia cells. Genetic testing, like cytogenetic analysis, finds genetic abnormalities. These tests help plan the best treatment.
Risk Stratification Process
The risk stratification process looks at several factors. These include age, white blood cell count, genetic characteristics, and treatment response. It categorizes patients into risk groups, guiding treatment intensity.
| Risk Category | Characteristics | Treatment Approach |
| Standard Risk | Age 1-9 years, WBC | Standard chemotherapy protocol |
| High Risk | Age ≥10 years, WBC ≥50,000/µL, unfavorable genetic features | Intensive chemotherapy, possible stem cell transplantation |
Accurate diagnosis and classification of B-cell ALL are vital for effective treatment. Understanding the disease’s characteristics helps tailor treatment. This improves outcomes and reduces complications.
Fact 5: Treatment Approaches for Leukemia Type B
The treatment for B-cell ALL is complex, with many options. Each child’s treatment plan is based on their risk level. It’s important for families to understand these options.
Standard Chemotherapy Protocols
Chemotherapy is key in treating B-cell ALL. Multi-agent chemotherapy protocols aim to kill cancer cells. The treatment’s intensity and length depend on the child’s risk level.
This risk level is based on age, white blood cell count, and how well the child responds to treatment.
Stem Cell Transplantation for High-Risk Cases
Children at high risk or who relapse might need a stem cell transplant. This involves replacing their bone marrow with healthy stem cells. These can come from a donor or the child themselves, if saved before chemotherapy.
Targeted Therapies and Immunotherapy
New treatments like targeted therapies and immunotherapy are being used. These include monoclonal antibodies and CAR-T cell therapy. They aim to kill cancer cells while protecting healthy tissues.
Treatment Phases and Duration
Treatment for B-cell ALL goes through several phases: induction, consolidation, and maintenance. It usually lasts 2-3 years. Knowing about these phases and their side effects helps families prepare.
By using these treatments together, we can improve outcomes for kids with B-cell ALL. Research is ongoing to make treatments even better, giving hope for the future.
Fact 6: Prognosis and Survival Rates for B-Cell ALL Leukemia in Children
Children with B-cell Acute Lymphoblastic Leukemia (B-ALL) have a better outlook today. Thanks to new treatments and care, their chances of survival have greatly improved.
Overall Cure Rates Exceeding 90%
Good news in pediatric oncology is that over 90% of kids with B-cell ALL can be cured. This shows how well modern treatments work.
High cure rates come from using treatments that match each child’s risk level. This makes treatment more effective.
Prognostic Factors and Risk Groups
How well a child with B-cell ALL does depends on several factors. These include age, how many white blood cells they have, genetic changes, and how they react to treatment.
Doctors sort patients into risk groups based on these factors. This helps decide the best treatment plan.
Special Considerations for Infant B-ALL
Infants with B-ALL face special challenges. They often have different genetic issues and a different outlook than older kids.
Targeted therapies are being tested to help this high-risk group.
Knowing about B-cell ALL’s prognosis and survival rates is key for families and doctors. It helps make better treatment and care choices.
Fact 7: Long-term Effects and Follow-up Care
The journey doesn’t end with the completion of treatment for B-cell ALL. Instead, it moves into a critical phase of follow-up care. As treatment for b cell lymphoblastic leukemia has improved, we focus on reducing long-term effects. We aim to improve the quality of life for survivors.
Late Effects of Treatment
Children treated for pre-B acute lymphoblastic leukemia may all face late effects. These can include physical, emotional, and cognitive challenges. These effects come from chemotherapy, radiation, or other treatments.
Common late effects include growth issues, heart problems, and a higher risk of secondary cancers.
Long-term Monitoring Protocols
Long-term monitoring is key to addressing these late effects. Regular follow-up care involves a team of healthcare providers. They work together to monitor the child’s health and catch any issues early.
This care is tailored to each child’s needs and history. It helps manage late effects effectively.
Quality of Life After Treatment
Improving survivors’ quality of life is a main goal of long-term care. This care goes beyond managing medical issues. It also supports the emotional and psychological well-being of the child and their family.
By providing complete care and resources, we help survivors live healthy, fulfilling lives. As we improve B-cell lymphoblastic leukemia treatment, we must also focus on long-term care. This ensures the benefits of modern treatment are fully realized. It also ensures survivors get the support they need to thrive.
Supporting Families Through the B-ALL Journey
The journey through B-cell acute lymphoblastic leukemia diagnosis and treatment is tough. Families must face challenges together. A B-ALL diagnosis affects not just the child but the whole family, needing strong support.
Resources for Parents and Caregivers
Parents and caregivers of children with B-ALL need reliable resources. They need emotional support and practical guidance. Organizations like the Children’s Oncology Group provide valuable information and support networks.
“Support is key for families dealing with B-ALL treatment,” they say. Community and professional guidance are vital.
Navigating School and Social Challenges
Children with B-ALL face big challenges when going back to school and social settings. Families must work with educators to create reintegration plans. These plans should support the child’s educational and emotional needs.
Effective communication between healthcare providers, families, and schools is essential. It helps ensure a smooth transition.
Sibling and Family Support
Siblings of children with B-ALL may feel left out or neglected. They need support to cope with their feelings. Counseling or support groups can help them.
Families should keep open lines of communication. This helps address the needs of all family members.
Conclusion
Pre B cell acute lymphoblastic leukemia is a complex condition that affects children. But thanks to medical advancements, it’s now treatable. We’ve looked at seven key facts about this disease, covering its definition, prevalence, treatment, and prognosis.
As healthcare providers, we’re committed to top-notch care and support for families with B-ALL. We’ve talked about the importance of early diagnosis and the different treatment options for leukemia type B. We’ve also discussed the long-term effects of the disease.
Understanding the biology behind B-cell ALL and its symptoms helps us improve diagnosis and treatment. The good news is that the prognosis for children with B-cell ALL has greatly improved. Cure rates are now over 90%.
We hope this information has been useful and helpful in your journey with your child. Our team is here to offer full support and guidance. We’re dedicated to helping through the treatment process for pre B cell acute lymphoblastic leukemia and b cell all leukemia.
FAQ
What is B-cell acute lymphoblastic leukemia (B-ALL)?
B-cell acute lymphoblastic leukemia (B-ALL) is a blood and bone marrow cancer. It happens when immature B cells, called lymphoblasts, grow too much.
What are the common symptoms of pre-B acute lymphocytic leukemia?
Symptoms include feeling very tired, having a fever, bruising easily, and high white blood cell counts. Spotting these signs early is key to treatment.
How is B-cell ALL diagnosed?
Doctors use many tests to diagnose B-cell ALL. These include blood tests, bone marrow exams, and genetic tests. They help confirm the disease and its type.
What are the treatment approaches for leukemia type B?
Treatments include standard chemotherapy, stem cell transplants for high-risk cases, and new therapies like targeted and immunotherapy. These aim to improve survival rates.
What is the prognosis for children with B-cell ALL?
The outlook for kids with B-cell ALL has greatly improved. Cure rates are over 90%. The disease’s risk level affects the outcome.
What are the long-term effects of treatment for B-cell ALL?
Treatment can lead to health issues later on. It’s important to monitor these effects closely. This ensures a good quality of life after treatment.
How can families be supported through the B-ALL journey?
Families need support from the start. This includes help with school, social challenges, and caring for siblings. A strong support system is vital.
What is pre-B cell acute lymphoblastic leukemia (pre-B ALL)?
Pre-B cell ALL is the most common leukemia in kids. It makes up about 40% of all childhood blood cancers.
What is the role of genetic testing in B-cell ALL diagnosis?
Genetic tests find specific mutations in B-ALL. They help doctors diagnose and understand the disease’s risk level.
How does B-cell leukemia differ from other types of leukemia?
B-cell leukemia is unique because it involves immature B cells. It’s different from other leukemias that affect different cell types or stages.
References
- Terwilliger, T., & Abdul-Hamid, B. (2017). Acute lymphoblastic leukemia: a comprehensive review. Blood Cancer Journal, (Nature) 7, 790. https://www.nature.com/articles/bcj201753
- Lee, J. W., Lim, N., & Huh, J. (2017). Prognostic factors and treatment of pediatric acute lymphoblastic leukemia. Blood Research, 52(2), 79-84. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5461276/