
Detailing the main triggers of an ra flare up and describing what the symptoms of acute joint inflammation feel like.
Living with rheumatoid arthritis means dealing with unpredictable times of worse symptoms. Pain, swelling, and tiredness get much worse during these times. These episodes, called RA flare-ups, can happen suddenly or after certain triggers.
It’s important to know what causes these bad times and how they affect your body. By understanding your own flare patterns, you can manage your health better. This way, you can work closer with your healthcare team.
Key Takeaways
- RA flare-ups are periods of increased disease activity, characterized by heightened inflammation and worsening symptoms.
- Understanding the causes of RA flare-ups is key to managing them well.
- Knowing your own flare patterns helps you take charge of your health.
- Working closely with your healthcare team is important for managing RA flare-ups.
- Recognizing triggers can help you prepare for and predict RA flare-ups.
Understanding Rheumatoid Arthritis and Disease Activity

RA, or rheumatoid arthritis, is an autoimmune disease. It makes the immune system attack the lining of the joints. This leads to inflammation and pain. Nisha Manek, M.D., from Medical organization, says, “Rheumatoid arthritis is an inflammatory condition. It’s also associated with the immune system.”
The Autoimmune Nature of RA
Rheumatoid arthritis happens when the immune system attacks the synovium, the lining of the joints. This causes inflammation, making joints swollen, painful, and stiff. If not managed, this can damage joints and cause deformity.
The disease can also affect other parts of the body. This includes the skin, eyes, lungs, heart, and blood vessels.
Distinguishing Between Baseline Symptoms and Flares
People with RA often have baseline symptoms like joint pain, stiffness, and fatigue. But, RA flare-ups happen when these symptoms get worse. About 79 percent of RA flares last less than 3 days. Flares can last weeks or months without treatment.
Knowing the difference between baseline symptoms and flare-ups is key. It helps patients get the right medical care. By working with healthcare providers, people with RA can manage their symptoms better. This reduces the number and severity of flares.
What Exactly Is an RA Flare Up?
RA flare-ups are a big worry for those with rheumatoid arthritis. They bring unpredictable and intense symptoms. These episodes make the condition worse, leading to more pain, stiffness, and other symptoms.
Definition and Characteristics
An RA flare-up means the disease is acting up more. Symptoms get worse, like intense pain and stiffness in the joints. You might also feel fatigue, fever, and rashes.
During a flare-up, joints can swell, turn red, and feel warm. The pain can be so bad it stops you from moving. Feeling tired and having a fever can also make things harder.
Duration and Frequency Patterns
The duration of RA flare-ups varies. Some last just a few days, while others can go on for weeks or months. How often they happen also varies.
Knowing when and how long flare-ups last is key to managing them. By catching the signs early, you can work with your doctor to lessen their impact. Keeping a journal of your symptoms can help track these patterns.
We’ll look at what causes RA flare-ups next. This will help you understand how to manage and maybe even prevent them.
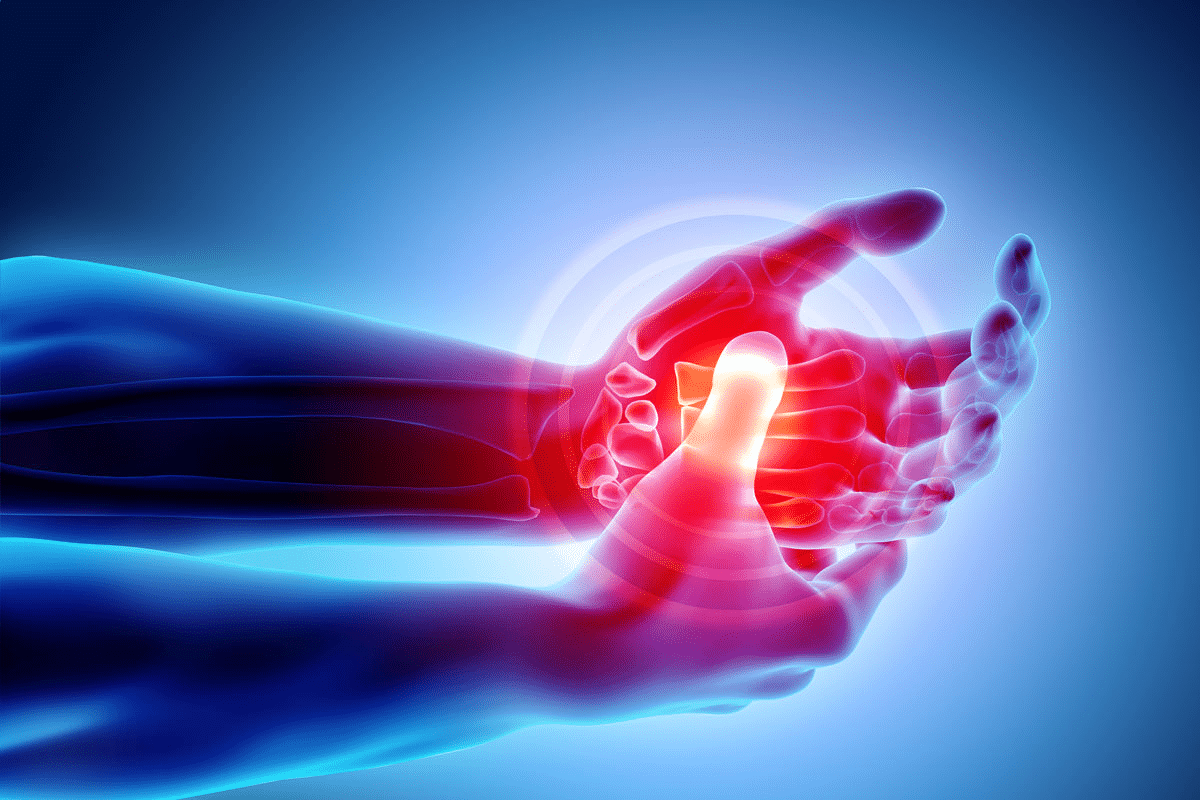
Common Symptoms of RA Flare Ups
Knowing the symptoms of RA flare-ups is key to managing them well. When rheumatoid arthritis flares, patients face many symptoms that can really affect their life.
Joint Pain and Stiffness Intensification
Joint pain and stiffness get worse during an RA flare. This makes it hard to do everyday things. Joint pain can feel like a dull ache or a sharp stab, and it might be swollen, red, and warm.
Systemic Symptoms: Fatigue, Fever, and Rashes
RA flare-ups also bring systemic symptoms. Fatigue is a big one, as RA’s inflammation makes people feel very tired. Some people get fever, showing the body’s fight against inflammation. Rashes or skin issues can also happen, making things even harder.
These symptoms affect more than just the joints. They can make patients feel really unwell, like they have the flu. It’s a big challenge for their overall health.
How Symptoms Differ From Everyday RA
Telling a flare-up from everyday RA symptoms is important. While some pain and stiffness are normal, a flare-up is much worse. Patients need to know their usual symptoms and watch for big changes, like more pain, longer stiffness, or fever.
By knowing these differences, patients can get help sooner and adjust their treatment. RA can also raise the risk of heart disease due to chronic inflammation. This can lead to atherosclerosis, where plaque builds up in arteries.
Many things can set off RA flare-ups, like too much activity, bad sleep, stress, infections, hormonal shifts, weather changes, air pollution, and pesticide exposure. Knowing these triggers helps patients manage their condition better.
What Does a Rheumatoid Arthritis Flare Feel Like?
Living with rheumatoid arthritis (RA) means dealing with unpredictable flares. These can mess with your body and mind. Each person’s experience with an RA flare is different.
Patient Experiences and Descriptions
People with RA say flares make their joints hurt more, feel stiff, and swell. “It’s like my joints are on fire,” one patient shared.
“The pain is not just in my joints; it feels like my whole body is aching, and I’m exhausted all the time.”
These stories show RA flares can hurt more than just your joints. They can affect your whole health.
The Emotional and Psychological Impact
RA flares also hit your emotions hard. The uncertainty of when a flare will happen can cause a lot of stress. Healthcare providers need to care for both your body and mind. Studies show the emotional pain of RA can be as tough as the physical.
RA Flare Up Flu-Like Symptoms
Some RA patients feel flu-like during a flare. They might have a fever, feel very tired, and not feel well overall. “It’s like having a constant flu,” one patient said. These symptoms show RA affects your whole body, not just your joints.
People with RA are also more likely to get other autoimmune diseases. Knowing all the symptoms of RA, including flu-like ones, is key to good care.
Primary Triggers of RA Flare Ups
Several primary triggers can lead to RA flare-ups. Understanding these can improve patient outcomes. RA flare-ups are periods of increased disease activity. Inflammation levels rise, and symptoms worsen.
By identifying and managing these triggers, patients can take proactive steps. This helps minimize their impact.
Physical Overexertion and Activity Levels
Physical overexertion is a big trigger for RA flare-ups. Doing too much or suddenly increasing exercise can make symptoms worse. It’s key to find a balance between staying active and avoiding too much strain.
Gentle exercises like yoga or swimming can help. They keep joints moving without too much strain.
Managing physical activity is important. Here are some tips:
- Listen to your body and rest when needed
- Gradually increase exercise intensity and duration
- Include low-impact activities in your routine
Sleep Disruption and Chronic Fatigue
Sleep disruption and chronic fatigue are linked to RA flare-ups. Poor sleep can make fatigue worse, which can worsen RA symptoms. Getting enough rest and keeping a regular sleep schedule is key.
Establishing a relaxing bedtime routine can improve sleep quality. Here are some strategies for better sleep:
- Create a sleep-friendly environment
- Avoid caffeine and electronics before bed
- Do stress-reducing activities
Psychological Stress and Emotional Factors
Psychological stress is a known trigger for RA flare-ups. Stress can increase inflammation and worsen symptoms. Managing stress through meditation, deep breathing, or cognitive-behavioral therapy can help. Having a strong support network and seeking professional help when needed is also important.
Effective stress management techniques include:
- Mindfulness and meditation practices
- Journaling or expressive writing
- Seeking support from mental health professionals
Skipping medication or changing treatment without a doctor’s advice can lead to flare-ups. It’s vital to stick to your treatment plan and talk to your healthcare provider before making any changes.
Environmental and Biological Causes of Rheumatoid Arthritis Flares
It’s important to know what triggers rheumatoid arthritis (RA) flares. RA is a complex disease influenced by genetics, lifestyle, and the environment.
Infections and Immune System Challenges
Infections can make RA worse. When the body fights off an invader, it can overreact in people with RA. This can lead to more inflammation and pain.
Viral infections like the flu or bacterial infections like UTIs can set off this overreaction. To prevent this, staying up-to-date on vaccines and practicing good hygiene is key.
Weather Changes and Barometric Pressure
Many with RA find that weather changes can cause flares. The exact reason is unclear, but changes in barometric pressure might play a part. Barometric pressure is the weight of the atmosphere’s pressure.
Research suggests that these pressure changes can irritate joints and muscles. This irritation can lead to pain in people with RA.
Environmental Pollutants and Pesticide Exposure
Exposure to pollutants and pesticides can also trigger RA flares. Air pollution, in particular, can make RA symptoms worse. Pollutants like particulate matter and ozone can irritate joints and cause inflammation.
Exposure to certain pesticides can also increase the risk of RA. To avoid this, staying informed about air quality and using air purifiers at home is helpful. Avoiding polluted areas and wearing protective gear when using pesticides can also reduce risk.
By understanding these causes, patients with RA can take steps to reduce their exposure. This can help decrease the frequency and severity of flares.
Hormonal Influences on Rheumatoid Arthritis Exacerbation
It’s important to know how hormones affect RA. Hormonal changes, like those in estrogen, can really impact RA in women.
Estrogen Fluctuations and Menstrual Cycle
Women with RA often see their symptoms change with their menstrual cycle. Research shows that estrogen might help control the immune system. This could affect how RA acts.
Some studies say symptoms can get worse right before or during menstruation. This is a common experience for many women with RA.
Pregnancy, Postpartum, and Menopause Effects
Pregnancy brings big hormonal changes. For some women, this means their RA symptoms get better. But, not all women see this improvement.
After pregnancy, when hormone levels drop, symptoms can flare up again. This is a common pattern for many women.
Menopause also brings big hormonal changes. Some women see their RA symptoms change. The drop in estrogen might make symptoms worse for some.
|
Hormonal Event |
Effect on RA Symptoms |
|---|---|
|
Menstruation |
Variable; some experience worsening symptoms |
|
Pregnancy |
Often improves symptoms, but not always |
|
Postpartum |
Frequently associated with flare-ups |
|
Menopause |
Variable; may see an increase in disease activity |
Knowing how hormones affect RA helps doctors give better care. They can adjust treatments to help women with RA live better lives.
Diagnosing and Treating RA Flare Ups
Handling RA flare-ups needs teamwork between patients and doctors. It’s about using medicine, changing your lifestyle, and taking care of yourself.
Collaborating With Your Rheumatologist
It’s key to work with your rheumatologist during a flare-up. They can tweak your treatment to ease your symptoms. It’s important to talk about any changes in your symptoms or side effects from your meds.
To work well together, consider these tips:
- Keep a symptom journal to track your flare-ups.
- Write down your questions and concerns before visits.
- Talk about any issues with your treatment plan.
Medication Adjustments and Treatment Options
Medicine is a big part of managing RA flare-ups. Over-the-counter NSAIDs can help with pain and swelling. For worse flares, corticosteroids might be needed. Your doctor might also suggest biologic treatments or DMARDs for long-term care.
|
Medication Type |
Use During Flare-Ups |
Potential Side Effects |
|---|---|---|
|
NSAIDs |
Pain and inflammation relief |
Gastrointestinal issues, kidney problems |
|
Corticosteroids |
Reducing severe inflammation |
Weight gain, mood changes, increased infection risk |
|
Biologics |
Targeted therapy for RA |
Increased infection risk, allergic reactions |
Self-Management Strategies and Home Remedies
There are also things you can do at home to feel better. Resting, using heat or cold packs, and trying stress-reducing activities like meditation can help.
Using medicine and these self-care steps can help manage RA symptoms. This way, flare-ups won’t disrupt your daily life as much.
Conclusion: Living With RA and Long-Term Outlook
Living with rheumatoid arthritis means taking a full approach. This includes medical care and healthy habits every day. Knowing what causes and triggers RA flare-ups helps patients manage their condition better.
For over 40 years, groups like the Arthritis Research and Education Foundation have supported RA patients in the U.S. The right treatment and support can make flares less common and easier to handle. This lets patients live active and meaningful lives.
To manage RA well, patients need to work with their healthcare team, make lifestyle changes, and stay active in their care. This way, they can have a better long-term outlook for RA and enjoy a good quality of life.
FAQ
What is a rheumatoid arthritis flare-up?
A rheumatoid arthritis flare-up is when the disease gets worse. You might feel more pain, stiffness, and fatigue. You could also get a fever.
What causes rheumatoid arthritis flare-ups?
Many things can trigger a flare-up. This includes too much activity, not enough sleep, stress, infections, weather changes, and pollution.
What are the common symptoms of an RA flare-up?
Symptoms of a flare-up include more pain and stiffness in your joints. You might also feel very tired, have a fever, or get rashes. These symptoms are usually worse than usual.
How do RA flare-ups feel?
Flare-ups make symptoms much worse. You might feel a lot of pain, stiffness, and tiredness. You could also feel stressed and have flu-like symptoms.
Can hormonal changes trigger RA flare-ups?
Yes, changes in hormones can affect your RA. This includes during your period, pregnancy, after having a baby, and during menopause.
How can RA flare-ups be managed?
Managing flare-ups involves several steps. You might need to change your medication, manage stress, get enough sleep, and avoid triggers.
What is the role of a rheumatologist in managing RA flare-ups?
A rheumatologist helps a lot during flare-ups. They adjust your treatment, teach you how to manage your symptoms, and support you when your disease is active.
Can RA flare-ups be prevented?
You can’t stop flare-ups completely, but you can reduce them. Avoiding triggers, staying healthy, and following your treatment plan can help.
How long do RA flare-ups typically last?
Flare-ups can last from a few days to months. How long it lasts depends on your treatment and how well you manage your symptoms.
What are some self-management strategies for RA flare-ups?
To manage flare-ups, rest, use heat or cold packs, reduce stress, and adjust your activities. This helps ease your symptoms and protect your joints.
References
World Health Organization. Evidence-Based Medical Guidance. Retrieved from https://www.who.int/news-room/fact-sheets/detail/rheumatoid-arthritis



































