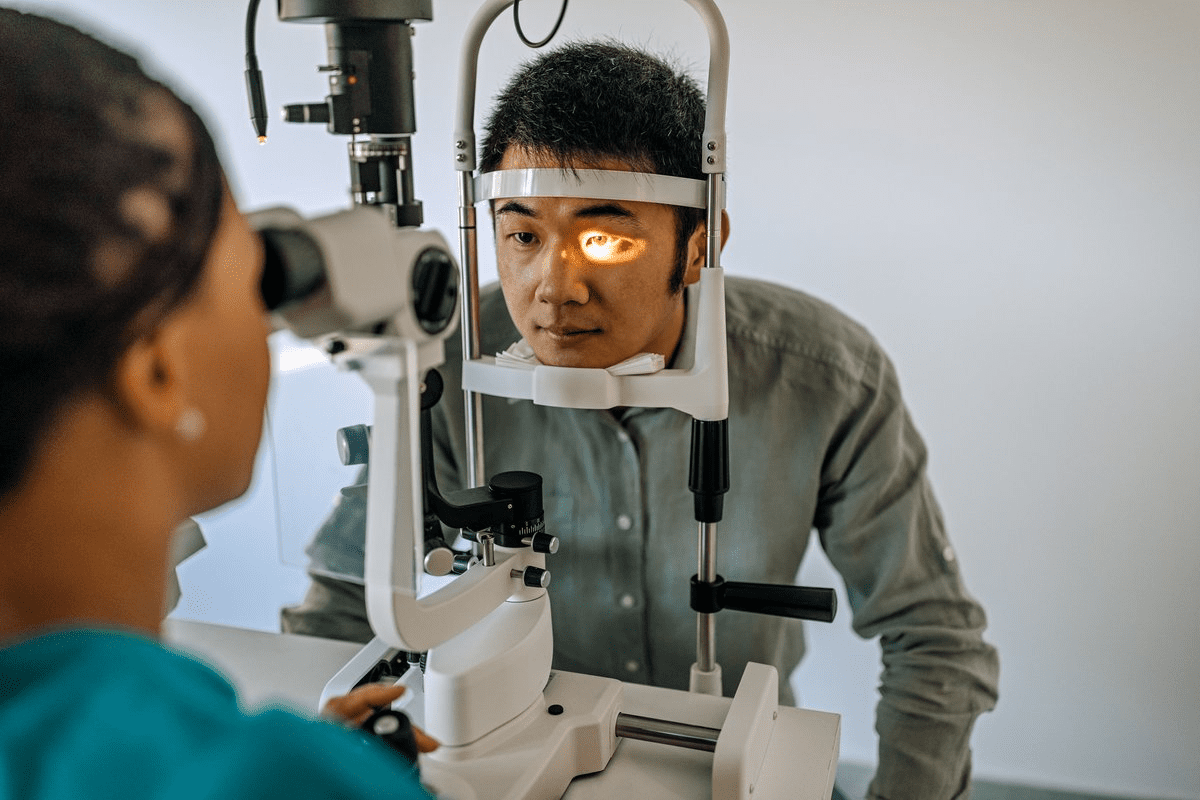
At Liv Hospital, we use advanced slit lamp techniques to check for inflammation in the front part of the eye. This is key for diagnosing and treating eye problems like uveitis. The slit lamp is a stereoscopic biomicroscope that shines a focused light. It lets us see the fine anatomy of the anterior segment in 3D. Guide to understanding cell and flare eye appearance as a sign of inflammation on a slit lamp exam. Assess cell and flare eye.
We look for cell and flare on the slit lamp to spot inflammation. Cells are white blood cells, and flare is protein leaking from blood vessels. By spotting these signs, we can choose the best treatment for our patients.
Key Takeaways
- Slit lamp biomicroscopy is key for spotting inflammation in the front of the eye.
- Cell and flare are important signs of inflammation in the eye’s front part.
- Spotting cell and flare helps us decide on the right treatment.
- Liv Hospital’s eye doctors use the latest slit lamp methods for accurate diagnosis.
- Spotting inflammation in the eye’s front part is vital for managing eye diseases like uveitis.
The Significance of Cell and Flare in Ocular Inflammation
Cell and flare are key signs of eye inflammation. They are important for diagnosing anterior uveitis. These signs show that there is inflammation that needs to be looked at closely and treated.
Clinical Importance in Diagnosing Anterior Uveitis
Anterior uveitis is when the iris and ciliary body get inflamed. Cell and flare are signs of this. We use a slit lamp to see and count these signs, which helps us decide how to treat it.
How much cell and flare there is tells us how bad the inflammation is. More cell and flare means it’s worse and needs stronger treatment. Less means the treatment is working and the inflammation is getting better.
Key factors in assessing cell and flare include:
- The number of cells present in the anterior chamber
- The intensity of flare, which indicates the level of protein leakage
- The presence of other inflammatory signs, such as keratic precipitates or posterior synechiae
Pathophysiological Basis of Inflammatory Signs
Cell and flare happen when the blood-aqueous barrier gets broken. This lets proteins and cells leak into the anterior chamber. This break is often caused by inflammation, which can come from infections, injuries, or autoimmune diseases.
“The assessment of cell and flare is fundamental in understanding the inflammatory process within the eye and guiding appropriate management strategies.” –
Ocular Inflammation Expert
Knowing why cell and flare happen helps us treat them better. By fixing the cause of the inflammation, we can make cell and flare less severe. This helps patients get better faster.
Anatomy of the Anterior Chamber and Blood-Aqueous Barrier
Understanding the anatomy of the anterior chamber is key for diagnosing and treating eye conditions. The anterior chamber, filled with aqueous humor, is vital for the eye’s health and clear vision.
Normal Structure and Function
The anterior chamber is the space between the cornea and the iris. It’s filled with aqueous humor, a clear fluid made by the ciliary body. The blood-aqueous barrier keeps the aqueous humor clear by stopping blood cells and large proteins from getting in.
Pathological Changes During Inflammation
When the eye gets inflamed, the blood-aqueous barrier breaks down. This lets proteins and cells leak into the aqueous humor. This is shown by cell and flare, signs of inflammation like anterior uveitis.
The amount of cell and flare can tell doctors how severe the inflammation is. This helps in diagnosing and understanding the inflammation’s impact.
Understanding Cell and Flare Eye Findings
Slit lamp biomicroscopy helps us see cells and flare in the eye’s front part. This is key for spotting inflammation and treating it. It’s vital for diagnosing and managing conditions like anterior uveitis.
Definition and Composition of Anterior Chamber Cells
Anterior chamber cells are white blood cells and other inflammatory cells in the aqueous humor. They show that the eye is inflamed. The type of cells can tell us what’s causing the inflammation.
There are different types of cells in the anterior chamber. Knowing which ones are there helps us figure out why the eye is inflamed.
Cell Type | Description | Clinical Significance |
Lymphocytes | Small, round cells involved in immune responses | Indicate chronic inflammation or infection |
Neutrophils | Multilobed nucleus, often associated with acute inflammation | Suggest acute infection or severe inflammation |
Pigment-laden Cells | Cells containing pigment, often from the iris or retina | May indicate trauma, surgery, or certain retinal conditions |
The Tyndall Effect: Mechanism of Flare
Flare in the anterior chamber comes from the Tyndall effect. This is when light scatters off protein particles in the aqueous humor. It happens when the blood-aqueous barrier gets broken, letting proteins leak into the aqueous humor.
“The Tyndall effect is the scattering of light by particles in a colloid or in a very fine suspension. In the context of the eye, it refers to the visibility of protein particles in the aqueous humor due to inflammation.”
The amount of flare shows how much protein is leaking. This helps us measure how severe the inflammation is.
Differentiating Normal from Pathological Findings
Telling normal from abnormal findings is key for correct diagnosis and treatment. Normal eyes usually have no or very few cells and no flare. But, if there are cells and flare, it means there’s inflammation.
Abnormal findings are when there are lots of cells and a lot of flare. It’s important to look at other eye signs and symptoms to make a full diagnosis.
Slit Lamp Biomicroscopy: The Gold Standard for Assessment
In ophthalmology, slit lamp biomicroscopy is the top choice for checking inflammation in the front part of the eye. It gives a close-up look at the front segment. This helps doctors spot and keep track of issues like anterior uveitis.
Basic Principles and Setup
To use slit lamp biomicroscopy well, knowing its basics and setting it up right is key. Getting the slit lamp aligned and adjusted properly is vital for a clear view. We start by tweaking the slit beam’s width, height, and angle to see the anterior chamber best.
The slit lamp needs to have a sharp, clear beam to light up the area we’re looking at. We start with a wide beam to get a broad view of the anterior chamber. Then, we narrow it down to see the finer details.
Optimal Techniques for Visualizing Cell and Flare
To see cells and flare, we need to be precise with the slit lamp. A thin slit beam helps spot cells in the aqueous humor, showing inflammation. We aim the beam at a 45-degree angle to the anterior chamber for the best view of cells.
To check flare, which is protein leaking into the aqueous humor, we use a smaller, more focused beam. We look at how much light scatters in the beam to judge flare intensity.
Common Examination Errors and Pitfalls
Even though slit lamp biomicroscopy is key, it can go wrong if not done right. Common mistakes include bad alignment of the slit beam, not enough light, and not adjusting the magnification right.
To steer clear of these mistakes, we make sure the patient’s eye is in the right spot and the slit lamp is focused well. Keeping the slit lamp calibrated and maintained is also key for accurate checks.
Standardization of Uveitis Nomenclature (SUN) Classification
We use the SUN classification to standardize how we look at anterior chamber cells and flare. This system is key in both clinical practice and research. It gives ophthalmologists a common way to describe and measure uveitis.
Development and Purpose of SUN Criteria
The SUN classification was made to have a standard way to grade uveitis. It makes it easier to compare data from different studies and places. The main goal is to help healthcare professionals talk clearly about diagnosis and treatment.
Many leading ophthalmologists and researchers worked together on the SUN classification. Their effort led to a detailed system for measuring the severity of inflammation in the anterior chamber.
Grading Scales for Anterior Chamber Cells
The SUN classification has a detailed scale for grading anterior chamber cells. This scale is key for understanding how severe uveitis is. It ranges from 0 to 4+, with clear criteria for each level:
- 0: No cells
- 0.5+: 1-5 cells
- 1+: 6-15 cells
- 2+: 16-25 cells
- 3+: 26-50 cells
- 4+: >50 cells
This scale helps doctors accurately track and manage inflammation, guiding treatment choices.
Grading Scales for Anterior Chamber Flare
The SUN classification also has a scale for grading anterior chamber flare. The flare is measured from 0 to 4+, based on how strong the Tyndall effect is seen with a slit lamp:
- 0: None
- +1: Faint
- +2: Moderate (iris and lens details clear)
- +3: Marked (iris and lens details hazy)
- +4: Intense (fibrin or plastic aqueous)
Getting flare grading right is key to knowing how severe the inflammation is and if treatment is working.
Clinical Application of SUN Grading
The SUN classification is widely used in clinics, helping manage uveitis better. It standardizes how we look at inflammation in the anterior chamber. This makes:
- Keeping track of disease severity consistent
- Healthcare providers communicate better
- Comparing treatment results in studies more accurate
- Treatment choices based on clear measures of inflammation
The SUN classification is a vital tool in ophthalmology, mainly for diagnosing and treating uveitis. Its use has made clinical assessments more consistent and reliable, improving patient care.
Alternative Methods for Quantifying Anterior Chamber Inflammation
New ways to check for inflammation in the front part of the eye are being developed. These methods aim to give more precise and detailed readings. This could help us better understand and treat eye inflammation.
Laser Flare Photometry
Laser flare photometry is a non-invasive test that measures light in the front part of the eye. It gives a clear number for how much light is scattered. This method is more precise than looking with a slit lamp, making it easier to compare results.
Key benefits of laser flare photometry include:
- Objective quantification of flare
- High sensitivity in detecting subtle changes in flare intensity
- Useful for monitoring treatment response
Anterior Segment OCT
Anterior Segment Optical Coherence Tomography (OCT) is a new tool for detailed eye scans. It’s mainly used for looking at structures, but some research shows it can also spot inflammation.
Potential applications of anterior segment OCT in inflammation assessment include:
- Detailed visualization of inflammatory cells and structures
- Measurement of changes in anterior chamber configuration
- Assessment of complications associated with inflammation
Emerging Technologies and Future Directions
New technologies will likely improve how we measure eye inflammation. Future tools might use advanced image analysis and artificial intelligence for better accuracy.
Future directions may involve:
- Integration of multiple diagnostic modalities for a complete check
- Creating devices that are easier to use and carry
- Improving software to better understand imaging data
These new tools could help us diagnose and treat eye inflammation better. This could lead to better health outcomes for patients.
Clinical Conditions Associated with Cell and Flare
It’s important to know the clinical conditions linked to cell and flare. These signs show inflammation in the eye. This can be due to many eye diseases.
Anterior Uveitis: Patterns and Presentations
Anterior uveitis is a common eye inflammation. It shows up as cells and flare in the eye’s front part. This condition can be mild or severe and linked to other diseases or eye problems.
Anterior uveitis can show up differently in people. Some may have:
- Acute onset with severe inflammation
- Chronic or recurrent inflammation
- Granulomatous or non-granulomatous inflammation
Getting the right diagnosis and type of uveitis is key. It helps find the cause and choose the right treatment.
HLA-B27-Associated Acute Anterior Uveitis
HLA-B27-associated acute anterior uveitis is a specific type. It starts suddenly and is often linked to HLA-B27. It mostly affects young adults and might be related to certain arthritis-like conditions.
Key signs of this condition include:
- Acute onset of symptoms
- Unilateral or alternating unilateral involvement
- High recurrence rate
- Association with systemic conditions like ankylosing spondylitis
Non-Infectious vs. Infectious Causes
Anterior uveitis can be caused by non-infectious or infectious factors. Knowing the difference is important for the right treatment.
Non-infectious causes include:
- Autoimmune disorders
- Trauma
- Masquerade syndromes
Infectious causes include:
- Bacterial infections
- Viral infections (e.g., herpes simplex, varicella-zoster)
- Fungal infections
- Parasitic infections
It’s important to do a thorough test to find the cause.
Masquerade Syndromes
Masquerade syndromes are conditions that look like uveitis but aren’t. They can be:
- Malignancies (e.g., lymphoma)
- Intraocular foreign bodies
- Pigment dispersion syndrome
Spotting masquerade syndromes is key. It helps avoid wrong treatments and manage the real problem well.
Knowing about the different conditions linked to cell and flare helps doctors make better diagnoses. They can then create specific treatment plans.
Differential Diagnosis of Anterior Chamber Findings
When looking at the anterior chamber, we must figure out what’s causing inflammation. Knowing the exact cause is key to treating it right.
Distinguishing Cell from Pigment and Other Particles
It’s important to tell apart cells, pigment, and other stuff in the anterior chamber. Cells usually mean inflammation. Pigment might show past eye injuries or pigment dispersion syndrome.
Other things like lens parts or foreign bodies can also be there. We need to use a slit-lamp biomicroscope to see what they are.
Flare vs. Other Causes of Aqueous Turbidity
Flare, from protein leaking into the aqueous humor, must be told apart from other causes of cloudiness. Things like bleeding or lipid buildup can also make it cloudy.
Doing a full check-up and taking a detailed history helps us make this distinction.
Correlation with Other Clinical Signs
Linking what we see in the anterior chamber with other signs is key. This includes looking at things like redness in the conjunctiva, keratic precipitates, and changes in eye pressure.
Here’s a quick guide on what to look for in the anterior chamber:
Clinical Finding | Differential Diagnosis | Key Diagnostic Features |
Cells | Inflammation, infection, malignancy | Presence of inflammatory cells, cytology |
Pigment | Pigment dispersion syndrome, trauma | Pigment on corneal endothelium, iris transillumination |
Flare | Inflammation, breakdown of blood-aqueous barrier | Protein leakage into aqueous humor, slit-lamp findings |
In conclusion, figuring out what’s going on in the anterior chamber needs a careful and all-around approach. We must consider many possibilities and link them with other signs.
Management Strategies Based on Cell and Flare Assessment
Checking cell and flare on a slit lamp is key to deciding treatment. It helps manage inflammation in the front part of the eye. Knowing how severe the inflammation is and what treatment to use is important.
Treatment Thresholds and Monitoring Parameters
Setting treatment levels is vital for starting or changing therapy. We use grading scales from the Standardization of Uveitis Nomenclature (SUN) Working Group. This helps us measure inflammation severity.
We watch for changes in cell and flare, and other signs like vision and eye pressure. Regular slit lamp exams are part of this.
Inflammation Level | Cells in Anterior Chamber | Flare Grading | Treatment Approach |
Mild | 6-15 cells | +1 | Topical corticosteroids |
Moderate | 16-30 cells | +2 | Intensified topical corticosteroids |
Severe | >30 cells | +3 or +4 | Systemic corticosteroids or immunosuppressive therapy |
Pharmacological Approaches to Anterior Chamber Inflammation
Managing inflammation with drugs mainly uses corticosteroids and immunosuppressants. Corticosteroids are key, available in different forms like eye drops, injections, or pills.
The right drug and how to use it depends on how bad the inflammation is and the patient’s health.
Evaluating Treatment Response
We check how well treatment is working by looking at signs like cell and flare, vision, and more. We change treatment based on how the patient is doing.
Documentation and Follow-up Protocols
Keeping accurate records of what we find and treatment plans is critical. Follow-up plans are made for each patient, based on how bad the inflammation is and the treatment.
By using these strategies, we can improve patient care and lower the chance of complications from inflammation in the front part of the eye.
Special Considerations in Pediatric and Geriatric Populations
When dealing with anterior chamber inflammation, kids and seniors need special care. Their bodies and health issues are different. So, doctors must adjust how they check and treat them.
Age-Specific Challenges in Assessment
Checking for inflammation in young and old people is hard. Kids might not sit quietly for exams. Older folks might have eye problems like cataracts that make it tough.
- In pediatric patients, the challenges include:
- Limited cooperation during slit-lamp examination
- Difficulty in assessing symptoms due to age-related inability to communicate effectively
- Higher risk of complications from inflammation due to developing ocular structures
- In geriatric patients, common challenges are:
- Age-related ocular changes that can mimic or mask signs of inflammation
- Presence of comorbid conditions that may affect treatment choices
- Potential for drug interactions with systemic medications
Interpretation Differences Across Age Groups
How we see inflammation changes with age. For example, what looks mild in an older person might be serious in a child.
Key considerations include:
- Baseline ocular health and previous inflammatory episodes
- Presence of systemic diseases that could influence ocular inflammation
- Age-related changes in the eye that could affect the interpretation of findings
Modified Examination Techniques
To deal with these challenges, doctors use different ways to check eyes. Handheld slit lamps or portable devices help with kids or those who can’t move much.
By using these special methods, we can better understand and help our patients. This makes their care more effective.
Conclusion: The Enduring Value of Cell and Flare Assessment
Cell and flare assessment is key in diagnosing and managing inflammation in the anterior chamber. We use slit lamp biomicroscopy to check how severe the inflammation is. This helps us decide the best treatment.
Understanding the importance of cell and flare is vital for good patient care. It lets us track how well treatments are working. We can then change our approach if needed, which helps improve patient results.
Even as we move forward in eye care, the basics of cell and flare assessment stay the same. By using our skills and the latest tools, like laser flare photometry and anterior segment OCT, we can get even better at diagnosing. This makes our care for patients even better.
The lasting value of cell and flare assessment is in helping us make the right diagnosis and treatment plans. This ensures our patients get the best care for their eye inflammation. By sticking to these principles, we can keep providing top-notch healthcare and support for our patients.
FAQ
What is the significance of cell and flare in diagnosing anterior chamber inflammation?
Cell and flare are important signs of inflammation in the anterior chamber. Cells are white blood cells and flare is protein leakage from blood vessels.
How are cell and flare identified in the anterior chamber?
Slit lamp biomicroscopy is used to spot cell and flare. Cells appear as white blood cells and flare is seen as protein leakage.
What is the Tyndall effect, and how does it relate to flare in the anterior chamber?
The Tyndall effect explains flare. It’s when protein particles scatter light, making the aqueous humor cloudy.
What is the Standardization of Uveitis Nomenclature (SUN) classification, and how is it used?
The SUN classification is a standard for grading inflammation. It helps quantify cells and flare clearly and consistently.
What are some alternative methods for quantifying anterior chamber inflammation?
Laser flare photometry and anterior segment OCT are alternatives. They offer objective measurements and can improve diagnostic accuracy.
How is anterior uveitis diagnosed, and what are its common causes?
Anterior uveitis is diagnosed by looking for cell and flare. It can be caused by many things, including HLA-B27-associated acute anterior uveitis and infections.
How do you differentiate between cells, pigment, and other particles in the anterior chamber?
To tell cells, pigment, and other particles apart, you need to examine them carefully. You also need to look at other clinical signs.
What are the treatment thresholds and monitoring parameters for anterior chamber inflammation?
Treatment and monitoring depend on the cause and severity of inflammation. They guide the use of medications like corticosteroids and immunosuppressants.
How is anterior chamber inflammation managed in pediatric and geriatric populations?
In kids and older adults, managing inflammation requires special care. It involves considering age-specific challenges and using modified examination techniques.
What is the role of slit lamp biomicroscopy in assessing anterior chamber inflammation?
Slit lamp biomicroscopy is key for checking inflammation in the anterior chamber. It gives a detailed view of the anterior segment, helping with diagnosis and treatment.
What are some common errors and pitfalls when using slit lamp biomicroscopy to assess cell and flare?
Common mistakes include wrong alignment, not enough light, and not adjusting the slit beam and magnification properly.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4724061/