Explaining how do doctors check for arthritis using a combination of physical exams, patient history, and blood tests.
Rheumatoid arthritis can be hard to spot early, but new medical tools help a lot. We use the latest blood tests to find rheumatoid arthritis early. This means we can start treatment quickly and help patients get better faster.
Blood tests are key in finding rheumatoid arthritis, like the anti-CCP antibody test. It can find the disease years before symptoms show up. At Liv Hospital, we aim to give top-notch healthcare to everyone, including international patients.
Key Takeaways
- Blood tests are a main way to find rheumatoid arthritis.
- The anti-CCP antibody test can spot rheumatoid arthritis years early.
- Finding it early is vital for treating rheumatoid arthritis well.
- We use advanced blood tests for accurate diagnosis.
- Starting treatment fast helps patients get better.
Understanding Rheumatoid Arthritis and Its Impact

Rheumatoid arthritis is a complex autoimmune disease that affects joints and overall health. It is a chronic condition found in about 1% of the population. It causes a lot of discomfort and can lead to disability.
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a disease where the immune system attacks the joints. This leads to joint inflammation and can cause serious damage if not treated. It often affects both sides of the body equally.
Common Symptoms and Warning Signs
The symptoms of rheumatoid arthritis vary but often include pain, swelling, and stiffness in the joints. Common signs include morning stiffness that lasts for hours, feeling very tired, and losing function in the affected joints. It’s important to recognize these symptoms early for timely treatment.
|
Symptom |
Description |
|---|---|
|
Morning Stiffness |
Stiffness in the joints that persists for hours after waking up |
|
Joint Pain and Swelling |
Pain and swelling in the joints, often symmetrically |
|
Fatigue |
Feeling extremely tired, which can be a result of chronic inflammation |
The Autoimmune Nature of RA
Rheumatoid arthritis is an autoimmune disease. This means the body’s immune system attacks its own tissues. In RA, the immune system attacks the lining of the joints, causing inflammation and symptoms. Understanding this is key to managing the disease.
Living with rheumatoid arthritis is tough, both physically and emotionally. It’s important for patients to work with their healthcare providers. Together, they can create a management plan that meets the patient’s needs.
The Role of Blood Tests in Rheumatoid Arthritis Diagnosis
Doctors use blood tests to help diagnose rheumatoid arthritis. They look for certain autoantibodies in the blood. Tests for rheumatoid factor and anti-CCP antibodies are key.
Why Blood Tests Are Essential
Blood tests are key in diagnosing rheumatoid arthritis. They find specific autoantibodies and markers of inflammation. A leading rheumatologist says, “The presence of certain antibodies, such as rheumatoid factor and anti-CCP, can indicate an increased likelihood of rheumatoid arthritis.”
These tests give important information. They help doctors plan the next steps in diagnosis and treatment.
Limitations of Blood Testing Alone
Even though blood tests are important, they have their limits. Not everyone with rheumatoid arthritis will have these antibodies. Some healthy people might test positive too.
So, doctors must look at the whole picture. They consider the patient’s symptoms and other tests.
Part of a Comprehensive Diagnostic Approach
Doctors use a mix of tests to diagnose rheumatoid arthritis. They look at blood tests, physical exams, and imaging studies. This way, they can accurately diagnose and plan treatment.
As we learn more about rheumatoid arthritis, using blood tests with other tools is key.
Key diagnostic components include:
- Blood tests to detect autoantibodies and inflammation markers
- Physical examination to assess joint health and function
- Imaging studies to evaluate joint damage and disease progression
By combining these, we get a more accurate diagnosis. This leads to better treatment plans for patients with rheumatoid arthritis.
Anti-CCP Antibody Test: The Gold Standard
The anti-CCP test is a top choice for diagnosing rheumatoid arthritis. It’s known for its high accuracy and specificity. This test has changed how we diagnose rheumatoid arthritis by finding a specific marker for the disease.
Cyclic Citrullinated Peptide Antibodies Explained
Cyclic citrullinated peptide (CCP) antibodies target citrullinated proteins. These proteins are made when arginine turns into citrulline. Finding anti-CCP antibodies is key in diagnosing rheumatoid arthritis.
Key characteristics of anti-CCP antibodies include:
- High specificity for rheumatoid arthritis
- Association with more severe disease progression
- Potential presence years before clinical symptoms appear
How the Anti-CCP Test Works
The anti-CCP test checks for CCP antibodies in the blood. It uses an enzyme-linked immunosorbent assay (ELISA) method. This test is very specific for rheumatoid arthritis, with a specificity of about 96 to 98 percent.
Understanding Anti-CCP Test Results
When you get your anti-CCP test results, it’s important to understand what they mean. A positive result means you have CCP antibodies, which is a strong sign of rheumatoid arthritis. The higher the titer, the more likely you have RA.
Interpretation guidelines:
- A negative result does not rule out RA, even in early stages
- A positive result supports a diagnosis of RA, with symptoms
- High titers suggest a more severe disease
The anti-CCP test is a key tool in diagnosing and managing rheumatoid arthritis. Its high specificity and early detection make it a vital part of the diagnostic process.
Rheumatoid Factor Testing: A Traditional Approach
Rheumatoid factor testing has been key in diagnosing rheumatoid arthritis for years. It checks for rheumatoid factor (RF) in the blood. RF is an antibody found in people with rheumatoid arthritis.
Understanding Rheumatoid Factor
Rheumatoid factor is an antibody found in people with rheumatoid arthritis. It’s not just for RA, though. It can also show up in other autoimmune diseases or infections. Yet, its presence is a big clue for diagnosing RA.
RF Test Procedure and Results
The RF test is a simple blood test. It measures the level of rheumatoid factor in your blood. The results are either a number or positive/negative. A positive result means RF is present, while a negative result means it’s not.
Limitations of RF Testing
Even though the RF test is helpful, it has its downsides. Not everyone with rheumatoid arthritis tests positive for RF. And some people without RA might test positive. So, it’s important to look at RF test results with other tests and criteria.
Combining RF with Anti-CCP for Improved Accuracy
Using the RF test with the anti-CCP antibody test makes diagnosis more accurate. The anti-CCP test is more specific to rheumatoid arthritis than the RF test. Together, they give a clearer picture, helping confirm the diagnosis and spot the disease earlier.
|
Test |
Specificity |
Sensitivity |
|---|---|---|
|
RF Test |
Moderate |
High |
|
Anti-CCP Test |
High |
Moderate |
|
Combined RF and Anti-CCP |
High |
High |
Understanding rheumatoid factor testing and its limits helps healthcare providers make better decisions. Using both RF and anti-CCP tests is a big step forward in diagnosing rheumatoid arthritis.
Inflammation Markers: ESR and CRP Tests
Inflammation markers like ESR and CRP tests are key in tracking rheumatoid arthritis. They show how much inflammation is in the body. This is vital for diagnosing and keeping an eye on the disease.
Understanding Erythrocyte Sedimentation Rate (ESR)
The ESR test shows how fast red blood cells settle in a test tube. It indirectly tells us how much inflammation is in the body. If the ESR is high, it means there’s more inflammation.
We use the ESR test to see if there’s inflammation. It doesn’t pinpoint rheumatoid arthritis, but it helps gauge inflammation levels and track the disease’s activity.
C-Reactive Protein (CRP) Testing
The CRP test checks for C-reactive protein in the blood. This protein is made by the liver when there’s inflammation. High CRP levels mean there’s a lot of inflammation.
CRP testing is great for seeing how severe the inflammation is and if treatment is working. It’s a more direct way to measure inflammation than ESR.
What Elevated Levels Indicate
High ESR and CRP levels show there’s inflammation, a key sign of rheumatoid arthritis. These tests help us understand how active the disease is and if the treatment is effective.
High levels might mean the disease is active and treatment needs to be adjusted. On the other hand, lower levels often show the treatment is working well.
Using Inflammation Markers to Monitor Disease Activity
It’s important to regularly check ESR and CRP levels in managing rheumatoid arthritis. These tests help us see how the disease is changing over time. This helps us make smart decisions about treatment.
By looking at ESR and CRP test results together with clinical assessments, we get a full picture of the disease. This lets us tailor the treatment to what the patient needs.
|
Test |
What It Measures |
Significance in RA |
|---|---|---|
|
ESR |
Rate of red blood cell settlement |
Indirect measure of inflammation |
|
CRP |
Level of C-reactive protein |
Direct measure of inflammation |
How Do Doctors Check for Arthritis: The Complete Diagnostic Process
To find out if you have rheumatoid arthritis, doctors use several steps. They look at your medical history, do a physical check, run lab tests, and use imaging. This detailed method helps them make a correct diagnosis and plan the best treatment.
Initial Assessment and Medical History
The first step is to review your medical history. Doctors ask about your symptoms, how long you’ve had them, and what makes them better or worse. This helps them understand your situation and see if you might have rheumatoid arthritis.
Physical Examination Techniques
Next, a physical exam is key to checking your joints. They look for swelling, redness, warmth, and tenderness. They also check how well your joints move. These signs tell them if you have rheumatoid arthritis and how serious it is.
Laboratory Testing Protocol
Lab tests are very important for confirming rheumatoid arthritis. Tests like the Anti-CCP antibody test and the Rheumatoid Factor (RF) test help. They also use the Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) test to learn more about your condition.
|
Laboratory Test |
Purpose |
|---|---|
|
Anti-CCP Antibody Test |
Detects antibodies against cyclic citrullinated peptide, indicative of RA |
|
Rheumatoid Factor (RF) Test |
Measures the level of rheumatoid factor in the blood |
|
Erythrocyte Sedimentation Rate (ESR) |
Assesses inflammation by measuring the rate of red blood cell sedimentation |
|
C-Reactive Protein (CRP) Test |
Evaluates the level of CRP, a protein produced in response to inflammation |
Imaging Studies and Their Role
Imaging like X-rays, ultrasound, and MRI are also used. They help see joint damage and how the disease is progressing. These images give doctors important information to help decide on treatment.
By combining all these steps, doctors can accurately diagnose rheumatoid arthritis. They then create a treatment plan that’s just right for you.
Beyond Blood Tests: Additional Diagnostic Methods
There are many ways to diagnose and monitor rheumatoid arthritis, not just blood tests. Blood tests show if certain antibodies and inflammation markers are present. Other tests help see how much damage joints have and how active the disease is.
Joint Fluid Analysis
Joint fluid analysis, or arthrocentesis, removes fluid from a joint to check for inflammation or infection. It helps tell if you have rheumatoid arthritis or other conditions like gout or septic arthritis.
Key aspects of joint fluid analysis include:
- Examining the fluid’s appearance, viscosity, and cell count
- Checking for the presence of crystals or microorganisms
- Assessing the fluid’s glucose and protein levels
X-rays and Joint Damage Assessment
X-rays are key for checking joint damage in rheumatoid arthritis. They show bone erosions, joint space narrowing, and other changes caused by the disease.
Benefits of using X-rays include:
- Providing a baseline assessment of joint damage
- Monitoring disease progression over time
- Helping to evaluate the effectiveness of treatment
Advanced Imaging: MRI and Ultrasound
Techniques like MRI and ultrasound give detailed views of joints and tissues. MRI spots early signs of inflammation and damage. Ultrasound is great for seeing inflammation in the synovium and early erosions.
Advantages of MRI and ultrasound include:
- High sensitivity for detecting early disease activity
- Ability to visualize soft tissue inflammation
- Guiding treatment decisions with detailed imaging
Bone Scans and Their Utility
Bone scans use a radioactive material injected into the bloodstream. It shows where bone activity is high, helping find inflammation or damage from rheumatoid arthritis.
Key uses of bone scans include:
- Detecting areas of active bone inflammation
- Assessing the extent of disease spread
- Monitoring response to treatment
Early Detection Through Blood Work: The Window of Opportunity
Blood tests are key in finding rheumatoid arthritis early. This gives doctors a chance to start treatment quickly. Early treatment can change how the disease progresses.
Detecting RA Years Before Symptoms Appear
Studies show that some antibodies linked to RA can be found years before symptoms start. Finding these antibodies early is vital. It lets doctors start treatment before joints are badly damaged.
Benefits of Early Intervention
Starting treatment early in RA can greatly help patients. It can make symptoms less severe, slow the disease, and improve life quality.
The early start of treatment brings many benefits:
- Less joint damage
- Better function
- Higher quality of life
- Best treatment results
Preventing Joint Damage Through Timely Treatment
Starting treatment early is essential to avoid joint damage in RA patients. Using DMARDs early can greatly lower the chance of long-term damage and disability.
|
Outcome |
Early Detection and Treatment |
Delayed Detection and Treatment |
|---|---|---|
|
Joint Damage |
Reduced risk |
Increased risk |
|
Quality of Life |
Improved |
Reduced |
|
Response to Treatment |
Better |
Poorer |
Early detection through blood tests is a big step forward in managing RA. This technology lets doctors act fast. It helps improve patient outcomes.
When Blood Tests Show Negative Results But Symptoms Persist
Rheumatoid arthritis diagnosis gets tricky when blood tests are negative but symptoms keep showing up. This means we need to look at everything carefully. Some patients show clear signs of rheumatoid arthritis but their blood tests, like rheumatoid factor and Anti-CCP antibodies, are negative. This is called seronegative rheumatoid arthritis.
Understanding Seronegative Rheumatoid Arthritis
Seronegative rheumatoid arthritis is when patients have symptoms of rheumatoid arthritis but their blood tests are negative. This makes diagnosing the disease harder because the usual blood tests might not find it.
Key characteristics of seronegative RA include:
- Negative rheumatoid factor and Anti-CCP antibody tests
- Presence of typical RA symptoms such as joint pain and swelling
- Variable disease progression
Alternative Diagnostic Approaches
When blood tests are negative, doctors use other ways to find out if someone has rheumatoid arthritis. These include:
|
Diagnostic Method |
Description |
|---|---|
|
Physical Examination |
A thorough examination of the joints to assess swelling, tenderness, and range of motion. |
|
Imaging Studies |
X-rays, MRI, and ultrasound to evaluate joint damage and inflammation. |
|
Joint Fluid Analysis |
Analysis of synovial fluid to check for signs of inflammation and infection. |
Follow-up Testing and Monitoring Protocols
For patients with seronegative RA, it’s important to keep checking and monitoring the disease. This means regular visits, more blood tests, and watching symptoms closely.
“Regular monitoring is essential to adjust treatment plans according to the disease activity and to prevent long-term joint damage.” –
Rheumatology Expert
We also use inflammation markers like ESR and CRP to keep track of the disease. This helps us adjust treatment plans as needed.
In conclusion, diagnosing rheumatoid arthritis in patients with negative blood tests needs a detailed and careful approach. This includes using other diagnostic methods and keeping a close eye on the disease.
Differential Diagnosis: Distinguishing RA from Other Conditions
It’s important to tell rheumatoid arthritis (RA) apart from other arthritis and autoimmune diseases. This step is key for the right diagnosis and treatment. We’ll look into how to tell RA from other conditions with similar symptoms.
Other Autoimmune Arthritis Conditions
RA isn’t the only disease that affects the joints. Psoriatic arthritis and ankylosing spondylitis also cause joint pain. Psoriatic arthritis is linked to psoriasis, a skin issue with red, scaly patches. Ankylosing spondylitis mainly hits the spine but can also affect other joints.
Getting the right diagnosis means looking at the whole picture. This includes the patient’s overall symptoms and any extra issues.
Osteoarthritis vs. Rheumatoid Arthritis
Osteoarthritis (OA) and rheumatoid arthritis (RA) are two different joint diseases. OA is a wear-and-tear condition, while RA is an autoimmune disease. Knowing the difference is key for the right treatment.
- OA usually affects joints that bear weight and those with past injuries.
- RA often hits both sides of the body and can affect any joint.
- RA is more likely to cause systemic symptoms like fatigue and fever.
Conditions That Mimic RA Symptoms
Some conditions can make RA hard to diagnose. These include infections, other autoimmune diseases, and some cancers. For example, Lyme disease can cause symptoms similar to RA. Other diseases like lupus and gout can also look like RA.
To accurately diagnose RA, a detailed diagnostic process is needed. This includes lab tests and imaging studies.
Understanding differential diagnosis helps doctors give patients the right treatment for their condition.
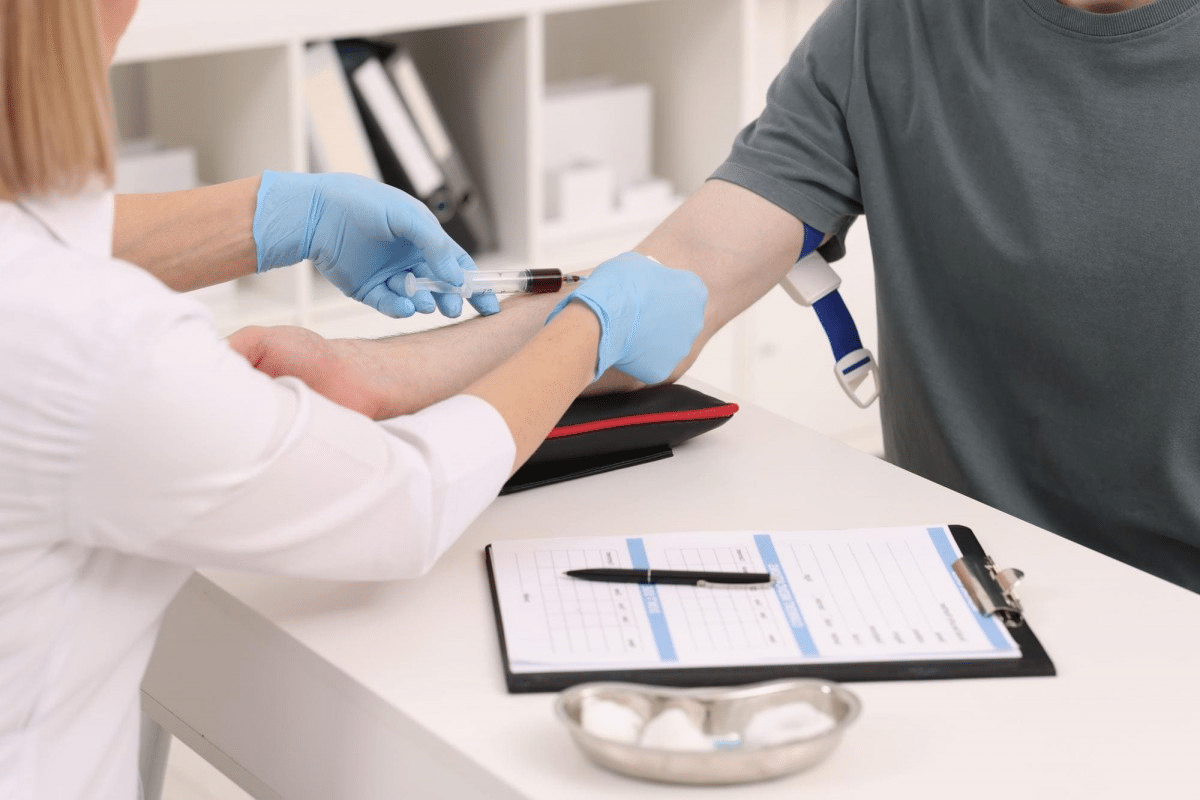
Preparing for Your Rheumatoid Arthritis Blood Test
To get accurate results, it’s key to prepare well for your rheumatoid arthritis blood test. A blood test is vital for diagnosing rheumatoid arthritis. Being ready can make the process easier and less stressful.
What to Expect During Testing
When you get to your blood test, here’s what happens:
- A healthcare professional will clean the area where the blood will be drawn, usually the inside of your elbow.
- A tourniquet may be applied to make your veins more accessible.
- A needle will be inserted into a vein to collect a blood sample.
- The blood sample will be sent to a laboratory for analysis.
Tips for a Smooth Blood Test:
- Stay hydrated to make your veins more accessible.
- Avoid tight clothing that may constrict your arm.
- Be prepared to provide information about any medications you’re taking.
Questions to Ask Your Healthcare Provider
It’s smart to have questions ready for your healthcare provider. Some examples include:
- What is the purpose of the blood test?
- Are there any specific preparations I need to make before the test?
- How long will it take to receive the results?
- What do the results mean, and how will they impact my diagnosis or treatment plan?
Knowing the process and being prepared can reduce anxiety. It ensures you get the most from your blood test.
Understanding Your Test Results
When your blood test results are ready, your healthcare provider will explain them to you. The results may show:
- Rheumatoid factor (RF) levels
- Anti-CCP antibody levels
- Inflammation markers such as ESR or CRP
It’s important to understand your test results. They help decide your next steps in diagnosis and treatment. Your healthcare provider will use the results to:
- Confirm a diagnosis of rheumatoid arthritis
- Rule out other conditions
- Develop a personalized treatment plan
By being prepared and knowing what to expect, you can actively participate in your care. This way, you can work closely with your healthcare provider to manage your condition well.
Conclusion: The Value of Blood Tests in Rheumatoid Arthritis Management
Blood tests are key in diagnosing and managing rheumatoid arthritis (RA). They help spot RA early, leading to better treatment and outcomes. Tests like the Anti-CCP antibody test are very helpful in this area.
Diagnosing RA takes a team effort. It includes looking at medical history, doing physical exams, and running lab tests. Blood tests show how active the disease is and the body’s inflammation levels.
Managing RA well depends on accurate diagnosis and regular checks. Blood tests help doctors create treatment plans that fit each patient. This can stop joint damage and make life better for patients.
Medical research is always moving forward. This means blood tests will play an even bigger role in RA care. Keeping up with new tests and treatments helps patients and doctors work together for the best results.
FAQ
Can a blood test detect rheumatoid arthritis?
Yes, blood tests, like the Anti-CCP test, are key in diagnosing rheumatoid arthritis. They spot specific antibodies and markers of inflammation linked to the condition.
What is the Anti-CCP antibody test?
The Anti-CCP antibody test is a precise test for rheumatoid arthritis. It looks for cyclic citrullinated peptide antibodies in the blood, common in RA patients.
Is there a test for arthritis?
There’s no single test for all arthritis types. But, doctors use blood tests, imaging, and physical exams to diagnose different arthritis forms, including RA.
Can a blood test show rheumatoid arthritis?
Blood tests can show RA by finding specific antibodies and inflammation markers like ESR and CRP.
What does a positive Anti-CCP test result mean?
A positive Anti-CCP test means you have cyclic citrullinated peptide antibodies, common in RA. It suggests you might have RA.
What is rheumatoid factor?
Rheumatoid factor is an antibody found in RA patients’ blood. It’s a traditional test used to diagnose RA.
How do doctors check for arthritis?
Doctors use a detailed approach to diagnose arthritis. This includes medical history, physical exams, blood tests, and imaging studies.
What is seronegative rheumatoid arthritis?
Seronegative RA is when patients show RA symptoms but test negative for certain antibodies. Doctors use other tests and follow-ups to diagnose it.
How can inflammation markers help in managing RA?
Inflammation markers like ESR and CRP help track RA inflammation. They show how active the disease is and if treatment is working.
What is the importance of early detection of rheumatoid arthritis?
Early RA detection through blood tests and other methods offers a chance for early treatment. This can prevent joint damage and improve outcomes.
How should I prepare for a rheumatoid arthritis blood test?
To prepare for a RA blood test, follow your doctor’s instructions. Be ready to ask about the test and its results.
Can rheumatoid arthritis be diagnosed with a blood test alone?
While blood tests are important, diagnosing RA requires a combination of clinical assessment, medical history, physical exams, and lab tests.
What other diagnostic methods are used beside blood tests?
Other methods for diagnosing RA include joint fluid analysis, X-rays, MRI, ultrasound, and bone scans.
How do imaging studies contribute to diagnosing RA?
Imaging studies like X-rays, MRI, and ultrasound help check joint damage and disease progression. They also show if treatment is working.









