Have you seen blood vessels that look unusual behind your eyes? Or have you noticed changes in your vision that worry you? Dilated retrobulbar and episcleral vessels can be signs of serious health issues. These need to be checked by a doctor and treated with care enlarged blood vessels behind the eye.
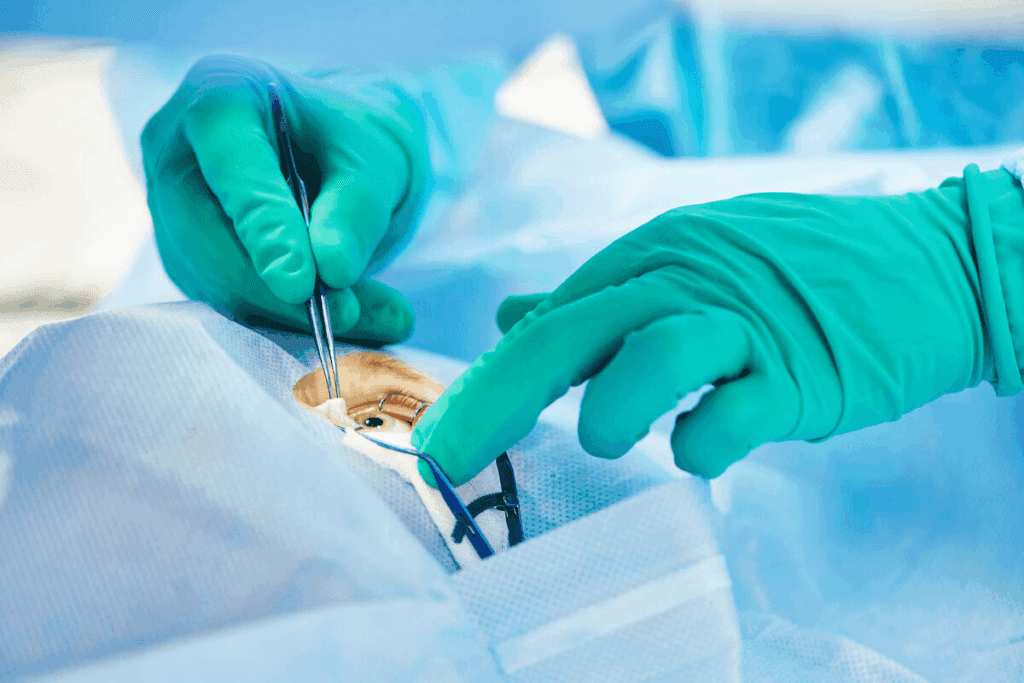
At Liv Hospital, we have top-notch eye doctors. They can find and fix problems that affect your eyes. One big issue is diabetic retinopathy. It’s a diabetes problem that harms the blood vessels in the retina, the back part of the eye.
It’s key to know why eye blood vessels get big. This helps keep your vision and eye health safe. Always see a doctor to find out why this is happening.
Key Takeaways
- Dilated retrobulbar and episcleral vessels can be a sign of underlying health conditions.
- Diabetic retinopathy is a complication of diabetes that affects the eyes.
- Professional evaluation is critical for figuring out why blood vessels get big.
- Good eye care is vital for keeping your vision and eye health in top shape.
- Liv Hospital offers world-class eye care.
Understanding Eye Anatomy and Blood Vessels

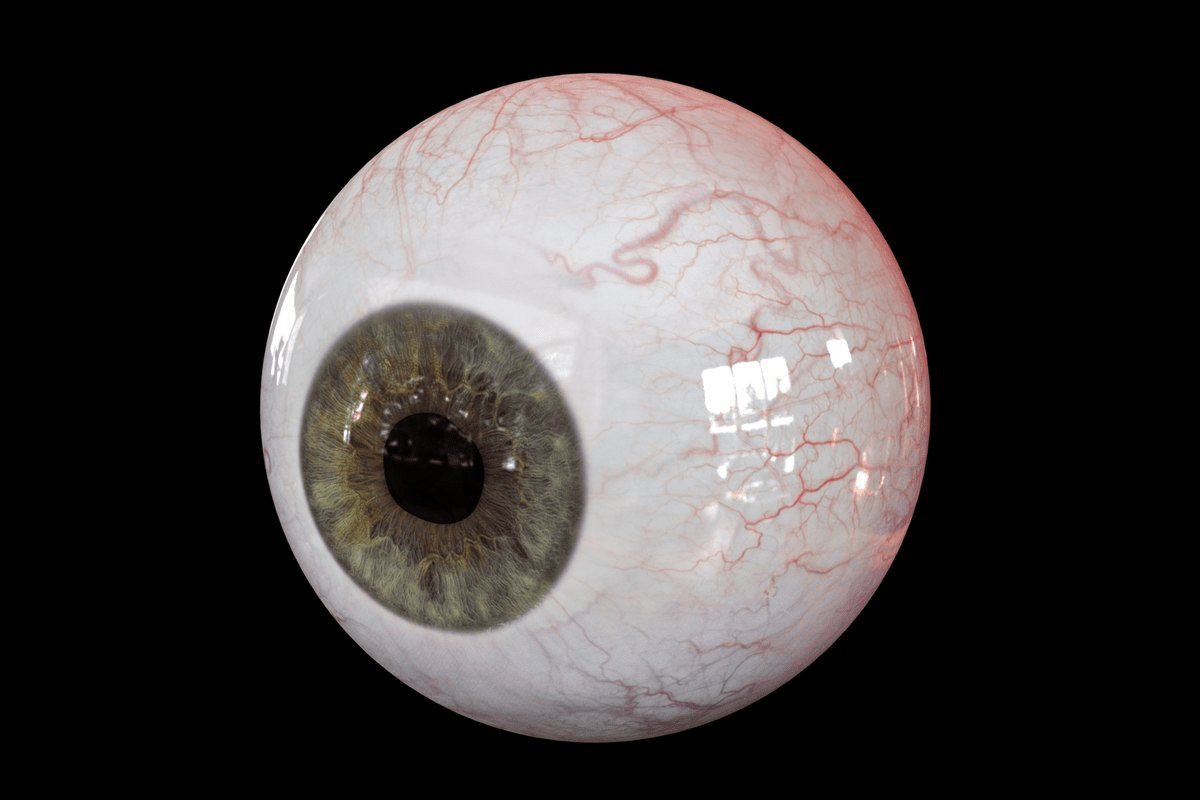
To understand why blood vessels behind the eye get big, we need to know about the eye’s structure and blood vessels. The eye is a complex organ. Its blood vessels are key to keeping it healthy.
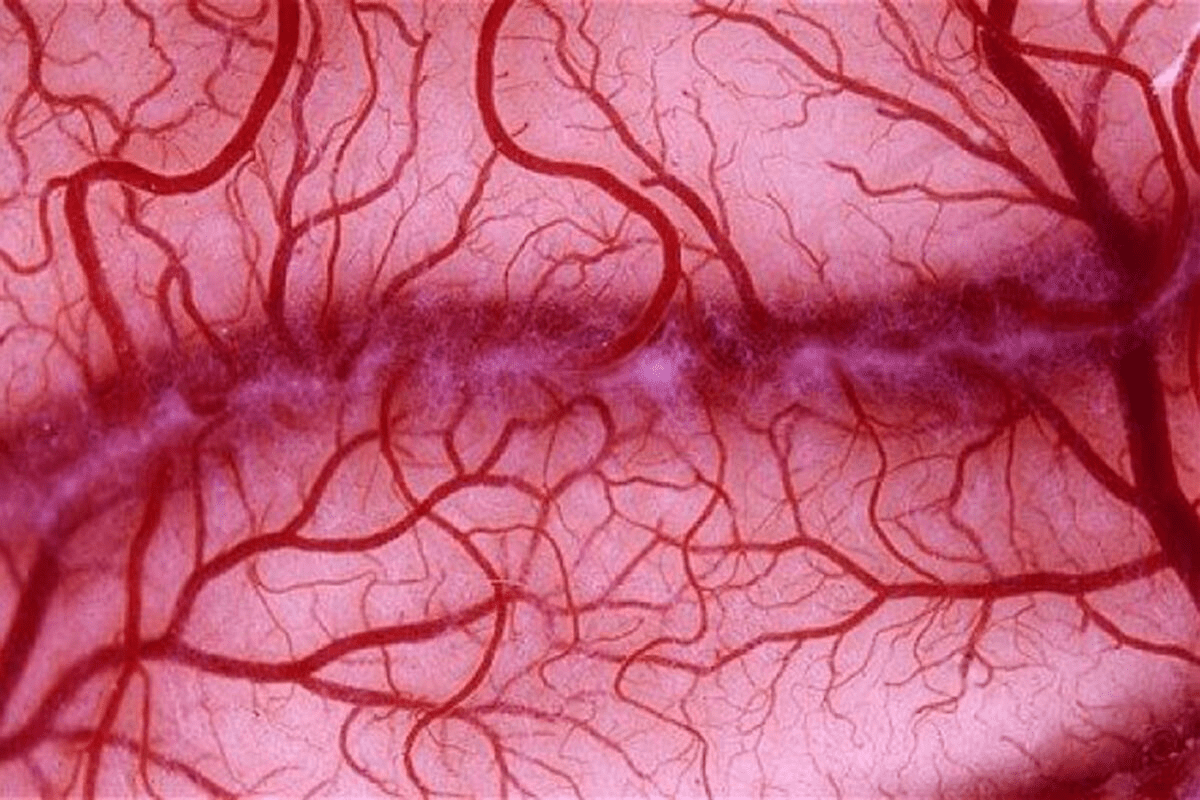
Normal Structure of Retinal Blood Vessels
The retina gets its blood from a network of vessels. Retinal blood vessels carry oxygen and nutrients to the retina. These vessels have a specific pattern and size.
The retinal arteries and veins feed the inner retina. The central retinal artery splits into smaller arterioles. These arterioles lead to capillaries that feed the retina.
Function of Blood Vessels in the Eye
Blood vessels in the eye do several important jobs. They bring oxygen and nutrients to the retina. They also take away waste and help control the eye’s internal environment.
- Delivering oxygen and nutrients to the retina
- Removing waste products from the retina
- Regulating blood pressure within the eye
Blood Supply to the Retina and Optic Nerve
The retina and optic nerve need blood to work right. The blood supply to the retina mainly comes from the central retinal artery. The optic nerve gets blood from the central retinal artery and the short posterior ciliary arteries.
- The central retinal artery supplies the inner layers of the retina.
- The short posterior ciliary arteries supply the optic nerve head.
Recognizing Enlarged Blood Vessels Behind the Eye
It’s important to know the signs of enlarged blood vessels in the eye. We’ll show you how to spot them and what symptoms to look out for. This will help you know when to see a doctor.
Visual Appearance and Common Symptoms
Enlarged blood vessels can cause different symptoms. You might see spots or dark strings floating in your vision. You could also have blurred vision or changes in your field of sight.
In some cases, people see dark or empty areas in their vision or even lose vision. These signs can mean there’s a problem that needs fixing.
Diabetic retinopathy is a condition where blood vessels in the retina get bigger. It can cause:
- Floaters or dark strings in your vision
- Blurred vision
- Fluctuations in vision
- Dark or empty areas in your field of vision
- Vision loss
Difference Between Normal and Abnormal Vessels
It’s key to tell normal from abnormal blood vessels in the eye. Normal vessels are the same size and follow a pattern. But abnormal vessels are bigger, twisted, or don’t follow a pattern.
They might leak blood or fluid, causing vision problems. These issues can be linked to diabetic retinopathy, hypertensive retinopathy, or retinal vein occlusions. Knowing the difference helps find the cause of enlarged vessels.
When to Seek Medical Attention
If you notice symptoms like sudden vision changes or more floaters, see a doctor right away. Early treatment can make a big difference in many eye conditions.
Make an appointment for a full eye check if your vision changes. An eye doctor can check your blood vessels and tell you what to do next.
Diabetes and Diabetic Retinopathy
Diabetic retinopathy is a serious eye condition that happens in people with diabetes. It shows how important it is to manage diabetes well. This condition affects the blood vessels in the retina, which can lead to vision problems if not treated.
Impact on Eye Blood Vessels
Diabetes really hurts the blood vessels in the eye. High blood sugar can damage these vessels over time. This can make them bleed or leak fluid, causing vision problems or even blindness. The damage to these blood vessels is a hallmark of diabetic retinopathy.
Stages of Diabetic Retinopathy
Diabetic retinopathy goes through several stages:
- Mild Nonproliferative Retinopathy: Early stage where some retinal blood vessels begin to swell.
- Moderate Nonproliferative Retinopathy: Some blood vessels become blocked, leading to reduced blood flow.
- Severe Nonproliferative Retinopathy: Many blood vessels are blocked, depriving the retina of its blood supply.
- Proliferative Retinopathy: The most advanced stage, where the retina starts growing new, fragile blood vessels.
Risk Factors and Complications
Several factors increase the risk of developing diabetic retinopathy, including:
- Duration of diabetes: The longer someone has diabetes, the higher the risk.
- Poor blood sugar control: High blood sugar levels exacerbate the condition.
- High blood pressure and high cholesterol: These conditions can further strain the blood vessels.
If left untreated, diabetic retinopathy can lead to severe complications, including vision loss and blindness. Regular eye exams are key for early detection and management.
High Blood Pressure and Hypertensive Retinopathy
High blood pressure can damage the blood vessels in the retina. This is called hypertensive retinopathy. It’s a big worry for people with high blood pressure because it can cause vision problems and even blindness if not treated.
Blood Pressure’s Impact on Eye Vessels
High blood pressure can harm the blood vessels in the retina. The retina needs these vessels to get oxygen and nutrients. When blood pressure goes up, these vessels can get narrow, leak, or even block, causing problems.
The effects of high blood pressure on retinal vessels can be seen in several ways:
- Narrowing of the arterioles, which can reduce blood flow to the retina
- Leakage of blood or fluid from damaged vessels, potentially causing retinal edema
- Blockage of larger vessels, leading to retinal ischemia or infarction
Grading of Hypertensive Retinopathy
Hypertensive retinopathy is graded using the Keith-Wagener-Barker system. It has four stages, from mild to severe. The stages show how much the retina has changed.
This grading helps doctors know how bad the condition is. It helps them decide the best treatment. Knowing the stage is key to predicting how well someone will do.
Complications of Untreated Hypertension
If hypertensive retinopathy is not treated, it can cause serious problems. These include:
- Vision loss due to retinal damage or ischemia
- Retinal vein occlusions, which can further compromise vision
- Optic neuropathy, potentially resulting in irreversible vision loss
Early detection and management of high blood pressure are critical to preventing these complications and preserving vision. By controlling hypertension and watching the retina closely, people can lower their risk of severe hypertensive retinopathy.
Retinal Vein and Artery Occlusions
Occlusions in the retinal veins or arteries can cause sudden and significant changes in vision. These blockages disrupt normal blood flow to the retina. This can lead to severe vision loss if left untreated.
Causes of Blood Vessel Blockages
Retinal vein occlusions happen when a vein in the retina gets blocked. This blockage can cause fluid buildup and swelling in the retina, known as macular edema. High blood pressure, diabetes, and glaucoma are common causes.
Artery occlusions, on the other hand, are often caused by emboli or thrombi that obstruct the arterial flow. These conditions require immediate medical attention to prevent permanent vision loss.
Macular Edema Development
Macular edema is a common complication of retinal vein occlusions. When the vein is blocked, fluid can leak into the macula. This causes it to thicken and swell, leading to distorted vision and, if severe, significant vision loss.
We diagnose macular edema using advanced imaging techniques such as optical coherence tomography (OCT). Treatment options include anti-vascular endothelial growth factor (anti-VEGF) injections and corticosteroids.
Differences Between Artery and Vein Occlusions
The main difference between artery and vein occlusions lies in their presentation and prognosis. Artery occlusions typically present with sudden, painless loss of vision. Vein occlusions may cause gradual vision loss due to macular edema.
Understanding these differences is key to determining the right treatment approach. Artery occlusions often require immediate intervention to restore blood flow. Vein occlusions may be managed with treatments aimed at reducing edema and preventing further complications.
Treatment Options and Prognosis
Treatment for retinal vein and artery occlusions varies depending on the severity and type of occlusion. For vein occlusions, anti-VEGF injections and corticosteroids are commonly used to reduce macular edema.
Treatment | Description | Prognosis |
Anti-VEGF Injections | Reduces vascular leakage and edema | Improves vision in many cases |
Corticosteroids | Decreases inflammation and edema | Can improve vision, but may have side effects |
Laser Photocoagulation | Reduces edema and prevents further vision loss | May stabilize or improve vision |
For artery occlusions, immediate medical attention is critical. Treatment may involve thrombolysis or other interventions to restore blood flow.
We understand that dealing with retinal vein and artery occlusions can be challenging. By understanding the causes, symptoms, and treatment options, patients can better navigate these complex conditions. This helps them make informed decisions about their care.
Enlarged Blood Vessels Behind the Eye: Vascular Malformations
It’s key to know about vascular malformations to treat enlarged blood vessels behind the eye. These malformations are abnormal blood vessel formations in the body, including the eye.
They can cause vision problems and even vision loss if not treated. We’ll look at three main types: arteriovenous malformations (AVMs), carotid-cavernous sinus fistulas, and Sturge-Weber syndrome.
Arteriovenous Malformations (AVMs)
AVMs are abnormal connections between arteries and veins. In the eye, they can cause enlarged blood vessels. This is because of the abnormal blood flow.
Symptoms include vision problems, eye pain, and vision loss in severe cases. Doctors use angiography to see the abnormal blood vessels.
Carotid-Cavernous Sinus Fistulas
Carotid-cavernous sinus fistulas connect the carotid artery to the cavernous sinus. This can cause enlarged blood vessels behind the eye. It’s due to increased blood flow.
Common symptoms are bulging eyes, double vision, and eye pressure. Doctors use MRI or CT angiography to find the fistula.
Sturge-Weber Syndrome
Sturge-Weber syndrome is rare. It has a port-wine stain on the face and eye problems. One problem is enlarged blood vessels behind the eye.
It can also cause glaucoma and vision loss. Doctors diagnose it by looking at symptoms and using imaging studies.
Early diagnosis and treatment are vital. They help avoid complications and keep vision. Knowing about these conditions helps us manage and treat them better.
Inflammatory and Infectious Causes
Enlarged blood vessels behind the eye can signal inflammation or infection. These issues can lead to various eye problems. If not treated quickly, they can cause serious complications.
Conjunctivitis and Eye Inflammation
Conjunctivitis is an inflammation of the thin membrane covering the eye and eyelids. It makes blood vessels in the eye swell and become visible. It can be caused by infection, allergies, or chemical exposure. Symptoms include redness, itching, and discharge.
Eye inflammation, or uveitis, affects the middle layer of the eye. It can be due to infection, autoimmune disorders, or trauma. If not managed, it can lead to vision loss.
Orbital Cellulitis
Orbital cellulitis is an infection of the eye’s surrounding tissues. It causes swelling, redness, and pain. It’s a serious condition that needs immediate medical attention to avoid vision loss or life-threatening issues.
Autoimmune Conditions Affecting Eye Vessels
Autoimmune conditions happen when the body attacks its own tissues. Several diseases can affect eye vessels, causing inflammation and enlargement. Examples include:
- Rheumatoid arthritis
- Lupus
- Sarcoidosis
These conditions can cause eye symptoms like redness, pain, and vision problems. It’s important to manage the underlying condition to prevent eye issues.
Condition | Symptoms | Complications |
Conjunctivitis | Redness, itching, discharge | Vision problems if untreated |
Orbital Cellulitis | Swelling, redness, pain around the eye | Vision loss, life-threatening conditions |
Uveitis | Eye pain, vision problems | Vision loss if not properly managed |
Thyroid-Related Eye Disease and Orbital Conditions
Thyroid-related eye disease is complex, with causes, symptoms, and treatments to know. It’s often linked to Graves’ disease and can cause eye problems like enlarged blood vessels. We’ll look at Graves’ ophthalmopathy, orbital hemorrhage, and vascular changes in thyroid eye disease.
Graves’ Ophthalmopathy Mechanism
Graves’ ophthalmopathy is an autoimmune condition that causes eye inflammation and swelling. The exact cause is not fully understood, but it’s closely tied to Graves’ disease, which affects the thyroid gland. This inflammation can make the eyeballs bulge out, cause double vision, and other symptoms.
Orbital Hemorrhage
Orbital hemorrhage is bleeding in the orbit, a complication of thyroid eye disease. It can increase pressure in the orbit, damaging the optic nerve and other important structures. Prompt medical attention is vital to manage orbital hemorrhage and avoid vision loss.
Vascular Changes in Thyroid Eye Disease
Vascular changes are key in thyroid eye disease, with enlarged blood vessels being a common sign. These changes come from the inflammation and swelling of Graves’ ophthalmopathy. Understanding these vascular changes is key to finding effective treatments.
Thyroid-related eye disease can greatly affect a patient’s life. By grasping the underlying causes and symptoms, we can offer better care and support.
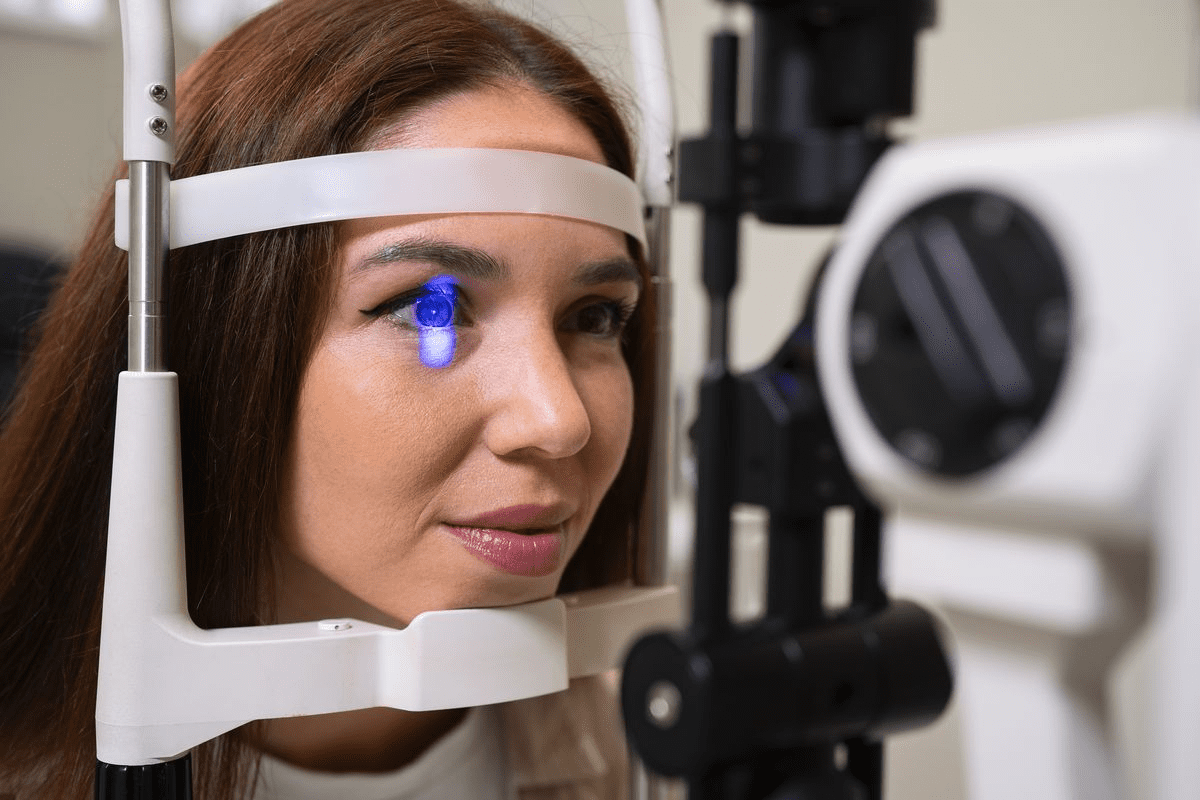
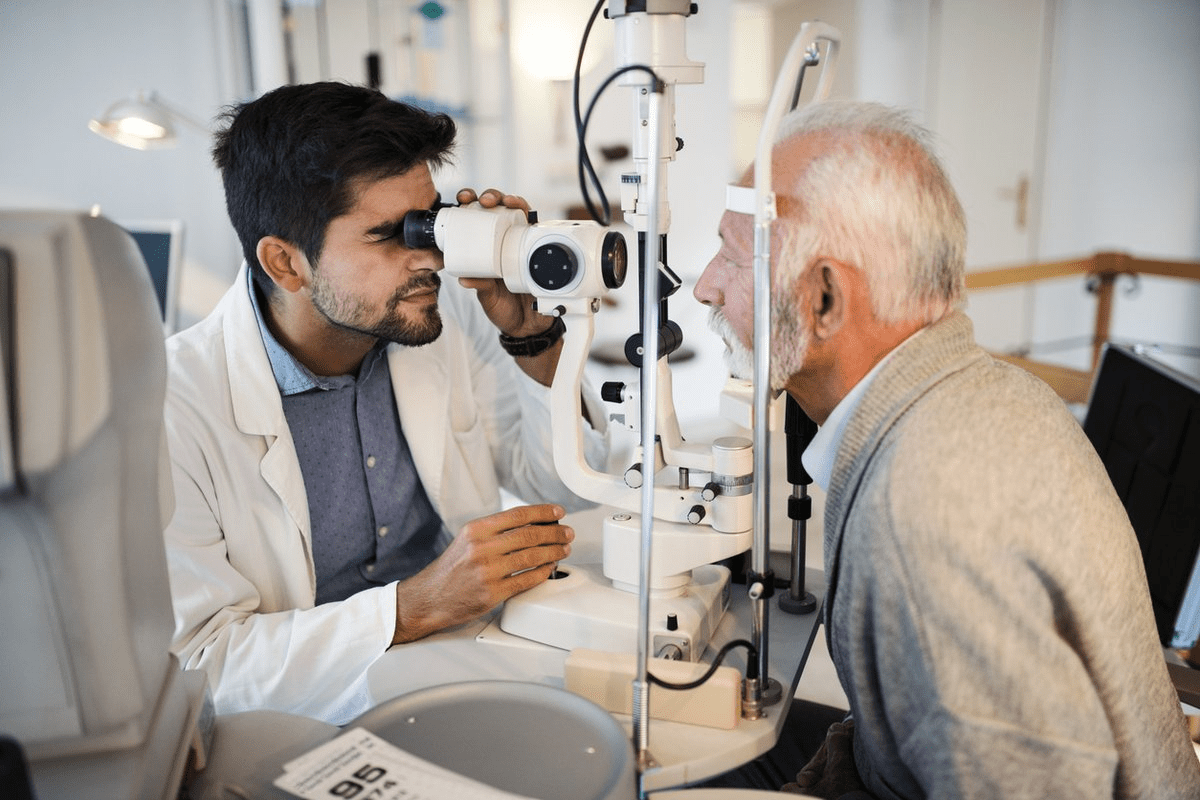
Diagnosis and Evaluation Methods
Diagnosing enlarged blood vessels behind the eye requires a detailed approach. This includes both traditional methods and the latest imaging technologies. Accurate diagnosis is key to managing these blood vessels. It helps doctors find the cause and plan the best treatment.
Comprehensive Eye Examination Techniques
A thorough eye exam is the first step. It includes:
- Visual acuity tests to check vision sharpness
- Fundus examination to see the retina and blood vessels
- Tonometry to measure eye pressure
In the fundus exam, doctors can see the blood vessels behind the eye. They look for signs like dilation or hemorrhages. A study found that a detailed fundus exam is vital for spotting retinal vascular diseases.
“The state of the retinal vessels can provide valuable insights into the overall health of the patient.”
Medical Expert, Ophthalmologist
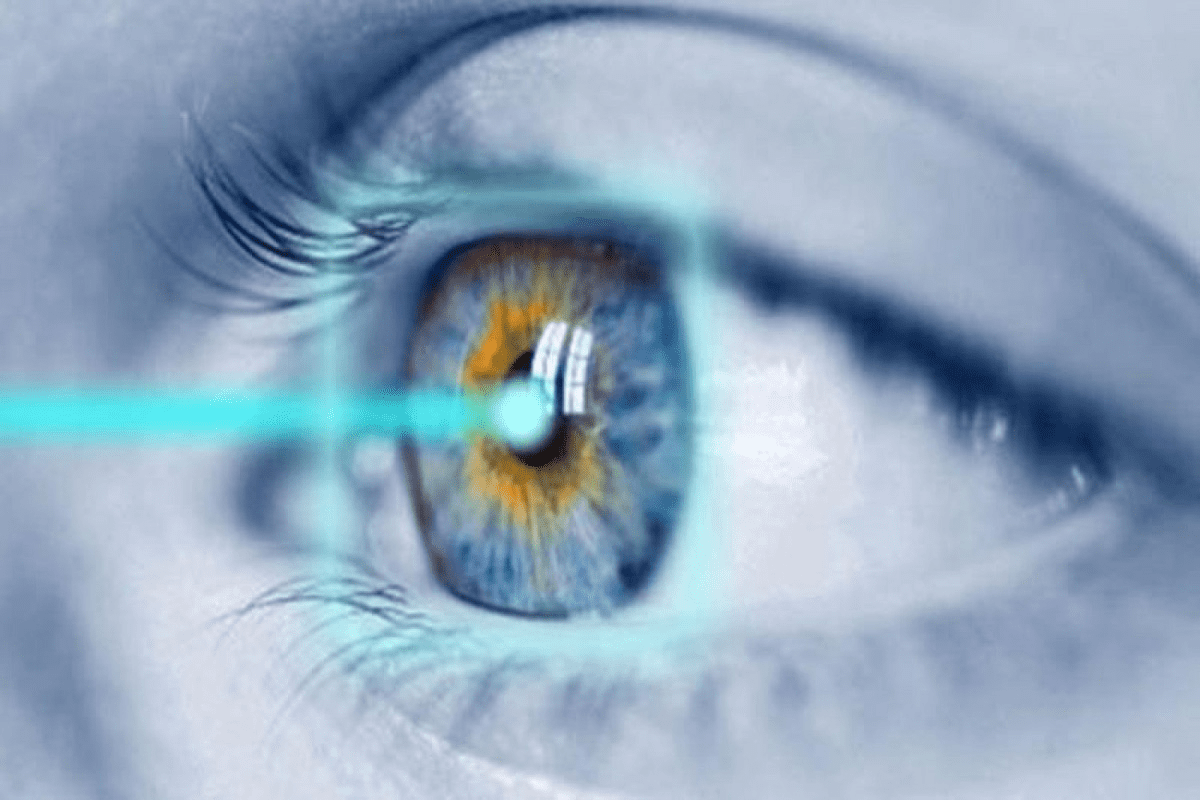
Advanced Imaging Studies
Advanced imaging is key for diagnosing blood vessel issues. Techniques like Optical Coherence Tomography (OCT) and fluorescein angiography give detailed views of the retinal vasculature.
Imaging Technique | Description | Clinical Utility |
Optical Coherence Tomography (OCT) | Non-invasive imaging using low-coherence interferometry | Detailed cross-sectional images of retinal layers and vessels |
Fluorescein Angiography | Dye-based imaging to visualize retinal vascular structure | Identifies vascular leakage, occlusions, and neovascularization |
Laboratory Tests and Systemic Evaluation
Eye exams are just part of the story. Lab tests and systemic checks are also vital. They help find systemic conditions that might cause blood vessel issues. This includes:
- Blood glucose tests to check for diabetes
- Blood pressure monitoring for hypertension
- Lipid profiles to check for dyslipidemia
By using eye exams, imaging, and lab tests, doctors can accurately diagnose blood vessel issues. They can then create a treatment plan that fits each patient’s needs.
Conclusion: Managing and Preventing Enlarged Eye Blood Vessels
Managing and preventing enlarged eye blood vessels needs a full plan. This plan includes lifestyle changes, medical care, and keeping an eye on your health.
To stop diabetic retinopathy, manage your diabetes well. Keep an eye on your blood sugar and get regular eye checks. High blood pressure can also be controlled to prevent hypertensive retinopathy.
Knowing why and how to spot enlarged eye blood vessels is key. This includes noticing squiggly veins in your eyes. Taking action early can help protect your vision.
Getting regular eye exams and acting fast when needed is vital. It helps avoid serious problems and keeps your eyes healthy. We suggest working with your doctor to create a plan for your eye health.
Being proactive and well-informed can lower your risk of losing your vision. It helps keep your eyes in the best shape possible.
FAQ
What are enlarged blood vessels behind the eye a sign of?
Enlarged blood vessels behind the eye can signal many health issues. These include diabetic retinopathy, hypertensive retinopathy, and retinal vein or artery occlusions. They can also point to vascular malformations, inflammatory or infectious causes, and thyroid-related eye disease.
How do diabetes and high blood pressure affect the blood vessels in the eye?
Diabetes can lead to diabetic retinopathy, damaging the retina’s blood vessels. High blood pressure, on the other hand, can cause hypertensive retinopathy. This results in narrowed or damaged blood vessels in the eye.
What are the symptoms of enlarged blood vessels behind the eye?
Symptoms include blurred vision, double vision, eye pain, redness, or swelling. Some cases may not show any symptoms at all.
What is diabetic retinopathy, and how does it progress?
Diabetic retinopathy damages the retina’s blood vessels due to diabetes. It progresses from mild non-proliferative to proliferative diabetic retinopathy.
How does high blood pressure affect the blood vessels in the eye?
High blood pressure can lead to hypertensive retinopathy. This causes narrowed or damaged blood vessels. It can result in vision problems or even blindness if not treated.
What are retinal vein and artery occlusions, and how are they treated?
Retinal vein and artery occlusions block blood vessels in the retina. This can cause vision loss. Treatment depends on the severity and type of occlusion.
What are vascular malformations, and how do they affect the eye?
Vascular malformations, like arteriovenous malformations or carotid-cavernous sinus fistulas, cause enlarged blood vessels behind the eye. They can lead to vision problems or other complications.
How is thyroid-related eye disease associated with enlarged blood vessels behind the eye?
Thyroid-related eye disease, such as Graves’ ophthalmopathy, causes inflammation and swelling. This can lead to enlarged blood vessels.
What diagnostic methods are used to evaluate enlarged blood vessels behind the eye?
To evaluate enlarged blood vessels, doctors use eye exams, advanced imaging like optical coherence tomography (OCT), and lab tests. These help diagnose underlying conditions.
Can lifestyle changes help prevent or manage enlarged blood vessels behind the eye?
Yes, a healthy lifestyle can help. This includes managing diabetes and high blood pressure, not smoking, and regular eye check-ups. These actions can prevent or manage enlarged blood vessels.
What are squiggly eye veins, and are they a concern?
Squiggly eye veins, or tortuous vessels, can indicate conditions like diabetic retinopathy or hypertensive retinopathy. They should be checked by an eye care professional.
Can low blood pressure cause vision problems?
Low blood pressure usually doesn’t cause vision problems. But, it can be a concern for some people, mainly those with underlying conditions.
How can I prevent complications from enlarged blood vessels behind the eye?
To prevent complications, monitor your condition closely, manage your health, and make lifestyle changes. A healthy diet and regular exercise are key.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4975428/