What is prostate brachytherapy? Learn how this form of internal radiation is delivered via seeds to treat localized prostate cancer.
Men with localized prostate cancer have a new treatment option: brachytherapy. This method involves putting radioactive seeds or temporary sources into the prostate gland. It kills cancer cells.
We use advanced ultrasound technology to guide this procedure. This ensures the radiation goes exactly where it needs to. It helps protect healthy tissues around the prostate, reducing side effects and improving quality of life.
Brachytherapy is very effective in treating prostate cancer. It’s a reliable choice for those looking for a good cure. Our team of experts is here to support you with top-notch care.
Key Takeaways
- Brachytherapy is a minimally invasive radiation therapy for localized prostate cancer.
- Radioactive seeds or temporary sources are implanted directly into the prostate gland.
- Advanced ultrasound technology guides the procedure for precise radiation delivery.
- This treatment minimizes damage to surrounding healthy tissues, reducing side effects.
- Brachytherapy offers exceptional cure rates and superior quality of life outcomes.
Understanding Prostate Cancer and Treatment Options
Prostate cancer treatment has changed a lot, giving patients many choices. These choices depend on the patient’s needs and the cancer’s type. It’s key to know about prostate cancer, its commonness, its effects, and the treatments available.
The Prevalence and Impact of Prostate Cancer
Prostate cancer is a big problem for men, mainly in rich countries. It’s a top cancer for men. It affects more than just health, touching on life quality, mental health, and social life.
Overview of Available Treatment Approaches
There are many ways to treat prostate cancer. Each method is chosen based on the patient’s cancer stage, health, and what they prefer. The main options are surgery, external beam radiation therapy (EBRT), and brachytherapy. Each has its good points and possible downsides.
Treatment Approach | Description | Potential Side Effects |
Surgery | Removal of the prostate gland | Incontinence, Impotence |
External Beam Radiation Therapy (EBRT) | High-energy beams targeting cancer cells | Fatigue, Urinary issues |
Brachytherapy | Radioactive seeds implanted near cancer cells | Urinary frequency, Erectile dysfunction |
It’s important for patients and doctors to know about prostate cancer and its treatments. By looking at the good and bad of each option, people can choose the best care for themselves.
What Is Prostate Brachytherapy?
Prostate brachytherapy is a treatment for prostate cancer. It involves placing small radioactive seeds in the prostate. This method targets the tumor with high doses of radiation, protecting healthy tissues nearby.
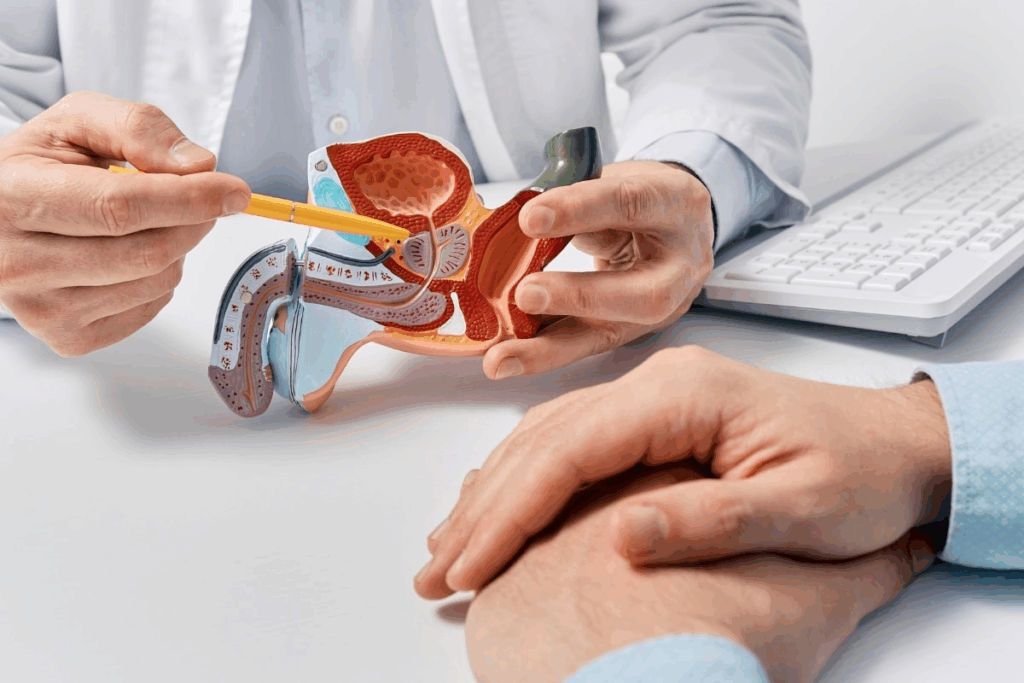
Definition and Basic Principles
Brachytherapy comes from the Greek word “brachios,” meaning “short distance.” It’s a radiation therapy where a source is placed inside or next to the tumor. For prostate cancer, it means putting radioactive materials right in the prostate gland.
The goal is to kill cancer cells with radiation. At the same time, it tries to keep healthy tissue safe. There are two types of implants: permanent and temporary. Permanent implants use small seeds that stay in the prostate for months. Temporary implants are removed after a short time.
History and Development of the Procedure
Brachytherapy started in the early 20th century, after Marie Curie found radium in 1898. It was first used to treat cancers by placing radium in tumors. The use of brachytherapy for prostate cancer began in the 1960s and 1970s, with early methods using radioactive gold grains.
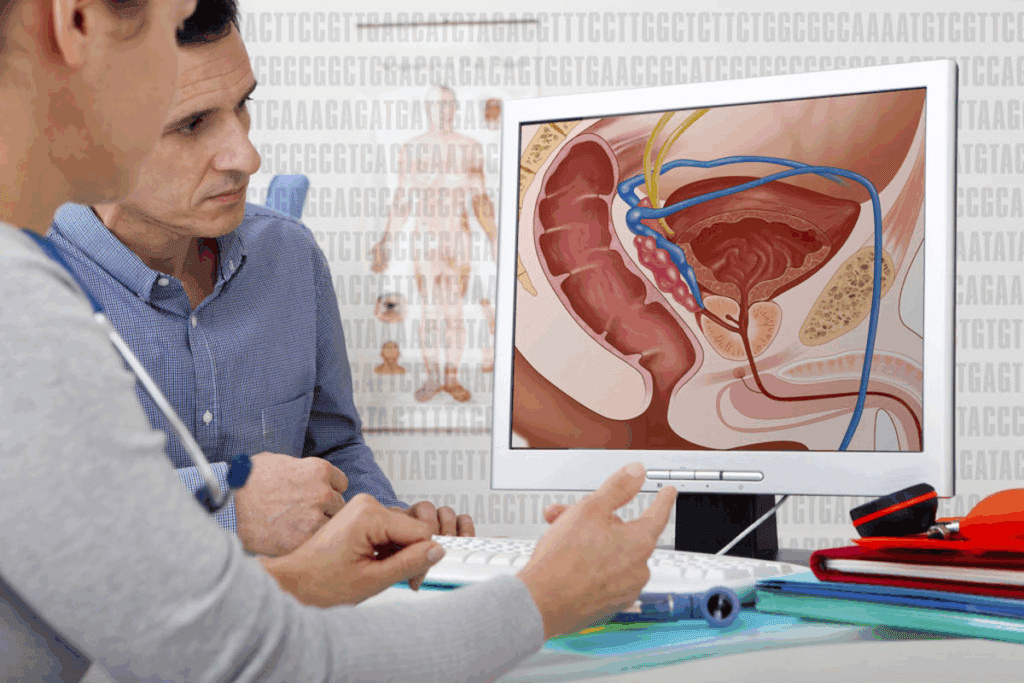
Technology and imaging have made brachytherapy for prostate cancer much better. The 1980s saw the use of transrectal ultrasound for better seed placement. Now, prostate brachytherapy is a key treatment for localized prostate cancer. It’s a less invasive option compared to surgery or external beam radiation therapy.
How Prostate Brachytherapy Works
In prostate brachytherapy, radiation is placed inside the cancer area. This way, healthy tissue around it is not harmed. It lets a lot of radiation go straight to the tumor, making treatment more effective.
Radiation Delivery Mechanism
The method uses radioactive seeds or sources placed in the prostate gland. These seeds kill cancer cells by stopping them from growing. They are put in with a template-guided insertion technique for the best placement.
The process is guided by ultrasound. This lets doctors see the prostate and tissues clearly. It helps place the seeds exactly where they need to be, protecting healthy areas.
Targeting Cancer Cells While Sparing Healthy Tissue
Prostate brachytherapy is great because it hits cancer cells right on target. It also keeps healthy tissue safe, like the rectum and bladder. This careful approach helps avoid side effects and keeps quality of life high.
The radioactive seeds give out radiation at a set rate. This ensures the tumor gets the right amount. As time goes on, the seeds stop giving off radiation. This method is very effective for treating prostate cancer, mainly for those with localized disease.
Knowing how prostate brachytherapy works helps patients make better choices. It lets them talk to their doctors about the best treatment for them.
Types of Prostate Brachytherapy
There are two main types of prostate brachytherapy. Each has its own way of treating cancer. Knowing the differences helps doctors choose the best treatment for each patient.
Low-Dose-Rate (LDR) Brachytherapy
LDR brachytherapy means tiny radioactive seeds are put into the prostate. These seeds give off low doses of radiation for months. This method targets the tumor well, keeping healthy tissues safe.
Doctors use special imaging to place the seeds exactly right. The seeds are tiny and don’t cause harm or discomfort. It’s often used for patients with low to intermediate-risk cancer.
High-Dose-Rate (HDR) Brachytherapy
HDR brachytherapy uses catheters in the prostate for a short, high dose of radiation. This method gives a strong dose to the tumor, but not to nearby tissues. It’s often paired with external beam radiation for high-risk cancer.
A remote afterloader controls the radiation in HDR brachytherapy. This technology lets doctors control the dose precisely, making treatment more effective. HDR is great for complex treatment plans.
Both LDR and HDR brachytherapy have their own strengths. The choice depends on the patient’s cancer stage and health. Understanding these differences helps doctors pick the best treatment.
The Prostate Brachytherapy Procedure Step by Step
Men with prostate cancer can feel better knowing about brachytherapy. It’s a treatment that uses radiation to fight cancer. The process involves several key steps to target the cancer while protecting healthy tissues.
Pre-Procedure Preparation and Planning
Before starting, a lot of planning is needed. This includes:
- Ultrasound or MRI scans to map the prostate and nearby areas.
- Planning the radiation dose and how it will spread to cover the cancer.
- Picking the right radioactive sources and where to place them in the prostate.
Getting ready for brachytherapy is key to its success. A team of doctors and experts work together to create a treatment plan just for you.
Ultrasound-Guided Implementation
During the treatment, ultrasound guidance is used. This means:
- An ultrasound probe is put into the rectum to see the prostate live.
- A template grid helps guide needles with radioactive sources into the prostate.
- The placement of the seeds is watched closely to match the plan.
Template-Guided Insertion Techniques
The template-guided technique ensures the seeds are placed right. This method includes:
- A grid template is placed against the patient’s perineum.
- Needles are inserted through the grid into the prostate at set points.
- The radioactive sources are then placed in the prostate as planned.
Post-Implantation Imaging and Verification
After the treatment, post-implantation imaging is done. This is to check if the seeds are in the right place and how well the treatment is going. This might involve:
- CT or MRI scans to see where the seeds are.
- Calculations to make sure the right dose of radiation is being given.
By following these steps, brachytherapy can be done with great precision. This helps ensure the treatment works well and reduces side effects.
Candidates for Prostate Brachytherapy
Choosing the right candidates for prostate brachytherapy is complex. It depends on the patient’s health and the cancer’s type. This treatment is specialized for prostate cancer.
Ideal Patient Profiles
Men with localized prostate cancer are often the best fit for brachytherapy. The cancer must stay within the prostate. The patient’s health also matters a lot.
Age, prostate size, and cancer stage are key factors. A low to intermediate risk of cancer coming back is also important. Those avoiding other treatments might also be good candidates.
Risk Group Classifications
How risky the cancer is affects brachytherapy choices. Patients are grouped by PSA level, Gleason score, and stage. Low to intermediate risk groups usually get brachytherapy.
Risk Group | PSA Level | Gleason Score | Clinical Stage |
Low | < 10 ng/mL | ≤ 6 | T1-T2a |
Intermediate | 10-20 ng/mL | 7 | T2b-T2c |
High | > 20 ng/mL | 8-10 | T3-T4 |
Contraindications and Limitations
Brachytherapy works well for many prostate cancer patients. But, there are limits. Large prostate, urinary issues, or certain health problems might rule it out.
Those with cancer spread or high risk of recurrence might need other treatments. A doctor’s evaluation is key to see if brachytherapy is right.
Combined Therapy Approaches
Using combined modality therapy in prostate cancer treatment is a big step forward. It allows us to tailor treatments to each patient’s needs. This could lead to better results.
Brachytherapy with External Beam Radiation
For patients with intermediate or high-risk prostate cancer, we use brachytherapy and external beam radiation therapy (EBRT together. This method delivers high doses of radiation directly to the tumor. It also treats any cancer that might have spread around the prostate.
This combination boosts the treatment’s effectiveness. Brachytherapy gives a high dose to the prostate. EBRT covers any cancer outside the prostate or in the seminal vesicles.
Treatment Modality | Benefits | Typical Use Cases |
Brachytherapy alone | High dose delivery to prostate, minimal side effects | Low-risk prostate cancer |
External Beam Radiation Therapy (EBRT) alone | Effective for treating larger areas, including any microscopic spread | Intermediate to high-risk prostate cancer |
Brachytherapy + EBRT | Combines high dose to prostate with treatment of any spread | Intermediate to high-risk prostate cancer |
Hormone Therapy Combinations
Hormone therapy, or androgen deprivation therapy (ADT), is often paired with radiation therapy. ADT lowers male hormones, which can help prostate cancer grow.
Brachytherapy with hormone therapy is very effective for high-risk patients. Hormone therapy can shrink the prostate. This makes brachytherapy more effective and could improve results.
Treatment Planning for Combined Approaches
Planning treatments that combine different methods is key. A team of healthcare experts works together. They create a treatment plan that fits each patient’s needs.
When planning, the team thinks about the order of treatments, doses, and side effects. Advanced imaging like MRI and CT scans help. They allow for precise targeting of the tumor while protecting healthy tissues.
Effectiveness of Prostate Brachytherapy
Prostate brachytherapy is a precise way to treat localized prostate cancer. It delivers radiation directly to the tumor. We’ll look at how well it works, including success rates and how it affects quality of life.
Success Rates for Different Risk Groups
Prostate brachytherapy works well for all risk groups. Low-risk patients often see a 90% success rate at 10 years. Intermediate- and high-risk patients also see good results, but it depends on their Gleason score and PSA levels.
Key statistics include:
- Low-risk patients: 90-95% biochemical recurrence-free survival at 10 years
- Intermediate-risk patients: 80-90% biochemical recurrence-free survival at 10 years
- High-risk patients: 70-80% biochemical recurrence-free survival at 10 years
Long-Term Survival Statistics
Long-term survival with prostate brachytherapy is promising. Studies show it’s as effective as surgery or external beam radiation therapy. This means patients can live long, healthy lives after treatment.
A notable study in a top oncology journal found an 80% overall survival rate at 15 years. This shows brachytherapy’s lasting benefits.
Disease-Free Survival Rates
How long patients stay disease-free is key. Research shows many patients stay disease-free for 10 years or more. Some studies report rates over 85% at 10 years.
Quality of Life Outcomes
Most patients have a good quality of life after brachytherapy. While some may face urinary or sexual issues, these often get better with time. Personalized care and follow-up are vital to manage any side effects.
Comparing Brachytherapy with Other Prostate Cancer Treatments
People with prostate cancer have many treatment options. These include brachytherapy, external beam radiation therapy, radical prostatectomy, and active surveillance. It’s important to know the differences to make the right choice.
We will look at how brachytherapy stacks up against other treatments. We’ll talk about what each has to offer, good and bad.
Brachytherapy vs. External Beam Radiation Therapy
Brachytherapy and external beam radiation therapy (EBRT) both use radiation. But they deliver it differently. Brachytherapy puts radioactive material inside the prostate. EBRT sends radiation from outside the body.
Brachytherapy’s advantages include targeting the tumor more directly. This means less harm to healthy tissues. But EBRT might be better for more advanced cancers or larger treatment areas.
Brachytherapy vs. Radical Prostatectomy
Radical prostatectomy removes the prostate gland through surgery. It’s different from brachytherapy, which keeps the prostate intact. Surgery can be more effective for localized cancer.
Brachytherapy’s benefits include being less invasive. It often leads to fewer side effects like incontinence. It also helps preserve sexual function. But surgery might be better for those with a longer life expectancy or cancer confined to the prostate.
Brachytherapy vs. Active Surveillance
Active surveillance watches the cancer closely, delaying treatment. Brachytherapy, on the other hand, aims to remove the cancer right away.
Brachytherapy is often chosen for those with intermediate-risk cancer or who want a more active treatment. Active surveillance is for low-risk cancer or those avoiding immediate treatment side effects.
Treatment | Invasiveness | Side Effects | Recovery Time |
Brachytherapy | Minimally invasive | Urinary issues, sexual dysfunction | Short |
External Beam Radiation Therapy | Non-invasive | Fatigue, urinary issues | Short |
Radical Prostatectomy | Invasive | Incontinence, sexual dysfunction | Longer |
Active Surveillance | Non-invasive | Anxiety, delayed treatment risk | N/A |
Potential Side Effects and Risks
It’s important for patients to know about the side effects of prostate brachytherapy. This treatment is good for prostate cancer, but knowing the risks is key. It helps patients make informed choices.
Short-Term Side Effects
Right after prostate brachytherapy, patients might feel more need to pee or have rectal pain. These issues can be helped with medicine and changes in daily life. Doctors might tell patients to avoid heavy lifting for a bit.
- Urinary issues, such as frequency or urgency
- Rectal discomfort or pain
- Temporary fatigue
These side effects usually go away in a few weeks or months. But, some people might keep feeling these issues and need ongoing care.
Long-Term Complications
Long-term problems can include not being able to control pee, trouble getting an erection, and radiation proctitis. The chance of these issues depends on the radiation dose, the patient’s health, and if they had problems before.
It’s vital for patients to talk to their doctors about their risks. This way, they know what to expect.
Managing and Minimizing Side Effects
It’s important to manage side effects well to improve life quality for those having prostate brachytherapy. This can be done with medicine, lifestyle changes, and regular check-ups with doctors.
- Pelvic floor exercises to improve urinary control
- Dietary adjustments to reduce urinary frequency and urgency
- Medications to manage erectile dysfunction or urinary symptoms
By knowing the side effects and risks of prostate brachytherapy and taking steps to manage them, patients can make better choices. This helps improve their treatment outcome.
Recovery and Post-Treatment Care
Recovering from prostate brachytherapy involves several steps. It’s important to follow guidelines to heal well. We’ll help you through this time, covering immediate care, long-term check-ups, and safety tips.
Immediate Post-Procedure Guidelines
Right after the treatment, rest is key. “Avoiding hard work, heavy lifting, and bending is vital,” experts say. Here’s what we suggest:
- Rest at home for 24 to 48 hours
- Avoid heavy lifting and bending
- Don’t drive until your doctor says it’s okay
Long-Term Follow-Up Protocol
Regular check-ups are important to see how treatment is working. We watch for:
- PSA levels to check for cancer
- Changes in urination or sex life
- Any late side effects
Regular visits help us fix any issues and adjust treatment plans. A patient said, “The care I got was top-notch, and it helped a lot.”
Radiation Safety Considerations
Brachytherapy radiation is mostly safe, but we’re careful about exposure. Pregnant women and young kids should stay away until it’s safe. We give personal advice on staying safe from radiation.
By sticking to these guidelines and keeping up with check-ups, patients can improve their recovery. Our team is here to support you every step of the way.
Conclusion
Prostate brachytherapy is a top choice for treating localized prostate cancer. It offers high survival rates and good quality of life. Knowing about brachytherapy helps patients choose the best treatment for them.
We looked at the different types of prostate brachytherapy. We also talked about how combining therapies can be key. The success rates of brachytherapy are high, making it a strong option for many patients.
Brachytherapy targets radiation to the tumor, sparing healthy tissue. This means fewer side effects and a faster recovery. Choosing brachytherapy can greatly improve a patient’s survival chances and quality of life.
FAQ
What is brachytherapy for prostate cancer?
Brachytherapy for prostate cancer uses small radioactive sources. They are placed inside or near the tumor. This method kills cancer cells while protecting healthy tissue.
How does prostate brachytherapy work?
Prostate brachytherapy targets cancer cells in the prostate gland. It uses small radioactive seeds or implants. This way, it spares the healthy tissue around it.
What are the types of prostate brachytherapy?
There are two main types. Low-Dose-Rate (LDR) brachytherapy uses permanent seeds. High-Dose-Rate (HDR) brachytherapy uses a temporary, high-dose source.
What is the difference between LDR and HDR brachytherapy?
LDR brachytherapy implants seeds that give off low doses of radiation for months. HDR brachytherapy uses a temporary, high-dose source that is removed after a short time.
Who is a candidate for prostate brachytherapy?
Those with localized prostate cancer and a low PSA level are candidates. A Gleason score of intermediate or low-risk is also required.
What are the benefits of prostate brachytherapy?
It has high success rates and little damage to healthy tissue. Recovery is also quick compared to other treatments.
What are the possible side effects of prostate brachytherapy?
Side effects include urinary issues and bowel problems. Erectile dysfunction is also possible. These are usually temporary and can be managed.
How is prostate brachytherapy performed?
It’s done under ultrasound guidance. Radioactive seeds or a temporary implant are placed in the prostate gland.
What is the recovery time for prostate brachytherapy?
Recovery is quick, with most men back to normal in a few days to a week.
Is brachytherapy used for prostate cancer treatment?
Yes, it’s a common treatment for localized prostate cancer.
Are radiation seeds used for prostate cancer?
Yes, seeds are used, mainly for LDR brachytherapy.
What is prostate seed brachytherapy?
It involves permanent implantation of small radioactive seeds in the prostate gland. This delivers radiation directly to the tumor.
Reference
- Nguyen, P. L., & Chen, M. H. (2009). Brachytherapy for prostate cancer: A systematic review. PLoS ONE, 4(8), e6698. https://pmc.ncbi.nlm.nih.gov/articles/PMC2735748/




































