Cancer treatment has changed a lot with the new external beam radiation therapy. This method is key to fighting cancer cells. It uses a cancer-treating machine to send precise radiation to the tumor. This way, it harms less of the healthy tissue around it.
Beam therapy targets specific areas of the body with cancer. It’s the most used radiation therapy, found in over 60 percent of cancer cases globally. Knowing about the different beam therapy types helps patients understand their treatment choices better.
Key Takeaways
- External beam radiation therapy is a non-invasive cancer treatment.
- It uses a machine to deliver precise radiation doses to the tumor.
- Beam therapy is a local treatment, targeting specific cancer sites.
- It is the most common form of radiation therapy used worldwide.
- Understanding beam therapy options helps patients make informed decisions.
The Science Behind External Beam Radiation Therapy
External beam radiation therapy targets and kills cancer cells with radiation beams. It uses high-energy particles or waves to harm cancer cells. This stops them from growing and dividing.
How Radiation Targets and Destroys Cancer Cells
Radiation therapy damages the DNA of cancer cells, leading to cell death. When radiation oncology machines send beams to the tumor, the energy harms the DNA. This stops the cancer cells from making copies, slowing down tumor growth.
The accuracy of external radiotherapy lets it send strong radiation right to the tumor. This keeps healthy tissues safe. Cancer radiotherapy machines use advanced technology to shape radiation beams for the tumor’s size and shape.
Prevalence and Importance in Modern Cancer Treatment
External beam radiation therapy is a key cancer treatment. It’s used at different stages of cancer care. It can be used alone or with surgery and chemotherapy.
New tech in radiation oncology machines makes treatments more precise. This leads to better results for patients. The field keeps improving, making external beam radiation therapy even more important in cancer treatment.
Radiotherapy Machine Technology: An Overview

Radiotherapy beam technology is key in modern cancer treatment. It offers flexible solutions for different tumors. Cancer radiotherapy machines are vital in radiation oncology, helping treat various tumors and locations.
Linear Accelerators and Beam Generation
The heart of most modern radiotherapy machines is the linear accelerator. It creates high-energy radiation beams. These beams are shaped to fit the tumor, ensuring the dose hits the target right.
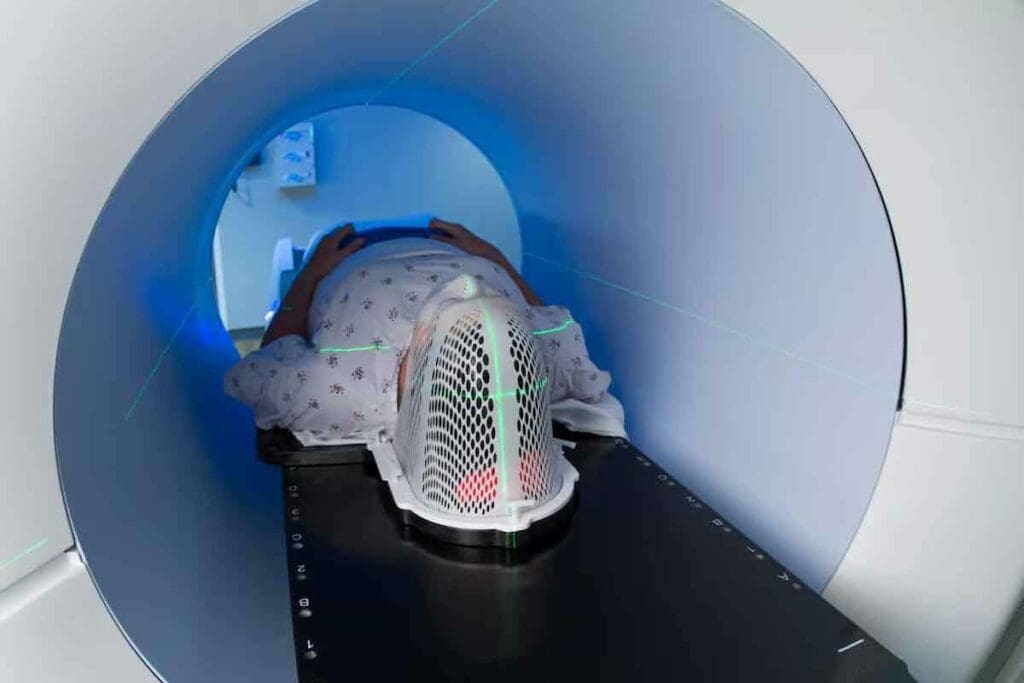
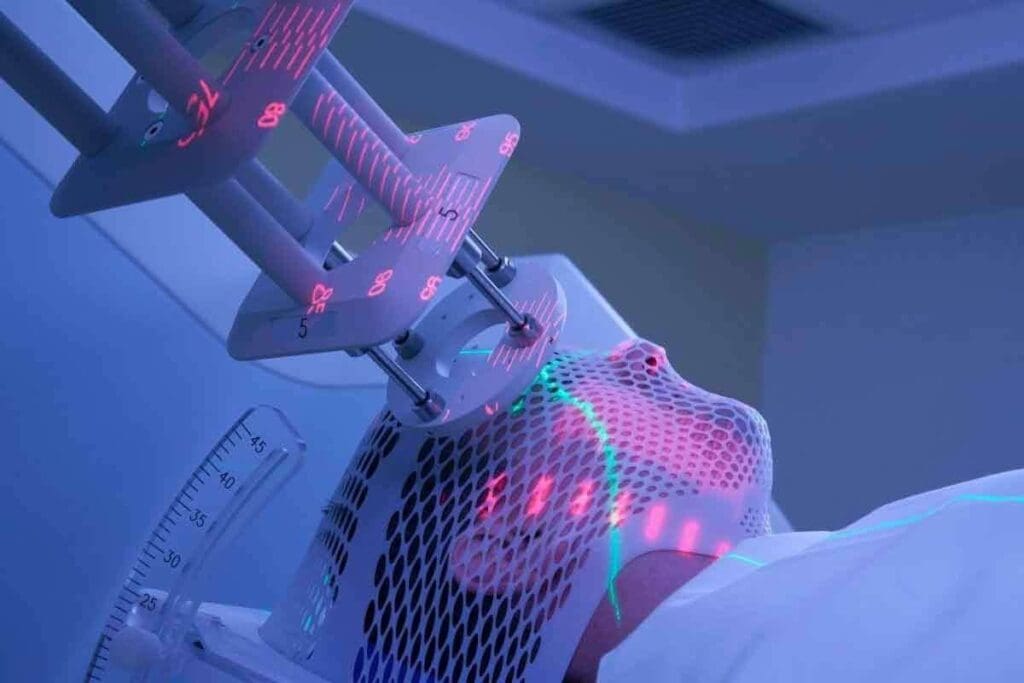
Precision Targeting Systems and Patient Positioning
Precision targeting is key in radiotherapy. It makes sure the radiation treatment machine hits the tumor right. Modern machines have advanced imaging for real-time monitoring and adjustments.
This is vital for beam radiotherapy methods like IMRT and VMAT. They need high precision.
The machine, or linear accelerator, moves around the patient. It sends beams from different angles. This method focuses the dose on the tumor, reducing harm to healthy tissue. It makes cancer beam therapy more effective.
Three-Dimensional Conformal Radiation Therapy (3D-CRT)
Three-Dimensional Conformal Radiation Therapy (3D-CRT) is a big step forward in external beam radiation therapy. It lets doctors target tumors more precisely. This way, they can protect the healthy tissues around them.
Fundamental Principles of 3D-CRT
The core idea of 3D-CRT is to make a detailed, three-dimensional image of the tumor. This image comes from CT, MRI, and PET scans. It’s key for planning how to aim the radiation beams at the tumor.
Thanks to advanced imaging, 3D-CRT can give the tumor a higher dose of radiation. At the same time, it protects important nearby structures. This is done through complex planning systems that figure out the best beam angles and intensities.
Treatment Planning and Delivery Process
The planning for 3D-CRT starts with imaging studies. These studies show where the tumor is and what’s around it. Then, a 3D model of the tumor and important structures is made.
Next, doctors use this 3D model to plan the treatment. They make sure the tumor gets the right dose of radiation. They also try to keep healthy tissues safe. The treatment is given by a radiation therapy machine, like a linear accelerator, which can aim beams from many angles.
Clinical Applications and Effectiveness
3D-CRT is used a lot in treating different cancers, like prostate, lung, and brain tumors. It’s good because it can give a high dose of radiation to the tumor. This helps avoid side effects.
Studies show that 3D-CRT can help control tumors better and improve survival rates for some cancers. It also helps reduce side effects. This makes life better for patients during and after treatment.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy (IMRT) is a big step forward in external beam radiation therapy. It lets doctors target tumors more accurately. This way, they can protect the healthy tissues around them.
Advanced Beam Modulation Techniques
IMRT uses new tech to change the intensity of radiation beams in small areas. This lets doctors give complex treatments with great precision. They do this by adjusting the beam strength in real-time, so more radiation goes to the tumor.
Protecting Healthy Tissue While Targeting Tumors
IMRT is great because it helps protect healthy tissue while hitting tumors hard. By changing the beam intensity, doctors can lower the dose to healthy areas. This cuts down on side effects and improves patient results.
The tech behind IMRT lets doctors give radiation doses that fit the tumor’s shape and size perfectly. This makes the treatment more effective. It also helps patients by lowering the chance of complications.
Volumetric-Modulated Arc Therapy (VMAT)
VMAT has changed radiation oncology with its new technology. It uses a continuous rotation to make treatments more efficient. This advanced radiation therapy gives precise treatment with arc technology.
Continuous Rotation Technology and Efficiency
VMAT’s technology lets radiation move in a continuous arc around the patient. This method makes treatments more efficient and precise. It also helps protect healthy tissues by rotating around the patient.
VMAT is faster than traditional IMRT, which is good for patients. Shorter treatments mean less time for patients and less chance of movement during treatment.
Comparing VMAT to IMRT: Clinical Advantages
VMAT has clear benefits over IMRT. VMAT offers:
- Reduced treatment times: VMAT’s technology makes treatments quicker.
- Improved dose distribution: Its arc therapy gives a more focused dose, making radiation therapy more effective.
- Enhanced patient comfort: Shorter treatments make patients more comfortable and compliant.
Studies show VMAT can match or beat IMRT in many cancer treatment cases. The choice between VMAT and IMRT depends on the patient’s needs.
In summary, VMAT is a big step forward in volumetric-modulated arc therapy. It brings better efficiency, precision, and comfort for patients. As cancer treatment evolves, VMAT will be key in delivering effective radiation therapy.
Image-Guided Radiation Therapy (IGRT)
Image-Guided Radiation Therapy (IGRT) is a big step forward in fighting cancer. It makes radiation therapy more precise. IGRT uses scans before and during treatment to hit the tumor right on target.
Real-Time Imaging During Treatment Sessions
IGRT’s main perk is real-time imaging during treatment. This lets doctors pinpoint the tumor’s exact spot, even if it moves. It helps adjust the radiation beam to hit the tumor, not healthy tissue.
Tumor Tracking and Adaptive Planning
IGRT tracks the tumor, which is key to moving tumors. It keeps an eye on the tumor’s spot, letting doctors tweak the plan as needed. This adaptive planning makes sure the radiation hits the tumor right, boosting treatment success.
Integration with Other Beam Therapy Techniques
IGRT works well with other treatments like IMRT and VMAT. This combo makes treatment more precise and effective. It helps doctors give more precise doses, saving healthy tissue and cutting down side effects.
Cancer radiotherapy machines are vital in fighting cancer. With IGRT, these machines make treatments more accurate and effective.
Stereotactic Radiosurgery (SRS) and Body Radiation Therapy (SBRT)
SRS and SBRT are changing radiation therapy with their precision and results. These methods have made a big difference in treating tumors. They offer hope to those with complex cases.
High-Precision, High-Dose Treatment Delivery
SRS and SBRT use advanced imaging and robots for precise radiation. This method treats tumors well while protecting healthy tissues. They use image-guided radiation therapy (IGRT) to track tumors during treatment.
These treatments are great for tumors that can’t be removed or are in hard-to-reach places. They target radiation carefully, lowering risks and improving results.
SRS Applications for Intracranial Lesions
SRS is key for treating brain lesions like metastases, AVMs, and benign tumors. It delivers precise radiation to hard-to-reach areas. This makes SRS perfect for cases where surgery or regular radiation therapy won’t work.
For brain tumors, SRS’s precision is vital. It uses advanced imaging to target tumors without harming the brain.
SBRT for Extracranial Tumors and Oligometastases
SBRT applies SRS’s precision to tumors outside the brain. It’s great for treating a few metastases. SBRT can give high doses of radiation to these tumors, aiming for local control and better survival.
SBRT is used for many types of tumors, from the lung and liver to the prostate. It’s a good choice for those who can’t have surgery or other treatments.
Proton Beam Therapy: Advanced Particle Treatment
Proton beam therapy is a new way to fight cancer. It uses protons instead of X-rays to kill cancer cells. This method is more precise and effective for many cancers.
The Physics of Proton Energy Deposition
Proton beam therapy works because of how protons deposit energy. Protons are charged particles that can travel deep into the body. Unlike X-rays, protons have a special property called the Bragg peak.
The Bragg peak phenomenon means protons deposit most of their energy at a specific point. This is where the tumor is. So, healthy tissues nearby get less damage.
Bragg Peak Phenomenon and Tissue Sparing
The Bragg peak is key to proton beam therapy’s benefits. It helps deliver a strong dose to the tumor but spares healthy tissues. This is great for tumors close to important areas like the brain or spine.
The advantages of proton beam therapy include:
- Less radiation to healthy tissues
- Lower risk of side effects and long-term problems
- Good for tumors near critical areas
- Potential for better cancer treatment results
Proton beam therapy is best for deep tumors. As shown in the image below, it can reach deep tumors and stop there. This reduces damage to healthy tissue nearby.
In summary, proton beam therapy is a big step forward in cancer treatment. Its unique properties, like the Bragg peak, allow for precise and effective treatment. This helps protect healthy tissues while targeting tumors.
Electron Beam Therapy for Surface Lesions
Electron beam therapy is a precise treatment for surface lesions. It uses electron beams that can’t travel far through body tissues. This makes it great for treating skin tumors or those near the body’s surface.
Because of this, electron beam therapy causes less damage to deeper tissues. It’s often used for cancers close to the skin.
Electron Energy Selection and Penetration Depth
The energy of the electron beam affects how deep it can go. Higher energy beams go deeper, while lower energy beams are better for surface lesions.
Choosing the right electron energy is key to good treatment planning. It helps make sure the tumor gets enough radiation without harming deeper healthy tissues.
Clinical Indications and Treatment Planning
Electron beam therapy is used for many surface lesions, like some skin cancers and shallow tumors. Planning treatment involves looking at the tumor’s size, depth, and where it is.
Advanced systems help plan electron beam therapy. They make sure the radiation dose fits the tumor’s shape and size well.
Effective treatment planning is vital for electron beam therapy success. A team of experts works together to give patients the best care.
Cancer and Radiotherapy Machine Advancements and Future Directions
The field of radiation oncology is seeing big changes in cancer radiotherapy machines. These changes are changing how we treat cancer.
Cancer radiotherapy machines are key in radiation oncology. They offer flexible external radiotherapy solutions. Researchers are working on new technologies to make these machines more precise and effective.
Artificial Intelligence in Treatment Planning
Artificial intelligence (AI) is being used in treatment planning for cancer radiotherapy. AI algorithms can look at lots of data, like medical images and patient info. This helps make treatment plans better.
- AI-assisted contouring of tumors and organs at risk
- Personalized treatment planning based on patient-specific data
- Real-time adaptation of treatment plans during radiation therapy
MRI-Guided Linear Accelerators
MRI-guided linear accelerators are a big step forward in radiotherapy technology. They combine MRI imaging with radiation therapy delivery.
Key benefits include:
- Real-time imaging during treatment
- Improved tumor tracking and targeting
- Reduced margins around tumors, sparing healthy tissue
FLASH Radiotherapy and Ultra-High Dose Rates
FLASH radiotherapy is a new technique that uses ultra-high dose rates. It shows promise in reducing damage to healthy tissues while keeping tumors under control.
Researchers are looking into the benefits of FLASH radiotherapy. These include:
- Reduced toxicity to normal tissues
- Improved tumor control
- Potential for hypofractionation and reduced treatment times
As radiotherapy technology keeps getting better, we can expect to see more AI, MRI-guided linear accelerators, and FLASH radiotherapy. These advancements will likely shape the future of cancer treatment.
Conclusion: Selecting the Optimal External Beam Therapy Approach
External beam therapy is key in modern cancer care. It offers many ways to treat cancer based on its type and stage. The right choice depends on where the tumor is, the patient’s health, and the cancer’s stage.
Radiation therapy has grown a lot thanks to new technology. Machines like linear accelerators and precision systems help target cancer better. Techniques like 3D-CRT, IMRT, VMAT, IGRT, SRS, SBRT, proton beam therapy, and electron beam therapy give patients more options.
Choosing the best external beam therapy needs careful thought. Healthcare experts must know the good and bad of each method. This way, they can make treatment plans that work best for each patient.
As cancer treatment keeps getting better, external beam therapy will keep playing a big role. It offers patients effective and focused ways to fight cancer.
FAQ
What is external beam radiation therapy?
External beam radiation therapy is a cancer treatment. It uses a machine to send high-energy beams to the tumor. This targets and kills cancer cells.
How does radiation target and destroy cancer cells?
Radiation therapy damages cancer cells’ DNA. This stops them from growing and dividing. The beams aim at the tumor, killing cells and shrinking tumors.
What is the difference between 3D-CRT and IMRT?
3D-CRT uses beams from many angles to match the tumor’s shape. IMRT is more advanced. It changes the beam’s intensity for better tumor targeting and less damage to healthy tissue.
What is VMAT, and how does it compare to IMRT?
VMAT uses beams while the machine moves around the patient. It’s often faster than IMRT. This means treatments can be shorter without losing quality.
What is IGRT, and how is it used in radiation therapy?
IGRT uses live images during treatment. It ensures the tumor is targeted correctly. It works with IMRT and VMAT to improve treatment.
What is proton beam therapy, and how does it differ from traditional radiation therapy?
Proton beam therapy uses protons to kill cancer cells. Protons have a unique property that focuses their energy. This spares healthy tissue beyond the tumor.
What is the role of artificial intelligence in radiation therapy?
Artificial intelligence is used in radiation therapy. It helps plan treatments, automates tasks, and improves delivery. AI can make plans better, shorten treatment times, and enhance outcomes.
What is FLASH radiotherapy, and what are its potential benefits?
FLASH radiotherapy delivers radiation at very high speeds. It might reduce treatment times and improve results. It’s a new area of research with promising benefits.
How is electron beam therapy used in cancer treatment?
Electron beam therapy treats surface lesions and tumors near the skin. Its shallow penetration is perfect for superficial tumors, protecting deeper tissue.
What are the benefits of MRI-guided linear accelerators in radiation therapy?
MRI-guided linear accelerators combine MRI imaging with radiation therapy. This allows for precise, real-time treatment plans. It improves treatment accuracy and effectiveness.
How is the optimal external beam therapy approach selected for each patient?
The best treatment plan is chosen based on the patient’s tumor,size, nd location. It also considers the patient’s health and medical history. A team of experts works together to find the best plan.
References
- Xiang, H., et al. (2017). Systematic review and meta-analysis of the diagnostic accuracy of low-dose CT KUB in diagnosing clinically significant urolithiasis. Journal of Medical Imaging and Radiation Oncology, 61(3), 415-422. https://onlinelibrary.wiley.com/doi/10.1111/1754-9485.12587
- Gilbert, F. J. (2022). Diagnostic accuracy systematic review and meta-analysis. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK578679/