sickle cell disease
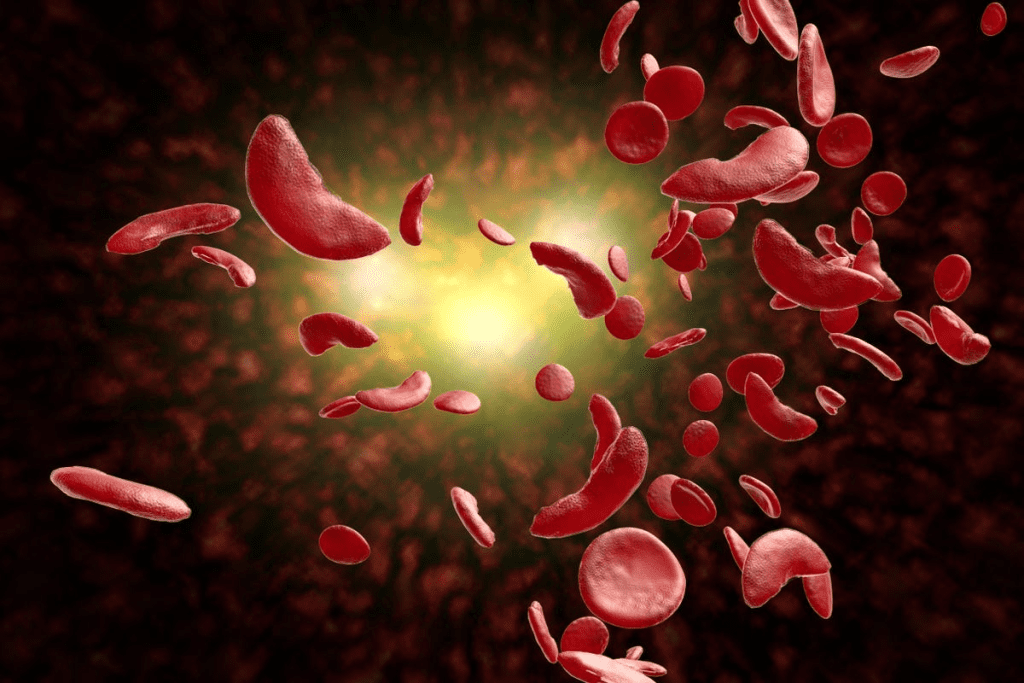
Sickle Cell Disease is a rare genetic disorder that affects how red blood cells carry oxygen. This happens because of a problem with hemoglobin, a protein in red blood cells. As a result, red blood cells can become sickle-shaped, causing serious health issues. In some cases, rare genetic results double sickle cell conditions may occur, leading to more severe symptoms and complications.
This disease can lead to a lot of pain, infections, and even damage to organs over time. It’s important to understand this condition well. This helps in managing its effects and improving life quality for those affected.
Looking into the causes, symptoms, and treatments for Sickle Cell Disease shows we need a detailed plan. This is the only way to handle this complex condition effectively.
Key Takeaways
- Sickle Cell Disease is a genetic disorder affecting hemoglobin production.
- It causes red blood cells to take on a sickle shape, leading to health complications.
- Understanding the condition is key to managing its effects.
- Complications can include pain episodes, infections, and organ damage.
- A comprehensive approach is necessary for managing Sickle Cell Disease.
The Science Behind Sickle Cell Disease
sickle cell disease mechanism
To understand sickle cell disease, we need to look at its genetic and molecular roots. It’s a genetic disorder that messes with hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen.
Definition and Basic Mechanism
Sickle cell disease comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation leads to abnormal hemoglobin, called hemoglobin S (HbS).
Hemoglobin S changes shape when it loses oxygen. This causes red blood cells to become sickle-shaped. These sickle cells can get stuck in blood vessels, blocking blood flow and causing problems.
Types of Sickle Cell Disease
There are several types of sickle cell disease, based on the genotype. The main types are:
- HBSS (Sickle Cell Anemia): This is the most severe form. It happens when someone gets two HbS genes, one from each parent.
- HBSC: This occurs when someone has one HbS gene and one HbC gene. It’s generally milder.
- HBAS (Sickle Cell Trait): People with one normal gene and one HbS gene are carriers. They usually don’t show symptoms but can pass the HbS gene to their kids.
- Other variants: There are rarer types, like HbS-beta thalassemia. These come from different abnormal hemoglobin genes.
| Type of Sickle Cell Disease | Genotype | Severity |
| Sickle Cell Anemia | HBSS | Severe |
| HBSC Disease | HBSC | Mild to Moderate |
| Sickle Cell Trait | HBAS | Generally Asymptomatic |
| HbS-beta Thalassemia | HBs/beta thalassemia | Variable |
Knowing about these types helps in managing the disease. It ensures the right care for those affected.
The Genetic Basis of Sickle Cell Disease
hemoglobin S mutation
To understand sickle cell disease, we must look at the hemoglobin S mutation. This mutation causes the disease by making abnormal hemoglobin, known as hemoglobin S.
Sickle cell disease is a genetic disorder. It comes from a single change in the HBB gene. This gene codes for the beta-globin subunit of hemoglobin. The change swaps glutamic acid with valine at the sixth position, making hemoglobin S.
Hemoglobin S Mutation
The hemoglobin S mutation is a single change in the HBB gene. This change makes abnormal hemoglobin. Under low oxygen, this hemoglobin can turn red blood cells into a sickle shape.
- The mutation affects the beta-globin subunit of hemoglobin.
- It results in the production of hemoglobin S, which is prone to polymerization.
- This polymerization causes red blood cells to sickle, leading to various complications.
Inheritance Patterns
Sickle cell disease is inherited in an autosomal recessive way. This means a person needs two defective HBB genes, one from each parent, to have the disease.
- If someone has one normal and one mutated HBB gene, they are a carrier.
- Carriers usually don’t show the disease’s full symptoms but can pass the mutated gene to their kids.
- The chance of two carrier parents having a child with sickle cell disease is 25%.
Knowing the genetic basis and inheritance patterns of sickle cell disease is key for genetic counseling. It’s also important for family planning. It shows why genetic testing is vital to find carriers and those affected.
How Sickle Cell Disease Affects Red Blood Cells
sickled red blood cells
Sickle cell disease changes red blood cells in big ways. These cells are key for carrying oxygen around the body. When they don’t work right, it can cause health problems.
Normal vs. Sickled Red Blood Cells
Normal red blood cells are flexible and disk-shaped. They move easily through blood vessels. But, sickled red blood cells are stiff and crescent-shaped because of sickle cell disease. This shape makes it hard for them to get through small blood vessels, which can cause blockages.
The Sickling Process
The sickling process happens when red blood cells, already affected by sickle cell disease, face low oxygen levels. The abnormal hemoglobin then changes the cell’s shape. This can be set off by things like dehydration, high altitudes, or hard physical work.
Once a red blood cell sickles, it’s more likely to break down, leading to anemia. The sickling process can also damage the cell’s membrane. This makes the cell work even worse.
Reduced Oxygen-Carrying Capacity
The oxygen-carrying capacity of red blood cells drops in people with sickle cell disease. Sickled cells are not only less flexible but also less good at carrying oxygen. This means tissues don’t get enough oxygen, leading to more problems.
Also, sickled red blood cells don’t last as long. This means there are fewer red blood cells overall. This makes anemia worse and makes it harder for the body to carry oxygen.
Acute Complications of Sickle Cell Disease
sickle cell disease acute complications
Sickle cell disease can cause severe problems that need quick medical help. These issues happen when red blood cells get stuck in small blood vessels. This can cut off blood flow to tissues.
Vaso-occlusive Crisis (Pain Crisis)
A vaso-occlusive crisis, or pain crisis, is a common problem. It happens when sickled red blood cells block blood vessels. This causes pain that can be mild or very severe.
The pain from a vaso-occlusive crisis can be very hard to handle. It’s important to get treatment right away to avoid more serious issues.
Acute Chest Syndrome
Acute chest syndrome is a serious issue for sickle cell disease patients. It shows up as a new spot on a chest X-ray, often with fever, cough, or trouble breathing.
This condition is a big reason for sickness and death in people with sickle cell disease. It can be caused by infection, fat in the blood, or damaged blood vessels. Treatment includes oxygen, blood transfusions, and supportive care.
Stroke and Neurological Complications
Stroke is a big risk for those with sickle cell disease, especially kids. Sickled red blood cells can block blood vessels, causing ischemic stroke. Hemorrhagic stroke can happen because of weak blood vessels.
Other brain problems include seizures, brief strokes, and brain damage. It’s key to catch and treat stroke risks early to avoid lasting brain damage.
Chronic Complications and Organ Damage
sickle cell disease complications
Chronic complications from Sickle Cell Disease can cause a lot of harm over time. As people get older, the damage from sickling and blocked blood vessels can harm different organs.
Chronic Anemia Effects
Chronic anemia is a big problem in Sickle Cell Disease. It happens when red blood cells break down too early. This can lead to many issues, including:
- Fatigue and Weakness: Not enough red blood cells can make you very tired and weak.
- Delayed Growth and Development: Kids with chronic anemia might grow and develop slower.
- Increased Risk of Infections: Anemia can make it harder for your body to fight off infections.
Organ Systems Affected
Sickle Cell Disease can harm many parts of the body. This leads to long-term problems. Some of the main affected areas are:
- Cardiovascular System: Chronic anemia can make the heart bigger and lead to heart failure.
- Renal System: Sickle Cell Disease can damage the kidneys, causing chronic kidney disease.
- Hepatic System: The liver can also be affected, leading to issues like gallstones and liver problems.
Cumulative Damage Over Time
The damage from Sickle Cell Disease adds up over time. This can make life very hard and shorten life expectancy. It’s important to manage these long-term problems to help patients live better.
Dealing with Sickle Cell Disease needs a full care plan. This plan should cover both the immediate and long-term issues. Understanding the damage to organs and chronic complications helps doctors find better ways to help patients.
Recognizing Sickle Cell Disease Symptoms
symptoms of sickle cell disease
Spotting sickle cell disease symptoms early can greatly improve life quality. This genetic disorder messes with hemoglobin in red blood cells, causing health problems.
Early Childhood Symptoms
In young kids, sickle cell disease symptoms include frequent infections, anemia, and swelling in the hands and feet. These happen because the abnormal hemoglobin makes red blood cells misshapen and break down.
Parents and caregivers need to watch for illness signs in kids. Early diagnosis and treatment can make a big difference in managing the disease.
Adolescent and Adult Symptoms
As people with sickle cell disease grow up, they face symptoms like chronic pain, fatigue, and jaundice. How often and how bad these symptoms are can differ a lot from person to person.
Adults with sickle cell disease might also face organ damage and increased risk of infections. This shows why they need to keep seeing doctors.
Warning Signs of Crisis
It’s very important for people with sickle cell disease and their caregivers to know the crisis warning signs. These include severe pain, shortness of breath, and fever. Getting medical help fast is key to avoiding serious problems.
Knowing the symptoms and crisis warning signs of sickle cell disease is crucial for managing it well. Being aware helps people get medical help when needed and can improve their life quality.
| Age Group | Common Symptoms | Warning Signs of Crisis |
| Early Childhood | Frequent infections, anemia, swelling in hands and feet | Severe pain, fever, difficulty breathing |
| Adolescence and Adulthood | Chronic pain, fatigue, jaundice, organ damage | Severe pain, shortness of breath, fever, dactylitis |
Diagnosing Sickle Cell Disease
sickle cell disease diagnosis methods
It’s important for patients and doctors to know how sickle cell disease is diagnosed. There are several ways to find out early and manage it well.
Newborn Screening
Newborn screening for sickle cell disease is common in many places, like the United States. It’s key because it starts treatment and prevention early. A simple blood test from a heel prick checks for sickle hemoglobin.
Blood Tests and Genetic Testing
Blood tests are key in diagnosing sickle cell disease. Complete Blood Count (CBC) and hemoglobin electrophoresis are used a lot. CBC checks the blood’s health, and hemoglobin electrophoresis finds sickle hemoglobin. Genetic testing finds the cause of the disease, helping with prenatal diagnosis and finding carriers.
The blood test process is:
- Getting a blood sample from the patient.
- Looking for sickle hemoglobin in the blood.
- Doing more tests if needed to confirm.
Prenatal Diagnosis
Prenatal diagnosis finds sickle cell disease in the fetus. Chorionic villus sampling (CVS) or amniocentesis get fetal cells for genetic tests. This helps parents make choices about their pregnancy.
Accurate and early diagnosis of sickle cell disease is key. Thanks to new medical tech, we can diagnose and manage it better than before.
Understanding Sickle Cell Trait vs. Sickle Cell Disease
It’s important to know the difference between sickle cell trait and sickle cell disease. Both involve the sickle cell gene, but they affect health differently.
Differences in Symptoms and Risks
Sickle cell trait means you have one normal and one sickle hemoglobin gene. People with this trait usually don’t show all the symptoms of sickle cell disease. But, they might face some issues during intense workouts or at high altitudes.
Sickle cell disease is more serious. It comes from having two sickle hemoglobin genes. Symptoms include pain episodes, infections, and anemia. This disease can greatly affect a person’s life and needs constant medical care.
“It’s not just about being a carrier; understanding whether you have sickle cell trait or sickle cell disease can have significant implications for your health and the health of your family members.”
Health Considerations for Carriers
People with sickle cell trait should be mindful of their health. They usually live healthy lives but need to watch out for certain situations. These include:
- Dehydration
- High-intensity exercise
- Travel to high-altitude areas
Knowing these risks and taking steps to prevent them is key. Also, genetic counseling is advised for those with sickle cell trait planning to have children. This helps understand the chances of passing the condition to their kids.
In summary, sickle cell trait and disease both involve the sickle cell gene but have different health effects. Knowing the differences is crucial for managing health and making smart choices.
Triggers That Worsen Sickle Cell Disease
Knowing what triggers sickle cell disease is key to managing it well. People with this condition must understand what can make their symptoms worse. This knowledge helps avoid severe problems.
Environmental Factors
Environmental factors are big triggers for sickle cell crises. Extreme temperatures, whether hot or cold, can cause a crisis. For example, sudden temperature changes can make red blood cells sickle.
- High altitudes with lower oxygen levels can trigger sickling.
- Exposure to cold temperatures, especially in air-conditioned spaces or during swimming, can induce vaso-occlusive crises.
A study in the Journal of Clinical Rheumatology found that environmental factors like temperature and humidity affect sickle cell crises.
Physical Stressors
Physical stressors also play a big role in worsening sickle cell disease. Doing intense physical activity, especially in hot weather or without enough water, can lead to dehydration. This increases the risk of a sickle cell crisis.
| Physical Stressor | Effect on Sickle Cell Disease |
| Intense Exercise | Increases risk of dehydration and sickling |
| Physical Trauma | Can trigger vaso-occlusive crises |
| Infections | Can cause inflammation, leading to sickling |
Dehydration and Its Effects
Dehydration is a major trigger for sickle cell crises. When we lose more fluids than we take in, our red blood cells get more concentrated. This makes them sickle. It’s important to stay hydrated to manage the condition.
“Adequate hydration is crucial in preventing the concentration of red blood cells that can lead to sickling,” according to a leading hematologist.
We suggest that patients with sickle cell disease drink lots of water. This is especially important during hot weather or when they’re being active. It helps prevent dehydration.
Standard Treatments for Sickle Cell Disease
Standard treatments for sickle cell disease aim to reduce symptoms and prevent complications. They improve quality of life. A comprehensive approach is needed, using various treatment strategies.
Pain Management Approaches
Pain management is key in treating sickle cell disease. We use hydration, pain medications, and rest to manage pain. Sometimes, hospitalization is needed for severe pain episodes.
“Pain is the hallmark of sickle cell disease, and its management is crucial to improving the quality of life for patients,” – A leading expert in hematology. “A multi-faceted approach to pain management can significantly reduce the frequency and severity of pain crises.”
- Hydration: Drinking plenty of fluids to help prevent dehydration, which can trigger pain crises.
- Pain Medications: Using over-the-counter or prescription pain medications as directed by a healthcare provider.
- Rest: Getting plenty of rest to help the body recover from pain episodes.
Hydroxyurea and Other Medications
Hydroxyurea reduces pain crises and may lower blood transfusion needs. Other medications manage specific complications of sickle cell disease.
| Medication | Purpose | Benefits |
| Hydroxyurea | Reduces frequency of pain crises | Decreased need for blood transfusions, reduced pain episodes |
| Penicillin | Prevents infections | Reduced risk of infections, especially in children |
Blood Transfusions
Blood transfusions reduce stroke risk and manage severe anemia. Regular transfusions improve oxygen delivery to tissues and organs.
By using these standard treatments, we can better manage sickle cell disease. This improves the quality of life for those affected.
Advanced Therapies and Emerging Treatments
Advanced therapies are changing how we treat sickle cell disease. They bring hope to those affected. New treatments aim to lessen sickle cell crises and enhance life quality.
Gene Therapy Approaches
Gene therapy is a hopeful area in sickle cell disease treatment. It fixes the genetic issue causing the disease. This way, patients can make healthy hemoglobin. Clinical trials are testing its safety and effectiveness, showing promising results.
One method uses a patient’s stem cells, which are then modified to make normal hemoglobin. Early trials suggest it could greatly reduce sickle cell events.
Stem Cell Transplantation
Stem cell transplantation, especially hematopoietic stem cell transplantation (HSCT), is being explored. HSCT replaces a patient’s bone marrow with healthy stem cells. This could cure sickle cell disease by making normal red blood cells.
However, HSCT comes with risks like graft-versus-host disease and the need for immunosuppressive drugs. Researchers are working to make it safer and more accessible for sickle cell patients.
New Medications in Development
New medications are also being developed for sickle cell disease. These aim to reduce crises, improve anemia, and protect organs.
Some target the sickling process, like anti-adhesion molecules and anti-inflammatory drugs. Others focus on boosting hemoglobin production or reducing hemolysis.
| Therapy Type | Description | Potential Benefits |
| Gene Therapy | Corrects genetic mutation to produce healthy hemoglobin | Potential cure, reduced sickling events |
| Stem Cell Transplantation | Replaces bone marrow with healthy stem cells | Potential cure, normal red blood cell production |
| New Medications | Targets sickling process, improves hemoglobin production | Reduced vaso-occlusive crises, improved quality of life |
As research advances, the future for sickle cell disease patients looks brighter. New therapies and treatments offer hope for better management and outcomes. Ongoing trials and studies are key to understanding their long-term benefits and safety.
Life Expectancy and Prognosis with Sickle Cell Disease
The outlook for people with sickle cell disease has improved a lot. This is thanks to better medical care and management. In the past, life expectancy was much lower. But now, thanks to healthcare progress, the future looks brighter.
Historical vs. Current Life Expectancy
Years ago, people with sickle cell disease often didn’t live long. Many didn’t make it past their 20s. But, thanks to new treatments and better care, life expectancy has increased.
Now, with the right care, many can live into their 40s, 50s, and even longer.
Factors Affecting Prognosis
Several things can change how long someone with sickle cell disease might live. These include:
- Access to Healthcare: Getting regular medical care and managing problems well can help a lot.
- Genetic Factors: Some genetic changes can make the disease worse or better.
- Environmental Factors: Things like infections, extreme weather, and stress can also play a role.
- Lifestyle Choices: Eating well, staying hydrated, and living a healthy lifestyle can help too.
Quality of Life Considerations
Life expectancy is important, but so is the quality of life. Thanks to better pain management and support, people with sickle cell disease can live more fully. It’s all about a holistic approach to care.
Understanding what affects life expectancy and quality of life helps everyone involved. Healthcare providers and those with sickle cell disease can work together to make life better.
Living With Sickle Cell Disease
People with sickle cell disease can live full lives with the right lifestyle and care. It’s all about a mix of medical treatment, lifestyle changes, and ongoing care.
Lifestyle Modifications
Changing your lifestyle is key for those with sickle cell disease. These changes can cut down on crises and boost health.
- Stay Hydrated: Drinking lots of water is key to avoid dehydration, which can lead to a crisis.
- Avoid Extreme Temperatures: High and low temperatures can cause sickling. So, it’s best to stay away from extreme weather.
- Exercise Regularly: Gentle activities like walking or swimming can improve blood flow without stressing the body too much.
- Maintain a Balanced Diet: Eating foods rich in fruits, veggies, and whole grains is good for your health.
Preventive Care Strategies
Preventive care is vital for managing sickle cell disease. Regular doctor visits and vaccines are key parts of this care.
- Regular Health Check-Ups: Seeing your doctor often helps keep an eye on your condition and solve problems quickly.
- Vaccinations: Keeping up with vaccines can stop infections that might cause a crisis.
- Monitoring for Complications: Regular tests can spot problems early, allowing for quick action.
Managing Daily Activities
Living with sickle cell disease means making some daily routine changes. This helps manage the condition better.
- Plan Ahead: Thinking ahead and planning for crises can lessen their impact.
- Prioritize Rest: Rest is important to avoid getting too tired, which can make the condition worse.
- Stay Organized: Keeping track of meds, appointments, and health tasks can help manage the condition better.
By using these strategies, people with sickle cell disease can live more stable and fulfilling lives. We’re here to offer full support and care to manage this condition well.
Psychological and Social Impacts
Sickle cell disease affects more than just the body. It impacts mental health and how people interact with others. Living with this disease is tough, not just for the person but also for their family and caregivers.
Mental Health Challenges
People with sickle cell disease face a higher risk of mental health problems like depression and anxiety. The constant pain and need for hospital visits can make them feel isolated and frustrated.
It’s key to focus on mental health to improve overall well-being. So, adding mental health support to a patient’s care plan is crucial.
Educational and Occupational Effects
Sickle cell disease can affect a person’s education and job chances. Missing school or work because of health issues can slow down progress in school or at work.
We suggest that patients work with their teachers and bosses to find solutions. This way, they can reach their goals despite the challenges.
Support Systems and Resources
A strong support system is essential for those with sickle cell disease. This includes family, friends, healthcare teams, and support groups. They offer emotional support, help with daily tasks, and share important information.
We stress the need for patients to find resources that help them deal with the disease. This improves their quality of life and lets them live a fulfilling life.
Sickle Cell Disease Around the World
Sickle cell disease is a big health problem worldwide. It affects millions of people, with different numbers in different places.
Prevalence in Different Populations
In places where malaria used to be common, sickle cell disease is more common. This is because the disease’s genetic mutation helps protect against malaria. These areas include parts of sub-Saharan Africa, the Middle East, and India.
The disease is not just found in these places. It’s a global issue because of people moving around. For example, in the United States, about 100,000 people have sickle cell disease, mostly African Americans.
| Region | Estimated Prevalence | Population Affected |
| Sub-Saharan Africa | 1 in 100 births | Approximately 300,000 births per year |
| Middle East | 1 in 400 births | Significant numbers in Saudi Arabia and Iran |
| India | 1 in 1,800 births | High prevalence in certain tribal groups |
| United States | 1 in 365 African Americans | Approximately 100,000 people |
Global Health Initiatives
Many global health efforts aim to fight sickle cell disease. These include newborn screening, public awareness, and research into new treatments.
Key Initiatives:
- Newborn screening to enable early intervention
- Development of guidelines for diagnosis and treatment
- Research into gene therapy and other novel treatments
Disparities in Care and Access
Even with these efforts, there are still big gaps in care and access. In many poor countries, getting diagnosed and treated is hard or too expensive.
We need better healthcare and education for both doctors and the public. This will help fix these gaps.
Together, we can work towards a future where everyone affected by sickle cell disease has access to the care they need.
Conclusion: The Future of Sickle Cell Disease Care
Looking ahead, sickle cell disease care is set to improve thanks to new treatments and research. Gene therapy and stem cell transplantation are leading the way. These advancements could change how we manage this condition.
Today, we’re moving towards treatments that are more tailored to each patient. Medications like hydroxyurea help reduce pain and improve life quality. Research is also leading to new treatments that meet the complex needs of patients.
Global health efforts are also playing a big role. They aim to make care more accessible and reduce treatment gaps. By continuing to research and develop better treatments, we can make a big difference in the lives of those with sickle cell disease worldwide.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic disorder. It affects how red blood cells make hemoglobin. This makes the cells misshapen and break down.
What are the symptoms of sickle cell disease?
Symptoms include pain episodes, anemia, and infections. Organs like the spleen, kidneys, and liver can also be damaged. Symptoms vary among people.
How is sickle cell disease inherited?
It’s inherited in an autosomal recessive pattern. A person needs two abnormal hemoglobin genes, one from each parent, to have the disease.
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait happens when a person has one normal and one abnormal hemoglobin gene. Carriers usually don’t show all the disease symptoms but can pass the gene to their kids.
How is sickle cell disease diagnosed?
It’s diagnosed through newborn screening, blood tests, or genetic testing. Prenatal diagnosis is also possible.
What are the treatment options for sickle cell disease?
Treatments include managing pain, using hydroxyurea, and blood transfusions. Advanced therapies like gene therapy or stem cell transplantation are also options.
Can sickle cell disease be cured?
The only current cures are stem cell transplantation and gene therapy. These treatments are risky and not for everyone.
What triggers sickle cell crises?
Crises can be triggered by dehydration, extreme temperatures, physical stress, infections, and certain medications. Avoiding these triggers is key.
How can individuals with sickle cell disease manage their condition?
Management involves lifestyle changes, preventive care, staying hydrated, avoiding extreme temperatures, and following treatment plans.
What is the life expectancy for someone with sickle cell disease?
Life expectancy has improved with modern treatments. Factors like disease severity, healthcare access, and complications affect prognosis.
Are there any new treatments being developed for sickle cell disease?
Yes, research is exploring new treatments. These include gene therapy, stem cell transplantation, and medications to reduce crisis frequency and severity.
How does sickle cell disease affect mental health?
It can lead to mental health issues like anxiety, depression, and stress. Managing a chronic condition can be emotionally challenging.
What support systems are available for individuals with sickle cell disease?
Support includes healthcare providers, patient organizations, support groups, and educational resources. These are crucial for managing the disease.
References
- National Heart, Lung, and Blood Institute. (2022, July 15). Sickle Cell Disease. National Institutes of Health. https://www.nhlbi.nih.gov/health/sickle-cell-disease
- National Human Genome Research Institute. (2024, April 17). About Sickle Cell Disease. https://www.genome.gov/Genetic-Disorders/Sickle-Cell-Disease