Autoimmune eye diseases are a big health issue. They can harm many parts of the eye and even threaten your sight. When your immune system attacks healthy cells, it can hit any part of your body, including your eyes.Discover the shocking link between red eyes and autoimmune disease. Learn the 7 key causes and proven strategies for lasting relief.
We’ll look at how these diseases can lead to different eye problems. This can cause a variety of symptoms and issues. Knowing the signs, causes, and treatment options is key. It helps catch these diseases early and stop them from causing permanent vision loss.
Key Takeaways
- Autoimmune eye diseases can cause significant ocular complications.
- These conditions occur when the immune system attacks healthy eye tissues.
- Early diagnosis and treatment are critical to prevent vision loss.
- Understanding symptoms and causes can lead to timely medical intervention.
- Experienced specialists can provide relief and restore quality of life.
Understanding Autoimmune Eye Diseases
It’s important to know about autoimmune eye diseases to treat vision problems. These diseases happen when the body’s immune system attacks its own tissues. Over 80 types of autoimmune diseases exist, making them a big cause of chronic illness in the U.S.
What Are Autoimmune Eye Diseases?
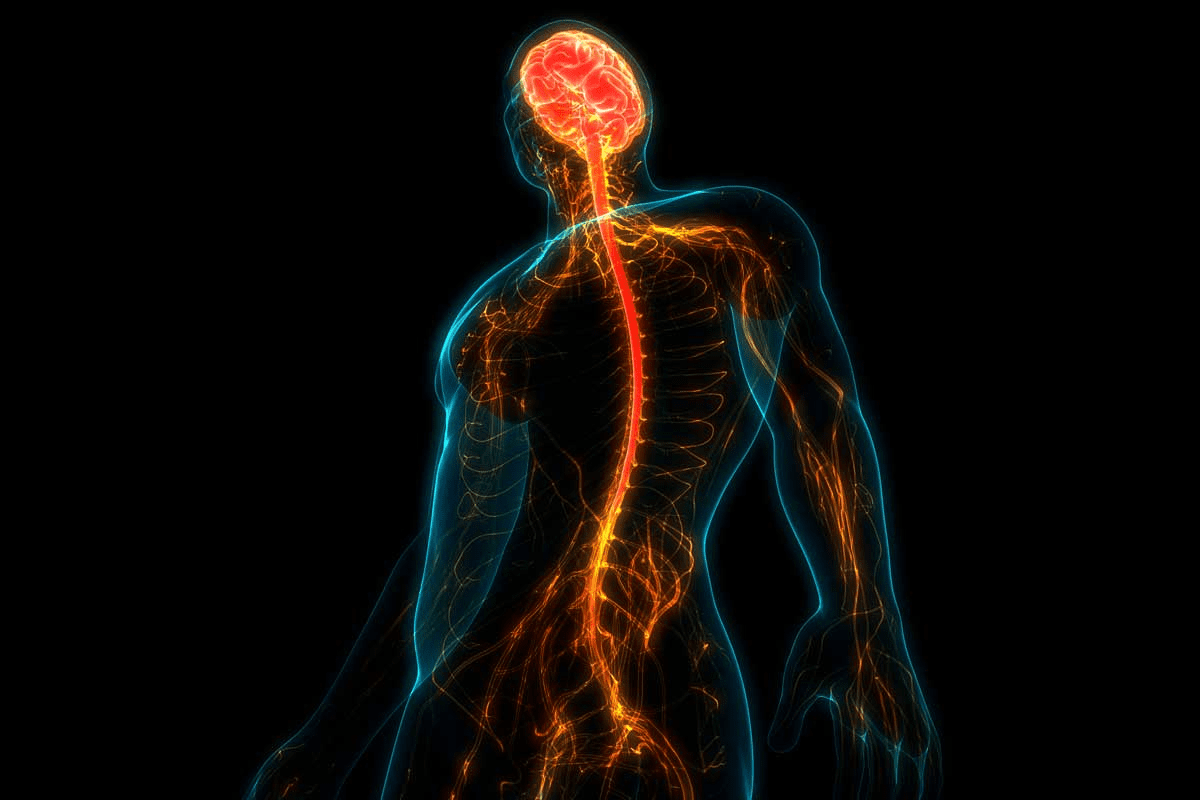
Autoimmune eye diseases happen when the immune system attacks the eyes. This leads to inflammation and can cause serious vision problems. The eyes have delicate parts like the retina, optic nerve, and cranial nerves that are needed for clear vision.
There are more than 80 types of autoimmune diseases, and many can affect the eyes. These diseases are hard to diagnose because they can show up in different ways.
How Autoimmune Conditions Affect the Eyes
Autoimmune conditions can harm the eyes in many ways. The immune system’s attack can cause inflammation in the eye’s tissues. This inflammation can lead to mild discomfort or even severe vision loss.
Autoimmune diseases cause inflammation in the body, which can affect the eyes. Conditions like uveitis, Sjögren’s syndrome, and rheumatoid arthritis can harm the eyes. This shows why eye care is important when managing autoimmune diseases.
Common Symptoms Across Autoimmune Eye Conditions
While symptoms can vary, some common ones include dry eyes, feeling like something is in your eye, sensitivity to light, pain, and changes in vision. Spotting these symptoms early is key to getting the right medical care and avoiding long-term damage.
Some common symptoms across various autoimmune eye conditions include:
- Dryness and irritation
- Sensitivity to light
- Blurred vision
- Eye pain or discomfort
- Redness of the eyes
By knowing these symptoms, patients and doctors can better manage autoimmune eye diseases.
Red Eyes and Autoimmune Disease: The Critical Connection

Red eyes and autoimmune disease are closely linked. Many autoimmune conditions can cause eye redness. This includes Sjögren’s syndrome, lupus, and rheumatoid arthritis.
Why Red Eyes Are a Common Symptom
Red eyes are common in several autoimmune diseases. This is because of inflammation and an immune system gone wrong. When the immune system attacks healthy tissues, it can cause eye inflammation. This leads to redness, irritation, and discomfort.
Autoimmune diseases often show eye symptoms, like red eyes. This can be a sign of a serious condition that needs medical help.
Distinguishing Autoimmune Red Eyes from Other Causes
Red eyes can have many causes, like allergies or infections. But autoimmune-related red eyes often have more symptoms. These include dryness, pain, light sensitivity, or vision problems.
Symptom | Autoimmune Cause | Other Causes |
Redness | Inflammation due to autoimmune disease | Allergies, infections, irritants |
Dryness | Sjögren’s syndrome, rheumatoid arthritis | Environmental factors, screen time |
Pain | Uveitis, lupus | Trauma, infection |
When to Seek Medical Attention for Red Eyes
If you have red eyes that don’t go away and are painful, you should see a doctor. Early treatment can stop serious problems and help you feel better.
See an eye doctor or a rheumatologist if you think your red eyes are from an autoimmune disease. They can check you thoroughly and create a treatment plan just for you.
Sjögren’s Syndrome: The Dry Eye Disease
Sjögren’s syndrome is an autoimmune disease that causes gland inflammation. It often leads to dry eyes. This condition makes life harder for those who have it, so it’s important to know about its effects on the eyes.
Impact on the Eyes
Sjögren’s syndrome makes eyes dry by inflaming the tear glands. This inflammation lowers tear production, causing dry, sore eyes. It can also lead to other eye problems, such as:
- Sensations of grittiness or sand in the eyes
- Burning or stinging sensations
- Blurred vision
- Eye fatigue
Because Sjögren’s is chronic, managing dry eyes is a long-term effort. It requires medical treatment and changes in daily life.
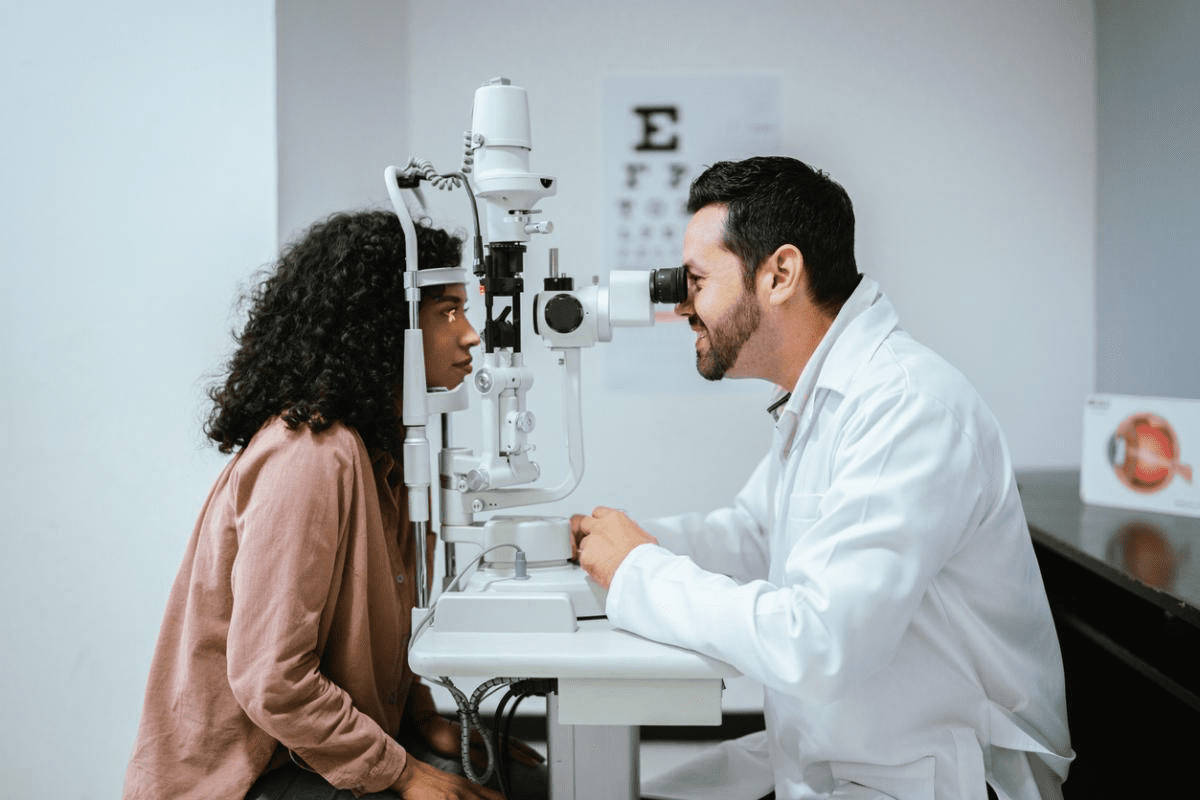
Diagnosing Sjögren’s-Related Eye Problems
Diagnosing Sjögren’s syndrome involves several steps. These include a doctor’s evaluation, patient history, and specific tests. For eye symptoms, doctors might use:
- Schirmer’s test to measure tear production
- Slit-lamp examination to check for eye damage
- Ocular surface staining to see damage
Getting a correct diagnosis is key to finding the right treatment. This helps manage dry eyes and other eye problems caused by Sjögren’s syndrome.
Treatment Options for Sjögren’s Dry Eyes
There are many ways to manage dry eyes in Sjögren’s syndrome. These include:
- Artificial tears and eye drops to help with tear production
- Punctal plugs to keep tears in the eyes
- Anti-inflammatory medicines to reduce inflammation
- Changes in daily life, like avoiding dry places and keeping eyes clean
In serious cases, doctors might suggest stronger treatments. These could be immunosuppressive therapy or biologic agents to fight the autoimmune disease.
Uveitis: Inflammation of the Eye’s Middle Layer
Uveitis is a big reason for preventable blindness worldwide. It’s important to get medical help quickly. This condition affects the uvea, the middle layer of the eye. It includes the iris, ciliary body, and choroid.
Types and Symptoms
Uveitis is divided into types based on where it affects the uvea. Anterior uveitis is the most common, hitting the iris. It’s often linked to ankylosing spondylitis. Intermediate uveitis targets the ciliary body, and posterior uveitis hits the choroid. Panuveitis affects all layers.
Symptoms vary by type but include eye pain, redness, and sensitivity to light. You might also see blurred vision and floaters. Spotting these signs early is key for treatment.
Autoimmune Causes
Uveitis often comes with autoimmune diseases. For example, ankylosing spondylitis, psoriatic arthritis, and inflammatory bowel disease raise the risk. Knowing these links helps manage uveitis better.
Current Treatments and Management
The main goal is to cut down inflammation and ease symptoms. Doctors use corticosteroids, either on the eye or taken by mouth. For severe cases, immunosuppressive drugs might be needed.
It’s important to have a full treatment plan. This should help eye symptoms and overall health. Regular eye checks are key to keeping vision safe.
Graves’ Disease and Thyroid Eye Disease
Graves’ disease is an autoimmune disorder that affects the thyroid gland. It can cause thyroid eye disease, a condition that impacts the eyes. Thyroid eye disease leads to inflammation and swelling around the eye in some patients.
Understanding the Eye-Thyroid Connection
The thyroid gland and eyes are connected in a complex way. In Graves’ disease, the immune system attacks the thyroid gland, causing hyperthyroidism. This can also affect the eye tissues, leading to thyroid eye disease.
The exact reasons are not fully known. But it’s thought that the same antigen causing Graves’ disease may also affect the orbital tissues. This leads to inflammation and swelling.
Recognizing Thyroid Eye Disease Symptoms
Symptoms of thyroid eye disease include bulging eyes (exophthalmos), double vision (diplopia), and eye discomfort. In severe cases, it can cause vision loss due to optic neuropathy. It’s important to notice these symptoms early for timely treatment.
- Bulging eyes or proptosis
- Double vision or diplopia
- Eye pain or discomfort
- Redness or inflammation of the eyes
- Sensitivity to light
Treatment Options and Visual Prognosis
Treatment for thyroid eye disease depends on how severe it is. Options include using lubricating eye drops and corticosteroids. In severe cases, surgery may be needed.
Surgical options include orbital decompression to relieve pressure on the optic nerve. They also include surgery to correct eyelid retraction or strabismus.
The visual prognosis varies for patients with thyroid eye disease. With the right treatment, many see a big improvement. But some may face ongoing issues. This shows the need for thorough care and follow-up.
Rheumatoid Arthritis and Its Ocular Manifestations
Rheumatoid arthritis is more than just a joint disease. It can also harm your eyes. This chronic autoimmune condition can cause various eye problems. So, getting your eyes checked regularly is key to managing RA.
Ocular Implications of RA
Rheumatoid arthritis can impact your eyes in different ways. One common issue is dry eyes. This happens when inflammation lowers tear production. It can make your eyes feel dry, blurry, and more prone to infections.
Another serious eye problem caused by RA is scleritis. It’s an inflammation of the sclera, the white part of your eyeball. Scleritis can cause a lot of pain, redness, and vision problems if not treated quickly.
Dry Eyes and Other Common Symptoms
Dry eyes are a common problem for RA patients. But, they might also face other eye issues. These include:
- Corneal thinning or ulcers
- Uveitis, an inflammation of the uvea, the middle layer of the eye
- Retinal vasculitis, inflammation of the blood vessels in the retina
These conditions highlight the need for regular eye exams for RA patients. This helps catch and treat any eye problems early.
Managing Eye Health with Rheumatoid Arthritis
Managing eye health for RA patients needs teamwork between rheumatologists and eye doctors. Treatment plans might include:
- Lubricating eye drops for dry eyes
- Anti-inflammatory medications for scleritis and uveitis
- Immunosuppressive drugs to control the underlying autoimmune condition
By working together, healthcare providers can help RA patients keep their eyes healthy. This improves their overall well-being.
Multiple Sclerosis and Optic Neuritis
Multiple sclerosis is a chronic autoimmune disease. It often shows up with optic neuritis, which inflames the optic nerve. This can cause vision problems, making it a big worry for those with MS.
Understanding Optic Neuritis in MS
Optic neuritis is when the optic nerve gets inflamed. It can cause pain, vision loss, and other vision issues. For people with MS, optic neuritis is a common sign, often one of the first symptoms.
The damage in optic neuritis in MS is due to demyelination. This is when the myelin sheath around the optic nerve gets damaged. This damage stops visual signals from being sent properly, causing the symptoms of optic neuritis.
Recognizing Vision Changes and Warning Signs
People with MS should watch out for signs of optic neuritis. These include:
- Vision loss, which can range from mild to severe
- Pain on eye movement
- Color desaturation
- Visual field defects
Spotting these symptoms early is key for quick treatment and management.
Treatment Approaches for MS-Related Eye Problems
Treating optic neuritis in MS usually means using corticosteroids to fight inflammation. Sometimes, intravenous corticosteroids are given to help the recovery speed up.
Treatment Approach | Description | Benefits |
Corticosteroids | Reduce inflammation | Help recovery, lessen symptoms |
Intravenous Corticosteroids | High-dose corticosteroids given through a vein | Quickly reduce inflammation, faster recovery |
Vision Therapy | Rehab programs to boost visual function | Improve vision, better quality of life |
We stress the need for quick medical help if optic neuritis symptoms show up. Early treatment can greatly help keep vision intact.
Behçet’s Disease: The Multi-System Eye Condition
Behçet’s disease affects many parts of the body, often causing severe eye inflammation. It’s a chronic condition that leads to inflammation in blood vessels. This can happen in the eyes, skin, and mucous membranes.
Ocular Symptoms
The eye symptoms of Behçet’s disease vary. They can include uveitis, retinal vasculitis, and other eye inflammation. Uveitis is a common symptom, causing inflammation in the eye’s middle layer.
People with Behçet’s may feel eye pain, have blurry vision, or be sensitive to light. If not treated, these symptoms can cause serious vision loss.
Diagnostic Challenges
Diagnosing Behçet’s disease is hard because of its complex symptoms. Doctors look at many signs, like oral and genital ulcers, skin lesions, and eye inflammation. This helps them make an accurate diagnosis.
To diagnose, doctors use a mix of clinical checks, patient history, and lab tests. Early diagnosis is key to avoid long-term damage, like eye damage.
Symptom | Frequency | Clinical Significance |
Oral ulcers | Common | Often the first symptom to appear |
Genital ulcers | Frequent | Can be painful and slow to heal |
Uveitis | Common | Can lead to vision loss if untreated |
Managing Eye Inflammation
Managing eye inflammation in Behçet’s disease needs a detailed plan. Doctors use corticosteroids and other drugs to reduce inflammation. This helps prevent damage to tissues.
Regular eye check-ups by an ophthalmologist are also key. Biologic agents are being studied as new treatments. They offer hope for those with severe or hard-to-treat disease.
Lupus and Its Effects on Eye Health
Systemic lupus erythematosus (SLE) affects many parts of the body, including the eyes. It can cause a range of eye problems, from mild to serious. These issues can threaten your vision.
Ocular Manifestations of Lupus
Lupus can show up in the eyes in different ways. Common problems include dry eyes, retinal vasculitis, and optic neuritis. These happen because lupus makes the immune system attack its own tissues.
Dry Eyes: Many lupus patients have dry eyes. This is when the eyes don’t make enough tears. It can cause discomfort and vision issues.
Retinal Vasculitis: This is inflammation of the retina’s blood vessels. It can lead to vision loss if not treated quickly.
Optic Neuritis: This is inflammation of the optic nerve. It can cause pain and temporary vision loss in one eye.
The Connection Between Lupus Flares and Eye Symptoms
Lupus has periods called flares where symptoms get worse. Eye symptoms can also get worse during these times. It’s important to manage them carefully to avoid lasting damage.
It’s key to watch your eye health during lupus flares. If you notice any vision or eye comfort changes, tell your doctor right away.
Protecting Your Vision When You Have Lupus
Managing lupus well is important for your eye health. Stick to your treatment plan, go to regular doctor visits, and report any eye symptoms.
Eye Condition | Symptoms | Management |
Dry Eyes | Dryness, irritation, blurred vision | Artificial tears, rest, avoiding irritants |
Retinal Vasculitis | Vision loss, floaters | Corticosteroids, immunosuppressive therapy |
Optic Neuritis | Pain, vision loss in one eye | Corticosteroids, monitoring for recovery |
Understanding how lupus affects the eyes and taking steps to protect them can help. This way, people with lupus can keep their vision and overall health safe.
Conclusion: Managing Autoimmune Eye Conditions Effectively
Managing autoimmune eye conditions needs a full plan. This includes medical care, lifestyle changes, and regular check-ups. We’ve looked at diseases like Sjögren’s syndrome and Graves’ disease. We’ve also talked about treatments for these conditions.
Handling these eye diseases means working together. It’s about keeping your vision sharp and improving your life. Knowing how autoimmune diseases affect your eyes is key. This knowledge helps you protect your sight and health.
It’s vital to keep an eye on your condition and adjust treatments as needed. Working with your healthcare team is key. This way, you can live well with autoimmune eye diseases.
FAQ
What are autoimmune eye diseases?
Autoimmune eye diseases happen when the body’s immune system attacks the eyes. This leads to inflammation and can cause serious vision problems. These diseases can affect different parts of the eye, like the cornea, uvea, retina, and optic nerve.
What are the common symptoms of autoimmune eye diseases?
Symptoms include dry eyes, feeling like something is in your eye, sensitivity to light, pain, redness, and vision changes. The symptoms depend on the disease and the eye part affected.
How does Sjögren’s syndrome affect the eyes?
Sjögren’s syndrome causes severe dry eye. This is because the tear glands are inflamed, leading to less tear production. It can also damage the eye surface severely.
What is uveitis, and how is it related to autoimmune diseases?
Uveitis is an inflammation in the eye’s middle layer. It’s often linked to autoimmune diseases like rheumatoid arthritis, lupus, and Behçet’s disease. Symptoms include eye pain, redness, and vision issues.
How does Graves’ disease affect the eyes?
Graves’ disease can lead to thyroid eye disease. This causes bulging eyes, double vision, and light sensitivity. It’s due to inflammation and swelling around the eye.
Can rheumatoid arthritis affect the eyes?
Yes, rheumatoid arthritis can cause eye problems. These include dry eyes, corneal thinning, and uveitis. This is because of the inflammation from the disease.
What is the connection between multiple sclerosis and optic neuritis?
Multiple sclerosis can lead to optic neuritis. This is an inflammation of the optic nerve. Symptoms include vision loss, eye pain, and color changes.
How does Behçet’s disease affect the eyes?
Behçet’s disease can cause severe eye inflammation. This includes uveitis and retinal vasculitis. Without proper care, it can lead to serious vision problems.
What are the ocular manifestations of lupus?
Lupus can cause eye issues like dry eyes, retinal vasculitis, and optic neuritis. This is due to the inflammation from the disease.
How can I protect my vision if I have an autoimmune disease?
To protect your vision, manage your autoimmune disease well. Follow a healthy lifestyle and get regular eye care. Always tell your doctor about any eye symptoms.
Are autoimmune eye diseases treatable?
Yes, many autoimmune eye diseases can be treated. The right treatment includes medicines to reduce inflammation and manage symptoms. The treatment plan depends on the disease and eye involvement.
What is the importance of seeking medical attention for autoimmune eye disease symptoms?
Getting medical help quickly is key to avoid vision loss and manage symptoms. Early treatment can greatly improve outcomes for those with autoimmune eye diseases.
References
National Center for Biotechnology Information. Autoimmune Eye Diseases: Symptoms and Treatment. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8593335/