Last Updated on October 31, 2025 by Saadet Demir

Renal artery stenosis is a serious condition where the arteries to your kidneys narrow. This is often due to atherosclerosis. If not treated, it can cause chronic kidney disease or kidney failure. We know how worried and confused you might be about this. Can renal bypass surgery reverse renal artery stenosis? Our ultimate guide explains the procedure and its amazing success rates.
At Liv Hospital, we have advanced treatments, including renal bypass surgery, for renal artery stenosis. Studies show that surgery can cure or greatly improve hypertension in about 58 percent of cases. This shows that surgery might reverse the condition.
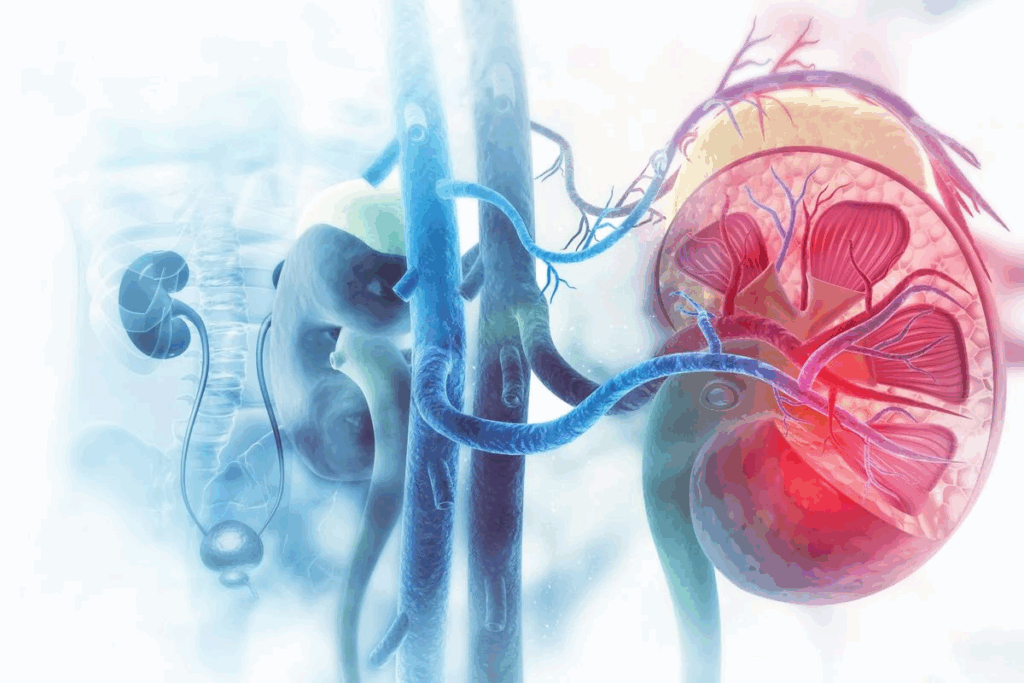
Renal artery stenosis is a serious condition where the renal arteries narrow. These arteries are key because they carry blood to the kidneys. If they narrow, it can harm kidney function and lead to severe health issues.
Renal artery stenosis is when one or both renal arteries narrow. This can cut down blood flow to the kidney. It starts a chain of reactions, including high blood pressure.
The main causes are atherosclerosis and fibromuscular dysplasia. Knowing the cause helps doctors choose the right treatment.
Atherosclerosis is the main reason for renal artery stenosis. It’s when plaque builds up in arteries. Fibromuscular dysplasia is another cause, affecting the renal arteries.
Smoking, high blood pressure, diabetes, and high cholesterol increase the risk. Older people are more likely to get it because atherosclerosis gets worse with age.
The early signs of renal artery stenosis can be hard to spot. As it gets worse, symptoms like high blood pressure and kidney problems appear. In severe cases, it can cause sudden lung swelling.
Some people might also feel pain in their flank or see a drop in kidney function. The symptoms can differ from person to person, making it hard to diagnose without tests.
The symptoms of renal artery stenosis include uncontrolled hypertension and kidney dysfunction. Catching it early is key to managing it well.

Healthcare professionals use many methods to diagnose renal artery stenosis. They do a clinical check-up, imaging studies, lab tests, and functional assessments. These help figure out how bad the stenosis is and its effect on the kidneys.
Imaging is key in diagnosing renal artery stenosis. We use different imaging methods to see the renal arteries and check the stenosis level.
Laboratory tests are vital for checking kidney function and spotting complications of renal artery stenosis. Common tests include:
These tests help us understand how renal artery stenosis affects kidney function. They guide our treatment choices.
Functional assessments are important for figuring out how much renal artery stenosis affects kidney function. Techniques like renal artery duplex ultrasound and captopril renography help assess this impact.
“The use of functional assessments in diagnosing renal artery stenosis allows us to tailor treatment strategies to individual patient needs, improving outcomes.”
– Expert in Vascular Surgery
By combining imaging, lab tests, and functional assessments, we can fully diagnose and assess renal artery stenosis. This helps us choose the right treatment and management plans.
Renal artery stenosis can cause many problems, like high blood pressure and kidney damage. It affects the renal arteries, which carry blood to the kidneys. This impacts how well the kidneys work and how blood pressure is controlled.
Hypertension in renal artery stenosis comes from less blood flow to the kidneys. The kidneys think they need more blood and start the RAAS system. This makes blood vessels narrow and blood pressure go up. This is a way the body tries to keep enough blood flowing to the kidneys. But, it can lead to high blood pressure that doesn’t go away.
Renal artery stenosis can harm the kidneys over time because of less blood flow. This makes it hard for the kidneys to work right. It can lead to chronic kidney disease or even kidney failure if not treated. The kidneys are very sensitive to not getting enough oxygen. It’s important to watch how the kidneys are doing in patients with this condition.
The heart and blood vessels also suffer from renal artery stenosis. The high blood pressure it causes can lead to heart failure, heart disease, and stroke. The connection between renal artery stenosis, kidney health, and heart health shows why treating it fully is key.
It’s vital to understand how renal artery stenosis affects the kidneys and blood pressure. By tackling its many effects, doctors can help patients get better and avoid serious problems later on.
Many patients with renal artery stenosis find relief without surgery. We use a mix of medications, lifestyle changes, and monitoring. This helps decide when more treatment is needed.
Medicines are key in managing renal artery stenosis. They help control blood pressure and lower heart disease risk. Antihypertensive drugs are used to keep blood pressure in check. Statins help lower cholesterol, which also reduces heart disease risk.
But, medicines alone can’t fix the stenosis. We keep a close eye on how well treatment is working. This way, we can adjust the plan as needed.
Changing your lifestyle is vital in managing renal artery stenosis. Eating a heart-healthy diet full of fruits, veggies, whole grains, and lean proteins helps. Regular physical activity, like walking, also boosts heart health.
“Adopting a healthy lifestyle can significantly impact the management of renal artery stenosis, reducing the risk of progression and related cardiovascular events.”
Even with non-surgical methods, some patients need more help. We then look at other options, like surgery or endovascular procedures. These methods directly tackle the stenosis.
It’s important to watch for signs of worsening kidney function or high blood pressure. If conservative treatment doesn’t work, we act quickly. This can prevent serious damage in the long run.
Renal bypass surgery is a complex procedure. It involves grafting a healthy artery onto the renal arteries to bypass a blockage. This technique treats renal artery stenosis, a condition that can cause high blood pressure and kidney damage.
The surgery starts with an incision in the abdomen to reach the renal arteries. We use different techniques based on the patient’s anatomy and the stenosis location. The goal is to improve blood flow to the kidneys, easing symptoms and preventing damage.
There are various methods for this surgery, including using grafts from the patient or synthetic ones. The choice depends on the patient’s health, other vascular diseases, and the surgeon’s preference.
The type of graft used can differ. Autologous grafts, like those from the saphenous vein or internal iliac artery, are often chosen for their biocompatibility and lower risk of complications. Synthetic grafts, made from materials like Dacron or Gore-Tex, are used when autologous grafts are not possible.
Autologous grafts have a lower risk of infection and better success rates. But, they need an extra surgical site for harvesting. Synthetic grafts are readily available and don’t need a second site, but they might have a higher risk of complications.
During surgery, several key considerations are important for success. Monitoring blood flow and pressure in the renal arteries is critical to ensure the graft works well. We also prevent ischemia-reperfusion injury, which can happen when blood flow returns to the kidney after a period of lack of blood.
Intraoperative imaging, like angiography, may be used to check the graft and renal arteries. This helps fix any problems right away, ensuring the best outcome for the patient.
Endovascular interventions have changed how we treat renal artery stenosis. They offer a less invasive option compared to traditional surgery. These methods help restore blood flow to the kidneys, improving function and controlling blood pressure.
We will look at the different endovascular techniques for treating renal artery stenosis. This includes renal balloon angioplasty, kidney artery stenting, and new endovascular technologies. Each method has its own benefits and risks.
Renal balloon angioplasty uses a catheter with a balloon to widen the narrowed renal artery. The balloon is inflated to improve blood flow. This method is often paired with stenting to keep the artery open.
This technique is minimally invasive, has a quick recovery time, and can be done under local anesthesia. But, it might not work for everyone, like those with complex or calcified lesions.
Kidney artery stenting involves placing a stent to keep the artery open after angioplasty. Stenting has been shown to improve long-term success rates compared to angioplasty alone.
| Procedure | Benefits | Potential Complications |
| Renal Balloon Angioplasty | Minimally invasive, quick recovery | Restenosis, artery damage |
| Kidney Artery Stenting | Improved patency rates, reduced restenosis | Stent thrombosis, bleeding |
New technologies, like drug-coated balloons and advanced stenting systems, are being studied. These innovations aim to lower restenosis rates and make procedures more durable.
The field of endovascular interventions for renal artery stenosis is rapidly evolving. As technology improves, we can expect better and safer treatments. This brings new hope to those with this condition.
Choosing the right patients for surgery to fix renal artery stenosis is key. We look closely at each patient to see who will do best with surgery or other treatments.
Renal bypass surgery is best for those with severe blockages in their renal arteries. Ideal candidates have high blood pressure that’s hard to control and signs of kidney damage. We also look at patients who have tried other treatments without success or have complex anatomy.
For example, someone with a very narrow artery (>70%) and high blood pressure that won’t go down might need surgery. Also, those with stenosis caused by fibromuscular dysplasia might do well with surgery.
For patients with less severe blockages, endovascular treatments like stenting are often better. Best candidates have blockages that are not too long, have high blood pressure that started recently, and have little kidney damage. We also consider those at high risk for surgery or with a short life expectancy.
Not everyone is a good fit for surgery. Patients with serious health problems, like heart disease or severe kidney issues, face high risks. Also, those with a short life expectancy or unlikely to benefit from surgery are not good candidates.
We look at each patient’s health, medical history, and how bad their blockage is to decide the best treatment. This way, we make sure our patients get the best care for their needs.
Revascularization procedures are a key treatment for renal artery stenosis. They offer hope to those with this condition. These procedures improve blood pressure, kidney function, and last long.
Research shows that revascularization can cure or greatly improve high blood pressure in about 58% of patients. This is a big deal, showing that over half of those treated see a big drop in their blood pressure.
A study on renal artery stenting and angioplasty found success rates of up to 98% in the right candidates. This shows that these procedures can effectively lower blood pressure and do so with great success.
Key statistics on hypertension improvement include:
Revascularization also helps improve kidney function. While results vary, many studies show that kidney function can stabilize or even improve after the procedure.
The chance of kidney function recovery depends on several things. These include how long and severe the stenosis is, and the patient’s starting kidney health.
The long-term success of revascularization is very important. Many factors can affect how long the procedure works. These include the type of procedure, the stent material, and the patient’s health.
“The durability of revascularization procedures is key to their success. It directly affects patients’ long-term health.”
— Expert in Vascular Surgery
Recent studies show that both surgical bypass and endovascular procedures can be long-lasting solutions for renal artery stenosis. This is true if the right patients are chosen and the procedure is done correctly.
Long-term outcomes are influenced by:
Knowing what affects the reversibility of renal artery stenosis is key. The chance of success depends on several important factors. We will look at these in this section.
The length and severity of renal artery stenosis matter a lot. Those with the disease for a shorter time and with less severe stenosis have a better chance of recovery. Early treatment can make a big difference.
Early detection is vital for better outcomes. Finding the disease early means we can start treatment before it causes too much damage. This increases the chances of successful reversal.
Age and other health issues also play a big role. Older patients or those with many health problems may face more risks during treatment. They might also have a harder time recovering.
Looking at the patient’s overall health is important. Patients with serious health issues, like diabetes or heart disease, need a careful treatment plan. This plan must consider their health and the risks of treatment.
The kidney’s function before treatment is also key. Patients with better kidney function tend to do better after treatment.
Checking the kidney function helps us know how well a patient might recover. For those with very poor kidney function, treatment goals might change. The focus might shift to managing symptoms and slowing the disease’s progress.
In summary, many factors affect whether renal artery stenosis can be reversed. These include how long and severe the disease is, the patient’s age and health, and their kidney function. Understanding these factors helps us create treatment plans that meet each patient’s unique needs.
Renal artery stenosis treatment needs a good recovery plan. This plan is key for the best results.
Patients are watched closely after surgery. They are in a recovery unit. Here, their vital signs, pain, and any complications are monitored.
Key aspects of immediate post-surgical care include:
After surgery, medication changes are made. These changes help with pain, prevent issues, and control blood pressure. Patients might take anticoagulants, antiplatelet agents, or other drugs to aid in recovery.
The table below shows common medication changes after renal artery stenosis treatment:
| Medication Type | Purpose | Duration |
| Anticoagulants | Prevent blood clots | Several weeks to months |
| Antiplatelet agents | Prevent platelet aggregation | Long-term, sometimes lifelong |
| Antihypertensives | Manage blood pressure | Ongoing, adjusted as necessary |
Patients are told to avoid strenuous activities. This includes heavy lifting and bending.
Gradually, patients can return to their normal activities as their doctor advises. A follow-up care plan is key to track progress and make changes as needed.
By sticking to a detailed post-operative care plan, patients can improve their health after renal artery stenosis treatment.
Treating renal artery stenosis requires knowing the risks of surgery and endovascular procedures. It’s important to understand these risks and how to reduce them.
Surgery for renal artery stenosis, like renal bypass, has risks. These include bleeding, infection, and damage to surrounding tissues. There’s also a chance of restenosis, where the artery narrows again.
To lower these risks, it’s vital to carefully choose patients and plan surgeries well. This means checking the patient’s health, the stenosis’s severity, and any surgery contraindications.
Endovascular treatments, like angioplasty and stenting of kidney arteries, have risks too. These include vascular injury, contrast-induced nephropathy, and stent thrombosis. There’s also a chance of restenosis within the stent.
To reduce these risks, precise techniques and careful patient preparation are needed. Using embolic protection devices during angioplasty and stenting can also help.
Effective risk management is essential for treating renal artery stenosis well. This includes a detailed patient evaluation, choosing the best treatment, and precise procedural techniques.
By understanding complications and using strategies to reduce risks, we can improve treatment outcomes for patients with renal artery stenosis.
Renal artery stenosis is a serious condition that needs quick treatment. This is to prevent more kidney damage and ease symptoms. We’ve looked at how to diagnose it, its effects on kidneys and blood pressure, and treatment options.
Treatment options include non-surgical methods and surgery. Surgery, like renal bypass surgery, can help control blood pressure. It might even reverse the condition. Knowing what affects the condition’s reversibility helps doctors choose the best treatment.
In short, treatment for renal artery stenosis must fit each patient’s needs. This includes looking at how severe the disease is, the patient’s age, and any other health issues. With the right care and support, patients can have better outcomes and a better quality of life.
Renal artery stenosis is when the arteries to the kidneys get narrow. This can lead to kidney disease or failure if not treated.
Surgery like renal bypass can help symptoms. It might reverse the condition, depending on the disease’s severity and patient factors.
Plaque buildup in the artery is a main cause. Risk factors include high blood pressure, atherosclerosis, and heart conditions.
Doctors use Doppler ultrasound and CT scans for diagnosis. They also check kidney function and assess the condition’s severity.
Treatments include medication and lifestyle changes. Surgery like renal bypass and endovascular procedures are also options.
It’s a surgery that bypasses the narrowed part of the renal artery. This restores blood flow to the kidneys.
The surgery can ease symptoms and improve kidney function. Success rates vary based on patient factors.
Recovery includes post-surgery care, medication changes, and rest. The goal is to get back to normal life.
Complications include surgery risks and endovascular procedure issues. Proper patient selection can minimize these risks.
Yes, a healthy diet and exercise can manage the condition. They can also ease symptoms.
It can cause high blood pressure and kidney damage. This highlights the need for prompt treatment.
It’s a procedure where a stent is placed in the narrowed artery. This restores blood flow to the kidneys.
Success rates vary by patient. These procedures can improve blood pressure and kidney function, and are durable.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us