Last Updated on November 27, 2025 by Bilal Hasdemir

Prostate cancer is a big problem worldwide, affecting millions of men. Robotic prostate surgery is a top choice for treatment. In the U.S., over 200,000 men get prostate cancer each year. Many of them choose robotic surgery for the prostate.
It’s important for patients and their families to understand this surgery. Knowing the patient’s position during surgery is key. We’ll look into what happens during a prostatectomy procedure.
Exploring robotic prostatectomy shows how the patient’s position matters. It’s vital for the surgery’s success.
Key Takeaways
- Robotic prostate surgery is a common treatment for prostate cancer.
- The patient’s position during surgery is key to success.
- Knowing the procedure can ease patient worries.
- Robotic prostatectomy has many benefits over the old methods.
- Patient positioning is a critical part of surgery.
The Evolution of Robotic Prostatectomy
Robotic prostatectomy has changed a lot over time. It has moved from old open surgery to new robotic-assisted methods. These changes have brought better technology and better results for patients.
From Open Surgery to Robotic Assistance
Old prostatectomy surgeries needed big cuts and took longer to heal. Robot-assisted laparoscopic prostatectomy changed this with a new, small cut method. This method uses robots to help surgeons work more accurately and lose less blood.
This move to robots has brought many benefits. Patients get smaller cuts, less pain, and heal faster. This makes robotic radical prostatectomy a top choice for many.
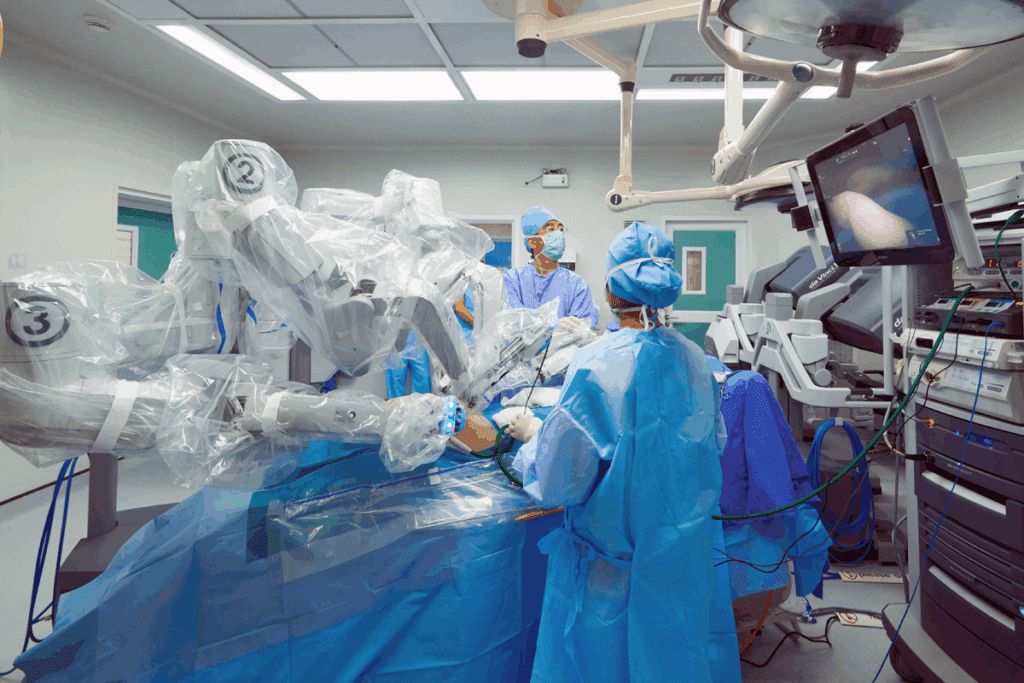
The Da Vinci Surgical System
The Da Vinci Surgical System is a key robot for prostate surgeries. It gives surgeons better views, control, and precision. The Da Vinci’s intuitive interface lets surgeons move instruments like they’re in the patient’s body.
Why Robotic Approaches Have Become Standard
Robot-assisted prostatectomy is now more common because it’s better for patients. It leads to fewer problems and better results than the old surgery. So, robot-assisted laparoscopic prostatectomy is now the main choice in urology.
Robot technology keeps getting better. This will make prostate surgeries even safer and more precise. It will keep robotic methods a key part of treating prostate cancer.
The Steep Trendelenburg Position Explained
The Steep Trendelenburg position is key in robotic prostatectomy. It tilts patients in a way that might seem odd but is vital for success. This position is not just for convenience; it’s essential for precise and minimally invasive surgery.
What the Position Looks Like
In this position, patients lie on a table tilted so their feet are above their heads. The tilt is quite deep, usually between 25 to 30 degrees. The exact angle depends on the surgery’s needs and the patient’s body.
The table has special equipment to keep the patient in place. This is important because the tilt is steep, and safety is a top priority.
Why This Position Is Necessary
This position is needed because it makes it easier for surgeons to reach the pelvic area. By tilting the patient, the intestines move away from the prostate. This gives a clearer view and more space for the robotic tools.
This setup is critical for robotic prostatectomy success. It allows for precise prostate gland removal. Better access and visibility lower the risk of problems and improve patient outcomes.
Degree of Tilt Used During Surgery
The tilt angle for robotic prostatectomy usually ranges from 25 to 30 degrees. The exact angle depends on the patient’s body, the surgeon’s choice, and the surgery’s needs.
Surgeons and anesthesiologists work together to ensure the patient is safely positioned. They monitor the patient closely to adjust the tilt as needed and address any issues.
Patient Preparation for Positioning
Getting ready for robotic prostate surgery is more than just the surgery itself. It also means preparing for the special position needed during the operation. We help our patients get ready for the steep Trendelenburg position, which is key for the surgery.
Pre-surgical Discussions About Positioning
We talk a lot with our patients about the position they’ll be in during surgery. “Knowing what to expect can really help reduce anxiety and make the experience better,” says a top urologist. These talks are important for setting clear expectations and answering any questions patients might have.
We explain the steep Trendelenburg position and why it’s needed for the robotic prostatectomy. We also talk about how they’ll be kept safe in this position to avoid any movement during the surgery.
Physical Preparation Steps
Getting physically ready for robotic prostate surgery is a big part of the process. We tell our patients how to stay comfortable and lower the risk of problems related to positioning.
- Maintaining a healthy weight reduces pressure on joints and improves circulation.
- Doing exercises that strengthen the muscles, which will be strained during surgery.
- Avoiding hard activities before the surgery to make sure they’re well-rested.
Mental Preparation for the Experience
Mental preparation is just as important as physical preparation. We help our patients understand what will happen during the surgery. This includes explaining the safety straps and supports that will keep them in the Trendelenburg position.
By preparing patients both mentally and physically, we can make their surgery and recovery better. “A well-prepared patient tends to have a smoother surgery and recovery,” highlights the value of thorough pre-surgical preparation.
Securing the Patient During Robotic Prostatectomy
Keeping the patient stable is key during robotic surgery. We take many steps to keep the patient safe during robotic prostatectomy. This ensures their safety from start to finish.
Positioning Devices and Supports
We use positioning devices and supports to keep the patient in the right spot. These include shoulder harnesses, leg rests, and side supports. They help keep the patient steady during the steep Trendelenburg position needed for robotic prostatectomy.
We plan and use these devices carefully to make sure the patient is both comfortable and secure. We also make sure to protect all pressure points to avoid injury.
Preventing Sliding During Steep Tilt
One big challenge in robotic prostatectomy is stopping the patient from sliding when tilted steeply. We use special anti-slip measures like non-slip mats and straps to keep the patient in place.
These steps are vital for keeping the patient’s position stable and safe during the surgery.
Protecting Pressure Points
It’s also important to protect pressure points during robotic prostatectomy. We use padding and cushioning to lower the risk of injuries from pressure.
By focusing on these areas, we can greatly reduce the chance of complications. This helps the patient recover more smoothly.
Physiological Effects of the Trendelenburg Position
When surgeons use the Trendelenburg position for robotic prostatectomy, they must consider how it affects the body. This position, which tilts the body steeply, impacts different systems in significant ways.
Cardiovascular Changes
The Trendelenburg position can change how blood flows in the body. Blood moves to the upper body, which can increase blood return to the heart. This might raise the heart’s output. Yet, it could also put extra pressure on the heart, which is risky for those with heart issues.
Some key changes include:
- Increased cardiac preload due to venous blood shift
- Potential increase in cardiac output
- Possible strain on the heart due to increased pressure
Respiratory Impacts
The Trendelenburg position also affects breathing. The pressure from the abdomen on the diaphragm can make it harder to breathe. This can lead to higher airway pressures and affect oxygen levels.
Key respiratory impacts include:
- Reduced lung volumes due to diaphragmatic displacement
- Increased risk of respiratory acidosis if not managed properly
- Potential need for adjustments in ventilation strategies
Neurological Considerations
The Trendelenburg position also has neurological effects. The head-down tilt can increase pressure in the brain, which is a concern for some patients. There’s also a risk of brain swelling and nerve damage if not managed well.
Some neurological considerations include:
- Increased intracranial pressure
- Risk of cerebral edema
- Potential for nerve compression or injury
In conclusion, the Trendelenburg position used in robotic prostatectomy has many physiological effects. These need careful management to ensure patient safety and the best outcomes. It’s important for surgeons and anesthesiologists to understand these effects to provide the best care.
The Complete Robotic Prostatectomy Procedure
The robotic prostatectomy procedure is a detailed surgical process. It includes several important steps. These steps range from the patient’s initial setup to the actual surgery, including nerve-sparing techniques.
Initial Positioning and Anesthesia
The first step is to position the patient on the operating table. They are placed in a steep Trendelenburg position. This allows the surgeon to easily access the prostate area. General anesthesia is administered to keep the patient comfortable and pain-free.
Port Placement and Robot Docking
After the patient is set up and under anesthesia, the team places ports in the abdomen. These small incisions are for the surgical instruments. The Da Vinci robotic system is then connected to these ports. This lets the surgeon control the instruments from a console.
Key Surgical Steps While in Position
With the robotic system ready, the surgeon starts the prostatectomy. They carefully dissect the prostate gland from the surrounding tissues. The robotic system’s high-definition visualization and precise control help in this delicate process.
The main steps are:
- Dissecting the prostate from the bladder and surrounding tissues
- Identifying and preserving nerves for urinary continence and erectile function
- Removing the prostate gland
- Reconstructing the bladder neck and urethra
Nerve-Sparing Techniques
Nerve-sparing techniques are key in robotic prostatectomy. These methods involve identifying and preserving the nerves next to the prostate gland. These nerves are vital for maintaining urinary and sexual functions. The robotic system’s precision helps surgeons perform these delicate steps accurately.
By saving these nerves, patients have a better chance of regaining their natural urinary and sexual functions after surgery. The surgeon’s skill in nerve-sparing techniques greatly impacts the patient’s quality of life post-procedure.
How Long You’ll Be in Position During Surgery
Knowing how long robotic prostate surgery lasts is key for patients. The time spent in the Trendelenburg position affects the surgery experience.
Average Duration of Robotic Prostate Surgery
Robotic prostate surgery usually lasts between 2 to 4 hours. This includes getting ready, the surgery, and the first part of recovery.
Factors That May Extend Time in Position
Several things can make surgery last longer. These include:
- Complexity of the case: More complex surgeries take longer.
- Patient anatomy: Different body shapes can affect surgery time.
- Surgeon experience: Even experienced surgeons may need more time for complex cases.
Surgeon Experience and Procedure Time
The surgeon’s experience greatly affects surgery time. More skilled surgeons often do surgeries faster, shortening the time needed.
In summary, robotic prostate surgery usually lasts 2 to 4 hours. But many factors can change this time. Knowing these can help patients prepare better for their surgery.
Potential Complications Related to Surgical Positioning
The way patients are positioned for robotic prostate surgery can cause several problems. This advanced surgery needs exact positioning to work well. But, this can lead to some issues. It’s key for patients and doctors to know these risks to get the best results.
Pressure-Related Injuries
One big risk is pressure injuries from the steep Trendelenburg position. Long-term pressure can hurt tissues and cause pain. Pressure sores are a big worry, mainly in spots where the body touches the table. We use special padding and supports to avoid these problems.
Nerve Compression Issues
Nerve compression is another issue. The way patients are positioned can sometimes harm nerves. This can cause numbness, tingling, or even nerve damage. Nerve compression issues can be lessened by careful positioning and using devices that reduce nerve pressure.
Respiratory and Circulatory Concerns
The steep Trendelenburg position can affect breathing and blood flow. It can press on the diaphragm, making breathing harder. It can also change blood pressure and flow. We watch patients’ vital signs closely during surgery to handle any breathing or blood flow problems right away.
Patient Experience of the Positioning
The way patients feel during robotic prostatectomy is very important. We look at how they see the steep Trendelenburg position needed for this surgery.
What Patients Report About the Experience
Patients usually feel safe and comfortable during surgery. The team’s careful setup and support help a lot. “I was worried about being tilted so much, but the staff made me feel secure,” one patient said.
Many patients feel the same way. They value good communication and care from the team.
Some might feel anxious or uncomfortable because of the position. But we help by talking to them before and during surgery. We make sure they know what to expect and listen to their worries.
Post-Operative Sensations Related to Positioning
After surgery, patients might feel stiff or sore. This is because of being in the Trendelenburg position for a long time. “I felt stiff, but it wasn’t too bad,” another patient said.
We help manage these feelings after surgery. We tell patients how to ease the discomfort with gentle exercises and pain relief.
Recovery from Position-Related Discomfort
It usually takes a few days to a week to get better from the discomfort. We suggest light activities to help with stiffness and blood flow. “Doing the exercises helped me recover faster,” a patient mentioned.
While some discomfort is normal, serious problems are rare if we follow the right steps. Our team works hard to keep risks low and ensure the best results for our patients.
Modifications to Standard Positioning for Special Cases
Robotic prostate surgery is very flexible. We adjust the position for obese patients, those with breathing problems, or musculoskeletal issues. Our team is trained to meet each patient’s unique needs for the best results.
Adaptations for Obese Patients
Obese patients need extra support and adjustments. Extra care is taken to secure the patient to the table to prevent movement during surgery.
We also watch for pressure points. We use extra padding and supports to prevent injuries from pressure.
Adjustments for Patients with Respiratory Issues
Patients with breathing problems need special care during surgery. Adjustments are made to the positioning to help their lungs and breathing.
Our team works with the anesthesia team to keep an eye on the patient’s breathing.
Accommodations for Musculoskeletal Conditions
Patients with musculoskeletal issues, like arthritis, get special attention. Careful consideration is given to the patient’s comfort and safety during surgery.
We use special equipment and techniques to reduce strain on their muscles and joints.
These adjustments help ensure all patients get top-notch care during robotic prostate surgery, no matter their needs.
Comparing Positions in Different Prostate Surgery Approaches
Prostate surgery uses several methods, like open, laparoscopic, and robotic. Each method needs a specific way of positioning. Knowing these differences helps us see how robotic surgery has improved.
Open Radical Prostatectomy Positioning
Open radical prostatectomy is done with the patient lying on their back. They are slightly bent to help reach the prostate. This method is simple but not as precise as newer techniques.
Laparoscopic Prostatectomy Positioning
Laparoscopic prostatectomy uses a Trendelenburg position. This is similar to robotic surgery. But the tilt and how the patient is secured can differ.
Advantages of Robotic Positioning
Robotic prostatectomy uses the Da Vinci Surgical System. It allows for detailed work in a steep Trendelenburg position. This setup improves vision and cuts down on recovery time.
| Surgical Approach | Patient Positioning | Key Advantages |
| Open Radical Prostatectomy | Supine with hyperextension | Traditional method, widely understood |
| Laparoscopic Prostatectomy | Trendelenburg position | Less invasive than open surgery |
| Robotic Prostatectomy | Steep Trendelenburg | Enhanced precision, reduced recovery time |
The table shows each method’s unique needs and benefits. Robotic surgery is special because of its precision and quick recovery.
A study in the Journal of Urology found robotic surgery to be better than the old methods. “Robotic-assisted laparoscopic prostatectomy has become a standard of care in many institutions due to its superior outcomes and reduced morbidity.”
Looking at different prostate surgery methods, robotic surgery is ahead. It offers better positioning and precision. As technology gets better, so will patient care and results.
Technological Advances in Positioning for Robotic Surgery
Technological advancements have changed how patients are positioned during robotic surgery. This has made the surgery safer and more effective. As robotic surgery grows, so does the technology for patient positioning.
Evolution of Positioning Systems
Positioning systems have been key to robotic surgery’s success. Early systems were simple, needing manual adjustments. But, as the field grew, so did the technology for positioning patients.
Today, positioning systems are advanced. They allow for precise adjustments during surgery. These systems work with robotic equipment to keep patients in the best position.
Modern Safety Enhancements
Safety is a top priority in robotic surgery. New positioning technology has greatly improved patient safety. Modern systems have many safety features, including:
- Advanced stabilization mechanisms to prevent movement during surgery
- Sensors to monitor patient position and detect any issues
- Automated adjustments to keep the patient in the best position
These features help reduce risks like nerve damage or pressure injuries.
| Safety Feature | Description | Benefit |
| Stabilization Mechanisms | Prevents patient movement during surgery | Reduces risk of complications |
| Position Monitoring Sensors | Monitors patient position in real-time | Early detection of issues |
| Automated Adjustments | Maintains optimal patient positioning | Improves surgical precision |
Future Developments in Patient Positioning
Robotic surgery is getting better, and so is patient positioning technology. We can expect more precise, safer, and more comfortable positioning in the future.
Future advancements might include artificial intelligence for real-time adjustments. They might also use new materials for better comfort and safety.
By exploring new possibilities in patient positioning, we can make robotic surgery even better for patients.
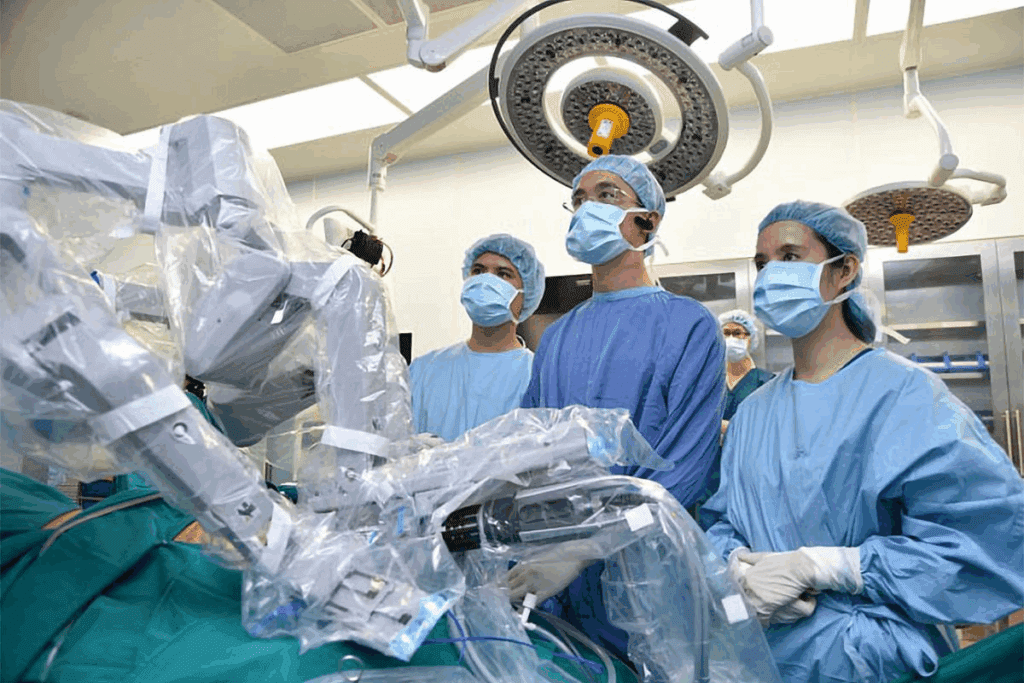
The Surgeon’s Perspective on Optimal Positioning
From the surgeon’s point of view, the right position is essential for a successful robotic prostatectomy. The steep Trendelenburg position is needed but must be managed carefully. This ensures the patient’s safety and the surgery’s success.
Ergonomic Considerations
Surgeons must think about ergonomic factors when setting the patient’s position. The robotic system allows for precise movements. But the surgeon needs to be comfortable and able to work the console well.
Ergonomic considerations include the height and position of the console, as well as the surgeon’s seating and hand positioning.
- Adjusting the console to fit the surgeon’s needs
- Ensuring proper hand positioning on the controls
- Maintaining a comfortable seating position
Visualization Advantages
Optimal positioning also improves visualization during the procedure. The robotic system offers a clear, 3D view of the surgical site. Proper patient positioning ensures this view is not blocked.
The steep Trendelenburg position helps to move the intestines away from the prostate, providing a clearer view.
The benefits of this visualization include:
- Better identification of anatomical structures
- More precise dissection and nerve-sparing techniques
- Enhanced ability to control bleeding
How Positioning Affects Surgical Outcomes
The patient’s position directly affects the outcomes of robotic prostatectomy. Proper positioning leads to more precise surgery. This can result in better cancer control and fewer complications.
It also makes nerve-sparing techniques easier, which can improve recovery and reduce the risk of incontinence and impotence.
Key factors that influence surgical outcomes include:
- The degree of Trendelenburg tilt
- The use of shoulder restraints to prevent sliding
- Careful padding of pressure points to prevent injury
Conclusion: Understanding Your Position During Robotic Prostate Surgery
Robotic prostate surgery has changed how we treat prostate cancer. It offers benefits like less invasive procedures and faster recovery times. The patient’s position on the table is key, usually in a steep Trendelenburg position. This helps the surgeon access the prostate area better.
We’ve looked at many parts of robotic prostate surgery in this article. This includes how it has evolved, how patients prepare, and the effects of the Trendelenburg position. Knowing about surgical positioning is important for patient education and care.
Patients can prepare better for surgery and recovery by learning about it. The advancements in robotic prostate surgery make it safer and more effective. These improvements include better positioning systems and safety features.
As medical technology advances, we aim to provide top-notch healthcare. Understanding robotic prostate surgery, including the importance of positioning, helps improve patient outcomes and satisfaction.
FAQ
What is robotic prostate surgery?
Robotic prostate surgery is a new way to treat prostate cancer. It uses the Da Vinci Surgical System. This system helps remove the prostate gland in a minimally invasive way.
What position are you in during robotic prostate surgery?
Patients lie on their backs with their head down and feet up. This is called the Steep Trendelenburg position. It’s about 30-40 degrees.
How long does a robotic prostatectomy take?
The surgery usually lasts 2-4 hours. It depends on the case’s complexity and the surgeon’s skill.
What are the benefits of robotic prostate surgery?
It has many benefits. These include smaller cuts, less blood loss, and fewer complications. Recovery is also faster than with traditional surgery.
How is the patient secured during robotic prostatectomy?
Patients are kept safe with special devices. These include shoulder harnesses and leg stirrups. They prevent sliding and protect pressure points.
What are the possible complications related to surgical positioning during robotic prostatectomy?
Complications can include injuries from pressure, nerve issues, and problems with breathing and blood flow. These are due to the Steep Trendelenburg position.
How do surgeons adapt the positioning for special cases, such as obese patients?
Surgeons adjust the position for special cases. For obese patients, they use extra supports. They also change the tilt for those with breathing problems.
What is the recovery time for robotic prostatectomy?
Recovery times vary. But most patients can get back to normal in a few weeks. Some recover faster than with traditional surgery.
How does the Da Vinci Surgical System improve surgical outcomes?
The Da Vinci System gives surgeons better vision and control. It allows for more precise and less invasive procedures.
What are the advantages of robotic positioning compared to other prostate surgery approaches?
Robotic positioning has many benefits. These include better vision, less blood loss, and less tissue damage. It’s better than open and laparoscopic surgeries.
What technological advances have been made in positioning for robotic surgery?
There have been many advances. These include better positioning systems and safety features. Ongoing research also improves outcomes in robotic surgery.
How does the surgeon’s experience impact the procedure time and outcome?
A surgeon’s experience is very important. More experienced surgeons do better and faster. They achieve better results and shorter surgery times.
Reference
- Hoshikawa, Y., et al. (2014). The effect of steep Trendelenburg positioning on ocular complications during robotic-assisted radical prostatectomy. British Journal of Ophthalmology, 98(3), 305-310. https://bjo.bmj.com/content/98/3/305