The eyes have a special shield called ocular immune privilege. It keeps the immune system from attacking them.Explanation of immune privilege andwhat happens if your immune system finds your eyes and attacks. The risk of rejection is high when what happens if your immune system finds your eyes.
This shield is key to keeping our vision safe. It stops the immune system from causing harm to our eyes.
At Liv Hospital, we understand how the immune system and eyes interact. This is a fascinating area in medicine. The same protection that keeps our vision safe can sometimes turn against us.
Key Takeaways
- The eyes have a unique protective mechanism called ocular immune privilege.
- This mechanism prevents the immune system from attacking the eyes.
- The relationship between the eye and the immune system is complex.
- Understanding this relationship is key to keeping our vision safe.
- Ocular immune privilege is vital for stopping immune damage to the eyes.
The Unique Relationship Between Eyes and Immunity
The immune system and eyes have a special connection. Our eyes are very sensitive and important. They need to be protected from harm, but also can’t get too much protection from the immune system.
Some parts of our body, like the eyes and brain, can’t easily fix themselves. This makes them extra sensitive. To keep them safe, the body has special ways to protect them. One of these ways is called “immune privilege.”
Immune privilege means some parts of our body can handle foreign substances without getting too upset.The eyes are one of these special places. They have ways to avoid getting hurt by the immune system.
The Vulnerability of Ocular Tissues
Ocular tissues are very special and can easily get damaged. If they do, it can hurt our vision a lot. The eye’s parts, like the cornea and retina, are key for seeing and can get hurt by the immune system.
“The eye is a complex organ with many specialized tissues that are vulnerable to immune responses. Protecting these tissues is critical for maintaining vision.”
The Concept of Immune Privilege
The idea of immune privilege was first found in the eye and brain. It means these areas can avoid the immune system’s attention. They stay safe through barriers, special molecules, and certain immune cells. In the eye, things like the blood-ocular barrier and special T cells help keep it safe.
It’s important to understand how the eyes and immune system work together. This helps us find ways to treat eye problems caused by the immune system. By knowing how to balance protection and safety, we can help fix issues where this balance is off.
The Architecture of Ocular Immune Privilege

To understand ocular immune privilege, we must look at the eye’s physical and molecular barriers. These barriers protect the eye with a complex system. It involves physical structures and immunological mechanisms working together.
Physical Barriers Protecting the Eye
The eye has several physical barriers to keep pathogens out and prevent immune damage. Tears are key in this defense, washing away foreign particles and containing enzymes like lysozyme. The cornea acts as a physical shield, stopping pathogens from entering. The blood-retinal barrier also plays a role, controlling what substances reach the retina.
Tight Junctions and Their Role
Tight junctions are vital for the eye’s tissue integrity. They block the free movement of molecules and cells across layers. In the eye, they are key in the cornea and blood-retinal barrier. They protect the eye by limiting immune cell and large molecule passage.
Experts say, “The integrity of the ocular barriers is essential for maintaining the immune privileged status of the eye.” This shows how important these structures are in protecting vision and the eye’s immune privilege.
Molecular Guardians: How Eyes Evade Immune Detection
The eyes have developed special ways to avoid the immune system. They use complex protection to keep the immune system from seeing them as different or damaged. We’ll look at how the eyes do this with special molecules and proteins.
Surface Molecules That Prevent Immune Recognition
Ocular tissues have unique molecules that stop the immune system from recognizing them. These molecules are key in stopping immune cells from attacking. For example, certain molecules on ocular cells can calm down immune cells, stopping them from reacting.
Key surface molecules involved in this process include:
- CD47, which interacts with signal-regulatory protein alpha (SIRPα) on macrophages to inhibit phagocytosis.
- CD59, a complement regulatory protein that prevents the formation of the membrane attack complex.
- Other molecules like Fas ligand (FasL) that can induce apoptosis in Fas-bearing immune cells.
Anti-Inflammatory Proteins in the Eye
The eyes also make anti-inflammatory proteins to stay safe from the immune system. These proteins help keep the eye area calm and tolerant. For instance, TGF-β is a big player in keeping the immune response in check.
Anti-Inflammatory Protein | Function |
TGF-β | Suppresses T cell activation and promotes regulatory T cell differentiation. |
IL-1 receptor antagonist | Blocks the action of IL-1, a pro-inflammatory cytokine. |
Soluble TNF receptors | Neutralizes TNF-α, a cytokine involved in systemic inflammation. |
Learning about these molecular guardians helps us understand how the eyes stay safe. This balance between protection and tolerance is vital for keeping our vision and eye health.
The ACAID Phenomenon: Teaching Tolerance
The immune system has a complex way of recognizing and responding to the eyes. This involves a unique process called Anterior Chamber-Associated Immune Deviation (ACAID). It’s key for keeping the eyes safe from infection and autoimmune damage.
What is Anterior Chamber-Associated Immune Deviation?
ACAID is when antigens in the eye’s anterior chamber trigger a response that promotes tolerance. This tolerance is vital for stopping autoimmune attacks on the eye. The eye is considered “immune-privileged” because it can’t easily repair itself and is very important.
ACAID works by creating regulatory T cells that calm down immune responses against eye antigens. This protects the eye from damage caused by an overactive immune system. It makes sure the immune system doesn’t see the eyes as foreign.
The Journey of Eye Antigens to the Spleen
ACAID starts when eye antigens enter the anterior chamber. They then go to the spleen, where they help create regulatory T cells. The spleen is key in this process, as it helps the immune response lean towards tolerance.
The trip of eye antigens to the spleen is complex. It involves many cell types and signals. Antigen-presenting cells pick up the eye antigens and go to the spleen. There, they meet T cells to teach them to tolerate the antigens. This shows how the body protects the eyes from immune damage.
Learning about ACAID and its role in eye immunity helps us understand how to treat autoimmune diseases. It also shows us how to promote tolerance in other immune-privileged areas.
Regulatory T Cells: The Peacekeepers
Regulatory T cells are like peacekeepers in the immune system’s dance with the eyes. They keep the balance needed for eye health.
How Tregs Maintain Eye Immunity Balance
Regulatory T cells (Tregs) are key in stopping immune responses and keeping tolerance to eye antigens. They do this in a few ways:
- Suppressing effector T cell activation
- Producing anti-inflammatory cytokines
- Modulating the function of antigen-presenting cells
Tregs control these actions to stop autoimmune reactions. These reactions could harm vision.
The Role of TGF-beta and Other Cytokines
Transforming growth factor-beta (TGF-beta) is a major cytokine for Tregs. It helps in immune suppression and tolerance in the eye. Other cytokines, like IL-10, also help in this process.
Cytokine | Function in Eye Immunity |
TGF-beta | Promotes immune suppression and tolerance |
IL-10 | Regulates anti-inflammatory responses |
IL-35 | Contributes to Treg-mediated suppression |
The balance kept by Tregs and these cytokines is vital. It helps prevent autoimmune eye diseases and keeps vision safe.
What Happens If Your Immune System Finds Your Eyes?
When the immune system finds the eyes, it can start a complex series of events. This may lead to damage caused by the immune system. The eyes are usually protected from the immune system’s watch. But if this protection is broken, the results can be very serious.
The Breaking of Immune Privilege
The immune privilege of the eyes is broken when its protective mechanisms fail. This can happen because of injury, infection, or autoimmune diseases. As a result, the immune system may see the eyes as foreign and attack them, causing inflammation and possible tissue damage.
Initial Immune Response to Eye Antigens
When the immune system finds eye antigens, it starts a response to get rid of the threat. It activates immune cells like T cells and macrophages to enter the eye tissues. The release of cytokines and chemokines makes the immune response stronger, which can harm the eye’s delicate parts.
The breakdown of immune privilege and the immune response can cause serious eye problems. It’s important to understand these processes to find effective treatments for eye diseases caused by the immune system.
Sympathetic Ophthalmia: When One Eye’s Trauma Endangers Both
Trauma to one eye can have far-reaching consequences. It can lead to sympathetic ophthalmia, a rare condition that affects both eyes. This condition shows how closely connected our eyes are and how our immune system reacts to injury.
The Mechanism of Sympathetic Ophthalmia
The exact mechanism of sympathetic ophthalmia is complex. It involves an immune response. When one eye is injured, it can trigger an autoimmune reaction. This reaction targets the uveal tissue of both eyes.
Key factors contributing to sympathetic ophthalmia include:
- Trauma or surgery to one eye
- Release of ocular antigens into the circulation
- Activation of T cells against these antigens
- Immune response targeting the uveal tissue of both eyes
Historical Perspectives and Famous Cases
Sympathetic ophthalmia has been known for centuries. The first recorded case was in the 17th century. Many cases have been documented in medical literature.
“Sympathetic ophthalmia is a rare but serious condition that highlights the importance of treating eye injuries promptly.” –
A leading ophthalmologist
In the past, sympathetic ophthalmia often led to vision loss in both eyes. But, thanks to medical advancements, treatment outcomes have greatly improved.
Understanding sympathetic ophthalmia is key for patients and doctors. It shows the need for quick medical care after eye trauma. It also shows how our eyes and immune system are connected.
Autoimmune Eye Diseases: When Self-Recognition Goes Wrong
Autoimmune eye diseases are a big problem in eye care. They happen when the immune system doesn’t see the eyes as its own. This leads to the immune system attacking the eyes.
Uveitis and Its Variants
Uveitis is a common autoimmune eye disease. It causes inflammation in the middle layer of the eye. It can affect different parts of the uvea, leading to different types of uveitis.
Symptoms of uveitis include eye pain, redness, and sensitivity to light. It can also cause vision problems. If not treated, it can lead to serious eye damage.
“Uveitis is a significant cause of visual impairment worldwide, stressing the need for quick diagnosis and treatment.”
Medical Expert, Ophthalmologist
Ocular Cicatricial Pemphigoid
Ocular cicatricial pemphigoid (OCP) is a chronic autoimmune disease. It affects the eye’s mucous membranes, causing scarring and vision loss. It leads to the formation of blisters and scarring on the conjunctiva.
- Symptoms include chronic conjunctivitis, eye irritation, and progressive scarring.
- Treatment involves immunosuppressive therapy to reduce inflammation and prevent further scarring.
Vogt-Koyanagi-Harada Disease
Vogt-Koyanagi-Harada (VKH) disease is a rare autoimmune condition. It affects melanin-rich tissues, including the eyes, skin, and inner ear. Symptoms include uveitis, retinal detachment, and vitreitis.
Disease | Primary Symptoms | Treatment Approaches |
Uveitis | Eye pain, redness, sensitivity to light | Corticosteroids, immunosuppressive drugs |
Ocular Cicatricial Pemphigoid | Chronic conjunctivitis, scarring | Immunosuppressive therapy |
Vogt-Koyanagi-Harada Disease | Uveitis, skin depigmentation, inner ear symptoms | Corticosteroids, immunosuppressive therapy |
In conclusion, autoimmune eye diseases like uveitis, ocular cicatricial pemphigoid, and Vogt-Koyanagi-Harada disease need quick diagnosis and treatment. Understanding these conditions is key to managing them effectively.
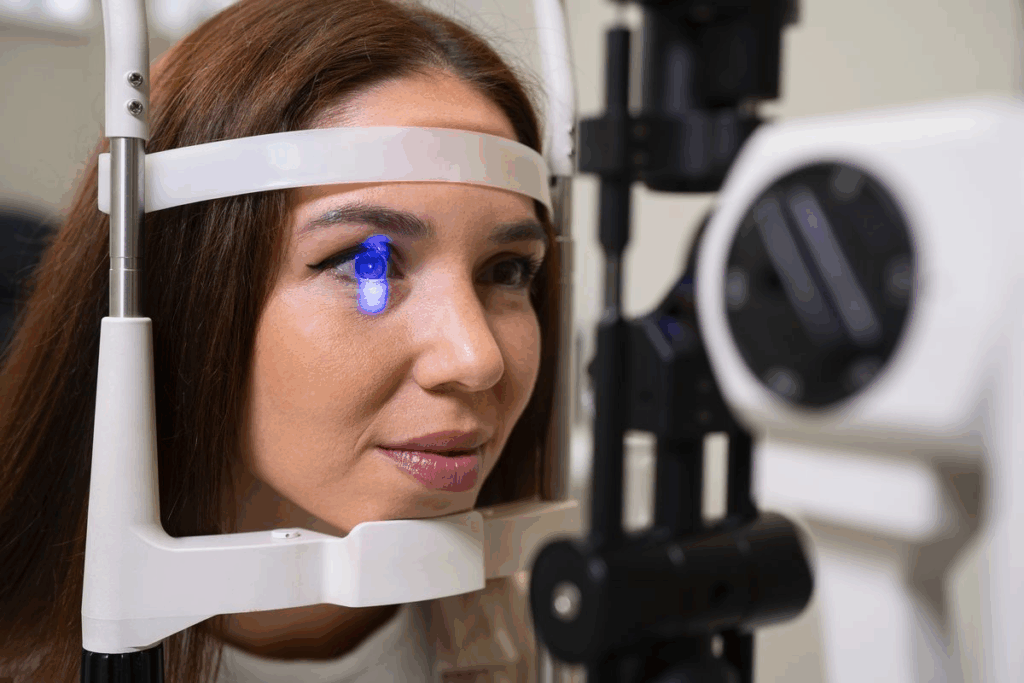
Diagnosing Immune-Mediated Eye Disorders
Immune-mediated eye disorders are hard to diagnose. They need a close look at symptoms and new testing methods. We’ll see how doctors figure out these tricky cases.
Clinical Signs of Immune Attack
The first step is spotting signs of an immune attack. Look for redness, pain, sensitivity to light, and vision problems. Severe cases can lead to inflammation, tissue damage, and vision loss.
Doctors must quickly spot these signs. A full eye check is key. It looks at the eye’s parts and how they work.
Modern Diagnostic Techniques
New ways to test help find immune eye disorders. Here are some:
- Imaging Studies: Tools like Optical Coherence Tomography (OCT) and fluorescein angiography show the eye’s details. They spot inflammation or damage.
- Laboratory Tests: Blood tests and other lab work find immune system problems or eye-related autoimmunity.
- Clinical Examination: A detailed eye exam, including vision tests and slit-lamp checks, gives important info.
Using these tests together helps doctors understand the patient’s eye health. This leads to the right treatment plan.
Diagnostic Technique | Description | Clinical Utility |
Optical Coherence Tomography (OCT) | Non-invasive imaging technique providing high-resolution images of retinal layers. | Assesses retinal thickness, detects edema, and identifies structural abnormalities. |
Fluorescein Angiography | Dye-based imaging technique highlighting vascular structures and leakage. | Evaluates vascular integrity, detects leakage, and identifies areas of ischemia. |
Blood Tests | Laboratory analysis of blood samples to identify inflammatory markers or autoimmune antibodies. | Helps diagnose underlying autoimmune conditions or systemic inflammation affecting the eye. |
By combining symptoms with new tests, we can accurately find and treat immune eye disorders. This helps save vision and improve patient care.
Treating and Managing Ocular Immune Disorders
Treating ocular immune disorders requires a variety of therapies. These aim to lessen inflammation and control the immune system. A good plan considers the condition, its severity, and the patient’s health.
Immunosuppressive Therapies
Immunosuppressive therapies are key in treating these disorders. They help reduce the immune system’s overactive response. This lessens inflammation and damage to tissues.
Common treatments include corticosteroids for quick inflammation control. For long-term use, drugs like methotrexate, cyclosporine, and azathioprine are used.
Corticosteroids are often the first choice because of their strong anti-inflammatory effects. But, long-term use can cause side effects like cataracts and increased eye pressure.
Biological Treatments
Biological treatments are a newer option that has changed how we manage these disorders. They target specific parts of the immune response. This approach can have fewer side effects.
Tumor necrosis factor-alpha (TNF-alpha) inhibitors, like infliximab and adalimumab, are used for conditions like uveitis. Choosing the right patient and monitoring them closely is important due to risks like infections and tuberculosis reactivation.
Surgical Interventions
Surgery is vital for managing ocular immune disorders, mainly for structural damage or complications. Surgical procedures can improve vision, reduce pain, and enhance quality of life.
Surgery might be combined with other treatments for better results. For example, cataract surgery in uveitis patients needs careful management with anti-inflammatory drugs to avoid complications.
By using these treatments together, we can manage ocular immune disorders well. This reduces complications and improves patient outcomes.
Conclusion: The Delicate Balance of Ocular Immunity
The balance of ocular immunity is key to keeping our eyes healthy and our vision clear. The eye’s immune system works hard to protect it without causing harm. We’ve looked into how the immune system affects our eyes and what happens when it doesn’t work right.
When the immune system finds the eyes, it can cause damage if not controlled. Knowing how ocular immunity works is vital for treating eye problems caused by the immune system.
Keeping this balance helps protect our eyes and our sight. The complex link between the immune system and our eyes shows why we need more research. This research is important for keeping our eyes healthy.
FAQ
Does the immune system recognize the eyes as part of the body?
Yes, the immune system knows the eyes are part of us. It keeps them safe to avoid harm.
What is ocular immune privilege?
Ocular immune privilege is a special protection for the eyes. It keeps them safe from harm and helps us see well.
How do the eyes evade immune detection?
The eyes use many ways to stay hidden from the immune system. They have physical barriers and special molecules. They also have proteins that fight inflammation.
What is Anterior Chamber-Associated Immune Deviation (ACAID)?
ACAID is when the immune system learns to ignore the eyes. This keeps the eyes safe and vision clear.
What happens when the immune system discovers the eyes?
If the immune system finds the eyes, it can lose its protection. This can cause damage and harm our vision.
Can the immune system attack the eyes?
Yes, sometimes the immune system can turn against the eyes. This can lead to diseases like uveitis and ocular cicatricial pemphigoid.
What is sympathetic ophthalmia?
Sympathetic ophthalmia is a rare condition. It happens when one eye is hurt, and it can affect both eyes. It’s a serious threat to vision.
How are immune-mediated eye disorders diagnosed?
Doctors use many ways to find these disorders. They look at symptoms, do tests, and use imaging to see what’s happening.
What are the treatment options for ocular immune disorders?
Doctors use different treatments to help the eyes. They might use medicines, biological treatments, or surgery. The goal is to stop the damage and help the eyes heal.
Why is maintaining the balance of ocular immunity important?
Keeping the balance of eye immunity is key. It helps protect the eyes from harm and keeps our vision safe.
How do regulatory T cells contribute to eye immunity?
Regulatory T cells are important for eye health. They help control the immune system and prevent diseases.
What is the role of tight junctions in ocular immune privilege?
Tight junctions are important for eye protection. They help keep the eyes safe by forming strong barriers against damage.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698145/

































