Last Updated on November 25, 2025 by Ugurkan Demir

When the heart’s rhythm is disrupted, electrical cardioversion can be a safe and effective treatment. At Liv Hospital, we use this procedure to restore a normal heart rhythm in patients with atrial fibrillation.
Electrical cardioversion, also known as electrocardioversion, involves delivering a controlled electric shock to the chest to reset the heart rhythm. This frontline treatment is trusted by patients and guided by our commitment to excellence.
Key Takeaways
- Electrical cardioversion is a safe and effective treatment for atrial fibrillation.
- The procedure involves delivering a controlled electric shock to the chest.
- It is a frontline treatment for restoring a normal heart rhythm.
- Liv Hospital is committed to delivering world-class healthcare.
- Our team of experts guides patients through the treatment process.
Understanding Atrial Fibrillation and Normal Heart Rhythm

Atrial fibrillation, or AFib, is when the heart beats irregularly and fast. This happens when the upper heart chambers (atria) don’t beat right. They don’t move blood well to the lower chambers (ventricles).
What Happens During Atrial Fibrillation
In atrial fibrillation, the heart’s electrical signals get mixed up. This makes the atria quiver instead of beating right. This can cause symptoms like:
- Palpitations or irregular heartbeats
- Shortness of breath
- Fatigue or weakness
- Dizziness or lightheadedness
Atrial fibrillation can start from many things, like high blood pressure or heart disease. Knowing what causes it helps manage it better.
How Normal Heart Rhythm Works
A normal heart rhythm comes from the heart’s natural pacemaker, the SA node. It sends signals to the atria, making them contract and pump blood. Then, the signals go to the ventricles, pumping blood out to the body.
Normal heart rhythm is key for the heart to work well. It makes sure the body gets enough oxygen and nutrients.
Impact of Arrhythmias on Overall Health
Arrhythmias, like atrial fibrillation, can harm health a lot. If not treated, they can cause stroke, heart failure, and other heart issues.
It’s important to know the risks of arrhythmias. Working with doctors can help manage the condition. This way, people with atrial fibrillation can lower their risk of problems and live better.
What is Electrical Cardioversion: The Heart Jump Start Procedure
Doctors might suggest electrical cardioversion for severe arrhythmia. This method uses electric shocks to fix the heart’s rhythm. It works well for atrial fibrillation, where the heart’s upper chambers beat irregularly.
Definition and Basic Principles
Electrical cardioversion, or electrocardioversion, is a treatment that uses electric shocks to the chest. It aims to get the heart’s rhythm back to normal. This method is based on the idea that a timed electric shock can reset the heart’s electrical activity.
The process involves sedation or anesthesia to minimize discomfort. Then, synchronized electrical shocks are applied. This synchronization is key to avoid complications.
How Cardioversion Differs from Defibrillation
Cardioversion and defibrillation both use electric shocks, but they differ. Defibrillation is used in emergencies when the heart stops or is in a dangerous rhythm. It shocks the heart without timing it.
Cardioversion, on the other hand, is planned for arrhythmias like atrial fibrillation. It uses timed shocks to fix the heart rhythm. This makes it safer and more controlled.
“Cardioversion is a highly effective treatment for restoring normal sinus rhythm in patients with atrial fibrillation, improving symptoms and quality of life.”
Historical Development of Electrocardioversion
The idea of using electrical shocks for arrhythmias started in the early 20th century. But it wasn’t until the 1960s that it became common. Advances in technology and understanding of heart rhythm disorders have made it a standard treatment.
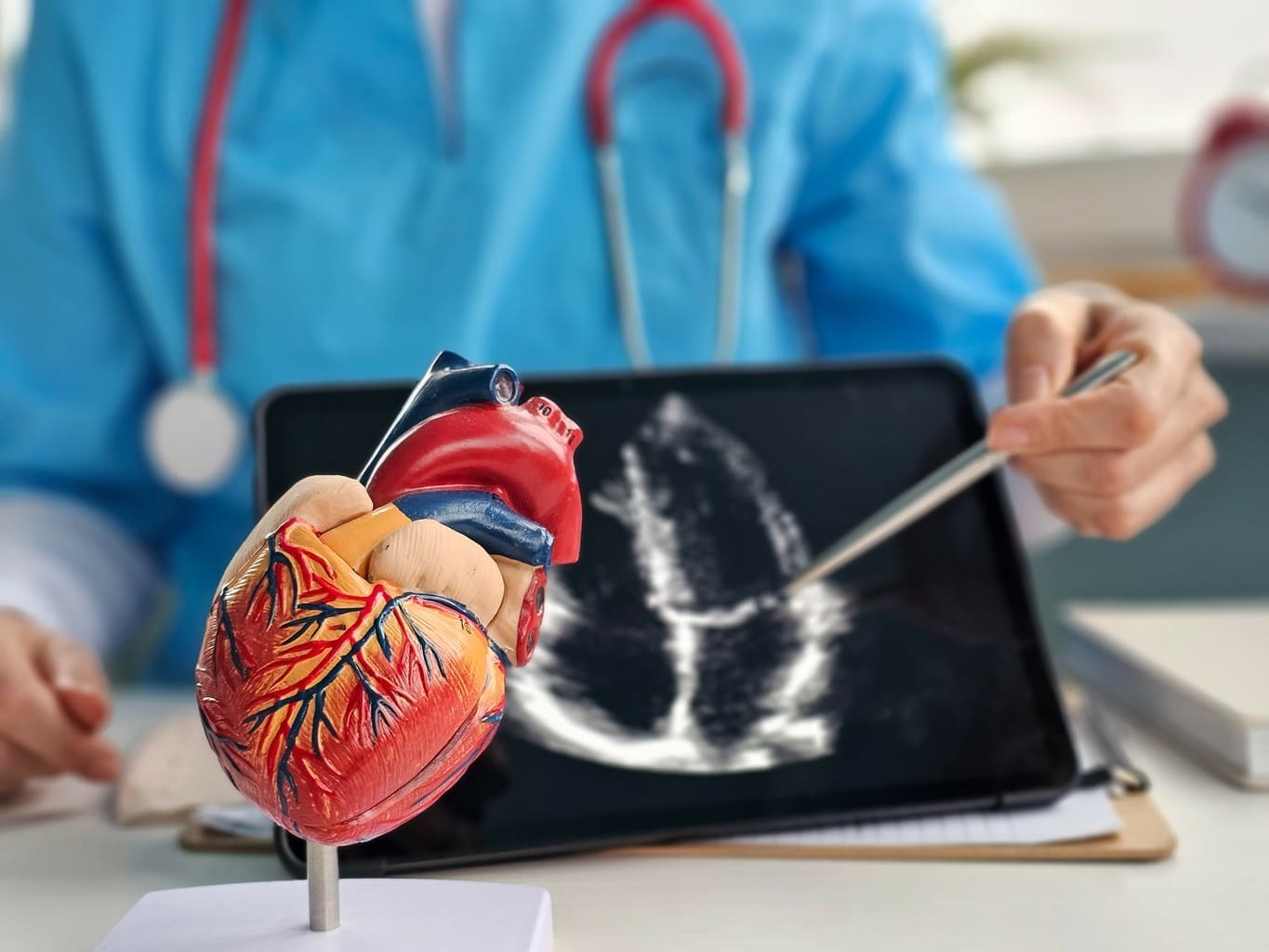
Equipment Used in Modern Cardioversion
Today’s cardioversion equipment has advanced a lot. It uses new technologies to make the treatment safer and more effective. Modern devices can give precise, timed shocks and monitor the heart’s response.
The tools include defibrillator/pacemaker machines, electrodes, and monitoring devices. These help doctors tailor the treatment to each patient. This increases the chance of success.
When Shocking the Heart for Atrial Fibrillation is Necessary
For many patients, electrical cardioversion is needed when atrial fibrillation symptoms don’t go away. Atrial fibrillation (Afib) is a complex condition that needs careful management. At first, treatments might include medication or lifestyle changes. But some patients need more immediate help.
Medical Indications for Electrical Cardioversion
Electrical cardioversion is considered when Afib symptoms are severe and affect a patient’s quality of life. It’s also for those at risk of heart failure or stroke from Afib.
We look at several factors before deciding on cardioversion. These include how long Afib has lasted, the patient’s health, and any heart conditions.
Emergency Cardioversion for Unstable Patients
In emergency cases, cardioversion is done quickly to fix a patient’s heart rhythm if they’re unstable. Symptoms of instability include severe chest pain, shortness of breath, or a big drop in blood pressure.
Emergency cardioversion is a lifesaving procedure. It helps stabilize the patient and improves their recovery chances.
Scheduled Cardioversion for Persistent Afib
For those with persistent atrial fibrillation, scheduled cardioversion is an option. This procedure is done under sedation or light anesthesia to reduce discomfort.
Scheduled cardioversion allows for careful planning. This includes anticoagulation therapy to lower stroke risk.
When Other Treatments Are Tried First
Before cardioversion, other treatments are tried first. These include medications to control heart rate or rhythm, and lifestyle changes like diet and exercise.
We also consider alternative treatments like catheter ablation or surgery for some patients.
Let’s look at a comparison of treatment approaches for atrial fibrillation:
| Treatment Approach | Description | Typical Use Case |
| Medication | Rate or rhythm control medications | Initial treatment for most Afib patients |
| Cardioversion | Electrical shock to restore normal rhythm | For persistent Afib or when medications fail |
| Catheter Ablation | Minimally invasive procedure to destroy abnormal electrical pathways | For patients who don’t respond to medications or cardioversion |
Preparing for Electrical Cardioversion
Electrical cardioversion needs careful preparation. This includes tests, anticoagulation therapy, and fasting guidelines. Understanding these steps is key to a safe and effective procedure.
Pre-Procedure Testing and Evaluation
Before the procedure, patients go through tests to check their heart health. These tests help find any risks. They may include:
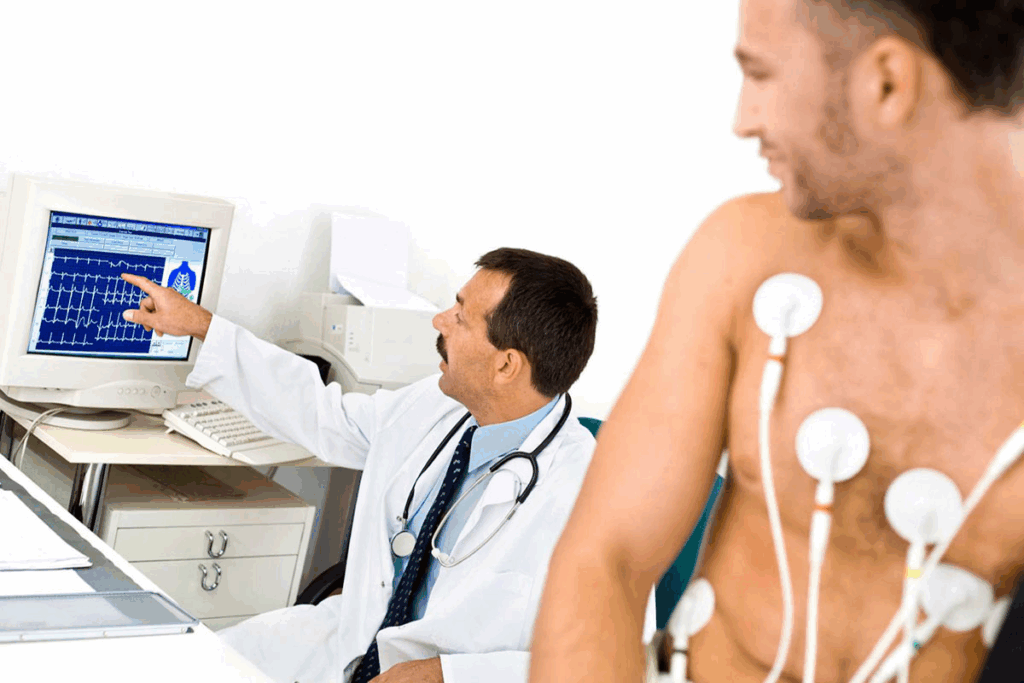
- Electrocardiogram (ECG): To check the heart’s rhythm and find any issues.
- Echocardiogram: To look at the heart’s structure and how it works.
- Blood tests: To see if there are blood clots or other problems that could affect the procedure.
Anticoagulation Requirements and Blood Thinners
Anticoagulation therapy is very important for preparing for electrical cardioversion. Anticoagulants, or blood thinners, prevent blood clots. This is to avoid the risk of stroke during the procedure. Patients usually take these for weeks before the procedure.
| Anticoagulant | Common Brand Names | Monitoring Requirements |
| Warfarin | Coumadin | Regular INR monitoring |
| Dabigatran | Pradaxa | Less frequent monitoring |
| Rivaroxaban | Xarelto | No routine monitoring |
Fasting and Medication Guidelines
Patients usually need to fast for 6 to 8 hours before the procedure. We also give specific advice on managing medications. This includes:
- Keeping up with essential medications as directed.
- Adjusting or stopping certain medications that could affect the procedure or anesthesia.
Insurance Coverage and Cost Considerations in the US
It’s important to know about insurance coverage and costs. We suggest checking with your insurance provider. Also, talk to our billing department about any financial worries.
Insurance coverage and costs can change a lot depending on the provider and your plan.
The Electric Shock to Heart Procedure Step by Step
For those with atrial fibrillation, electrical cardioversion is a game-changer. It uses a controlled electric shock to fix the heart’s rhythm. Let’s explore the steps involved in this treatment.
Setting Up the Cardioversion Equipment
The first step is setting up the needed equipment. This includes a cardioversion device and monitoring tools. Our team makes sure everything is ready and working right.
Sedation Process and Anesthesia
Before starting, patients get sedation to relax and feel less pain. The sedation level depends on the patient’s health and the team’s choice. We focus on making sure patients are comfortable and safe. Sometimes, general anesthesia is used for anxious patients or complex procedures.
Paddle Placement and Synchronized Energy Delivery
The next step is placing paddles on the patient’s chest. These paddles connect to the device, which sends a synchronized shock. This method lowers the risk of problems. The shock’s strength is chosen carefully for each patient.
Monitoring During the Reset Heart Rhythm Procedure
During the procedure, the patient’s heart and vital signs are watched closely. This lets the team act fast if needed.
“The key to a successful cardioversion is not just the delivery of the electric shock, but the complete care before, during, and after.”
Monitoring continues until the patient is stable and recovering well.
Recovery After Electric Shock for Afib
The journey to a normal heart rhythm doesn’t stop after the procedure. It continues into the recovery phase. We’ll guide you through this critical period, covering post-procedure care, monitoring, and when to resume activities.
Immediate Post-Procedure Care
After the procedure, we watch your heart rhythm and overall health closely. You’ll be in a recovery area where our team will monitor your vital signs. They ensure you’re recovering well from the procedure and sedation.
You might feel groggy from the sedation. Our staff will help you until you’re fully awake and stable. It’s normal to feel disoriented or have a sore throat if a breathing tube was used.
Monitoring Heart Rhythm After Cardioversion
Monitoring your heart rhythm is key in the hours after cardioversion. We use electrocardiogram (ECG) machines to track your heart’s activity. This ensures your rhythm stays stable.
Our team will also check for any complications and address your concerns. The data from this monitoring helps us see how well your heart is responding to treatment.
Managing Skin Irritation
Some patients may get skin irritation or redness where the paddles were placed. This is usually mild and temporary, going away in a few hours.
We suggest keeping the area clean and dry. If you have persistent discomfort, we can offer advice on how to manage it.
When You Can Return Home and Resume Activities
How long you stay in the hospital or clinic depends on your health and recovery. Most people can go home the same day, once they’re fully awake and their vital signs are stable.
| Activity | Guidelines for Resuming Activities |
| Driving | Wait at least 24 hours after the procedure, or as advised by your doctor. |
| Returning to Work | Typically within a few days, depending on your job requirements and recovery. |
| Exercise and Physical Activities | Resume gradually, as recommended by your healthcare provider. |
Following our post-procedure instructions is key for a smooth recovery. We’ll give you detailed guidance on resuming activities. This includes any follow-up appointments to check on your heart’s rhythm.
Risks and Complications of Electrical Shock to Heart
It’s important to know the risks of cardioversion for those with atrial fibrillation. This treatment is usually safe, but knowing the possible complications and side effects is key.
Common Side Effects and Discomfort
Most people do well with cardioversion, but some might face minor issues. These can include:
- Discomfort or pain from the electrical shock
- Skin irritation or redness at the electrode sites
- Mild soreness or bruising
- Fatigue or drowsiness due to sedation
These side effects are usually short-lived and go away by themselves.
Serious Complications to Be Aware Of
Even though rare, serious problems can happen. These might include:
- Thromboembolic events, such as stroke
- Arrhythmias or irregular heartbeats
- Cardiac arrest (very rare)
- Reaction to sedation or anesthesia
Talking to your doctor about your risks is very important.
Risk Factors for Adverse Outcomes
Some factors can make complications more likely during or after cardioversion. These include:
- Pre-existing heart conditions
- History of stroke or thromboembolic events
- Poorly controlled heart failure
- Electrolyte imbalances
Knowing these risk factors helps doctors prepare better.
How Doctors Minimize Cardioversion Risks
Doctors take many steps to lower risks:
- Careful patient selection and evaluation
- Appropriate anticoagulation therapy
- Monitoring during and after the procedure
- Use of sedation or anesthesia to reduce discomfort
By understanding and addressing these risks, doctors can help patients have the best results from cardioversion.
Alternative Methods to Get Heart Back into Rhythm
Treating atrial fibrillation isn’t just about electrical cardioversion. Other methods can also help get the heart back to normal. For many, a mix of treatments works best to manage symptoms and improve life quality.
Medication Options for Rhythm Control
Medicines are key in managing atrial fibrillation. Anti-arrhythmic drugs help keep the heart rhythm normal. Rate-control medications slow the heart rate, making it more efficient. The right choice depends on symptoms, health, and the cause of atrial fibrillation.
Some common medicines include:
- Beta-blockers to slow the heart rate
- Calcium channel blockers to reduce heart rate and blood pressure
- Flecainide or propafenone to maintain normal sinus rhythm
- Amiodarone for severe or persistent atrial fibrillation
Catheter Ablation Procedures
Catheter ablation is a minimally invasive treatment. It destroys the abnormal electrical pathways in the heart. A cardiologist uses catheters to deliver energy, creating scar tissue that stops the faulty signals.
This treatment is good for patients who:
- Have not responded well to medication
- Experience severe symptoms
- Prefer a more definitive treatment
Lifestyle Modifications to Support Heart Health
Changing your lifestyle can greatly help manage atrial fibrillation. Maintaining a healthy weight, exercising regularly, and eating a balanced diet are all good for the heart. Also, cutting down on caffeine, alcohol, and tobacco can reduce symptoms.
Stress management, like meditation or yoga, can also help reduce episodes of atrial fibrillation.
When to Consider Surgical Interventions
In some cases, surgery is needed to treat conditions that cause atrial fibrillation. Procedures like the Maze procedure or surgical ablation can be done during heart surgeries. These are usually for patients with severe symptoms or those having other heart surgeries.
Conclusion: Living with Atrial Fibrillation After Cardioversion
After electrical cardioversion for atrial fibrillation, patients must manage their condition well. This helps prevent recurrence and keeps quality of life high. Living with atrial fibrillation means ongoing medical care and lifestyle changes for heart health.
Managing afib after cardioversion involves watching heart rhythm and following medication. It also means making lifestyle changes. We help patients create a care plan tailored to them. This ensures they get the support they need to manage their condition well.
Understanding the role of anticoagulation therapy, eating healthy, and staying active can lower recurrence risk. We aim to provide complete care and guidance. This helps patients deal with the challenges of living with atrial fibrillation after cardioversion.
FAQ
What is electrical cardioversion?
Electrical cardioversion is a medical procedure. It uses electrical shocks to fix irregular heartbeats, like atrial fibrillation.
How does electrical cardioversion work?
It works by giving the heart a controlled shock. This shock is timed with the heart’s rhythm to be safe and effective.
What is the difference between cardioversion and defibrillation?
Both use electrical shocks for heart rhythm issues. But, cardioversion treats organized arrhythmias, while defibrillation is for emergencies.
Is electrical cardioversion painful?
It’s usually done under sedation to avoid pain. Patients might feel a brief shock, but the sedation helps.
How long does it take to recover from electrical cardioversion?
Recovery is fast, with most going home the same day. Some might have minor side effects like skin redness, but these go away quickly.
Can electrical cardioversion cure atrial fibrillation?
It can fix the heart rhythm in many patients. But, it might not last forever. More treatments or lifestyle changes might be needed.
What are the risks associated with electrical cardioversion?
It’s generally safe but can have risks like skin burns or blood clots. Certain health conditions might increase these risks.
How is electrical cardioversion performed?
The process involves setting up equipment, giving sedation, and using paddles on the chest. Then, a synchronized shock is delivered to fix the rhythm.
Are there alternative treatments to electrical cardioversion for atrial fibrillation?
Yes, there are other options. These include medications, catheter ablation, lifestyle changes, and sometimes surgery.
What should I expect after undergoing electrical cardioversion?
After the procedure, you’ll be monitored and your heart rhythm checked. Most can go back to normal activities soon, but follow post-procedure instructions.
Can atrial fibrillation recur after electrical cardioversion?
Yes, it can happen again. To prevent it, ongoing management like medication and lifestyle changes might be needed.
How do I prepare for electrical cardioversion?
Preparation includes pre-procedure tests, anticoagulation therapy, fasting, and adjusting medications as your doctor advises.
References:
- Ruel, M. (2024). Coronary artery bypass grafting: Past and future. Circulation, 150(10), 763-766. https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.124.068312