A shoulder dislocation can be very traumatic. Many wonder if their shoulder will ever be the same. Surprisingly, nearly 2% of people will experience a shoulder dislocation in their lifetime.Discover if shoulder strength after dislocation improves and how rehab helps rebuild muscles.
Research shows that recovery from a shoulder dislocation is complex. It involves healing the injured joint and restoring its strength and function.
So, do shoulders get stronger after dislocation? The answer depends on the rehabilitation process and factors that affect shoulder strength after an injury.
Key Takeaways
- Understanding the impact of a shoulder dislocation on overall shoulder health.
- The importance of proper rehabilitation in restoring shoulder strength.
- Factors influencing the recovery process and outcomes.
- Strategies for improving shoulder strength after dislocation.
- The role of physical therapy in shoulder injury rehabilitation.
Understanding Shoulder Dislocations
The shoulder joint is very mobile, which makes it prone to dislocations. This mobility is great for movement but also makes the joint unstable. Knowing about shoulder dislocations helps in treating and rehabilitating them effectively.
Types of Shoulder Dislocations
Shoulder dislocations can be divided into different types based on the direction and severity. The most common types are:
- Anterior Dislocation: This is the most common type, where the humerus is displaced forward, out of the shoulder socket.
- Posterior Dislocation: Less common, this occurs when the humerus is displaced backward.
- Inferior Dislocation: A rare and severe form where the humerus is displaced downward.
Each type has its own causes and treatment options.
Common Causes and Mechanisms of Injury
Shoulder dislocations often happen due to significant trauma, like falls, sports injuries, or car accidents. The ways these injuries occur include:
- Direct Blow: A direct hit to the shoulder can cause dislocation.
- Falls onto an Outstretched Hand: The force transmitted through the arm can dislocate the shoulder.
- Sports Injuries: High-impact sports increase the risk of shoulder dislocation.
Understanding these causes is key for prevention and creating effective rehabilitation plans.
By knowing the types and causes of shoulder dislocations, people can better handle the recovery process. This is important for regaining strength and preventing future dislocations.
The Immediate Impact on Shoulder Function
A dislocated shoulder right away makes it hard for the shoulder to work right. The shoulder joint is very mobile but also gets hurt easily. When it gets dislocated, it can cause many problems with how the shoulder works.
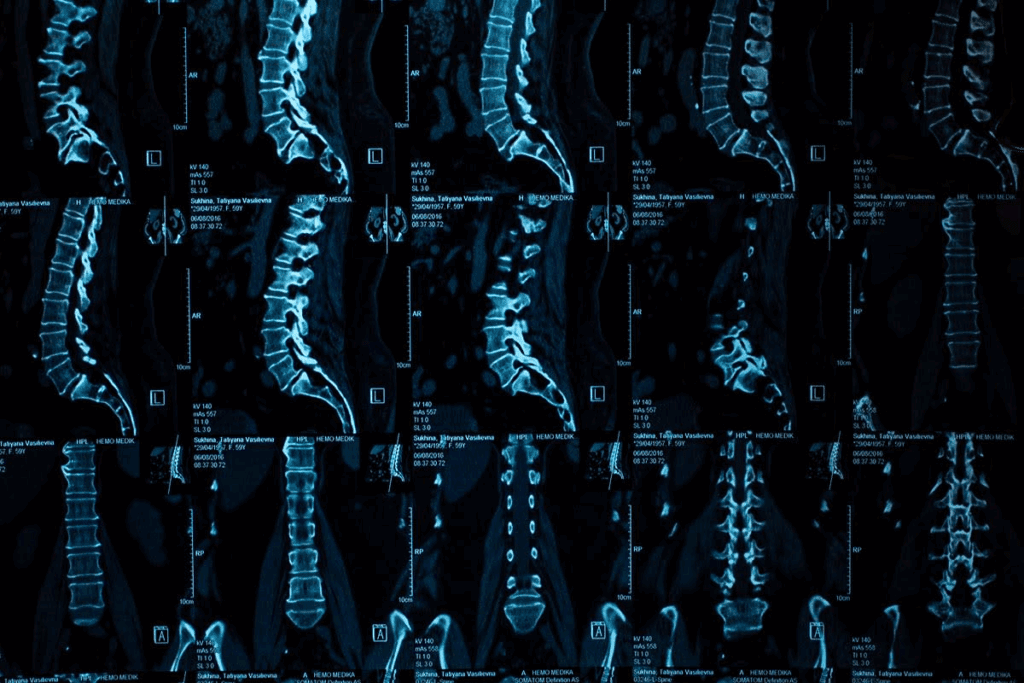
Muscle and Tissue Damage Assessment
How much muscle and tissue get hurt from a shoulder dislocation can differ a lot. It’s important to check the damage to figure out the best treatment. Doctors do a detailed check-up and might use X-rays or an MRI to see how bad the damage is.
Muscle damage can be small or all the way torn. Tissue damage might hurt the labrum or other parts that keep the shoulder stable. Getting the right diagnosis is essential to fix these problems and get the shoulder working again.
Initial Strength Deficits Post-Dislocation
After a shoulder dislocation, people often can’t lift as much as they used to. This weakness is because of the pain, swelling, and instability from the injury. It makes simple tasks hard to do.
The amount of weakness depends on how bad the dislocation was and any other injuries. Rehab programs help by starting with easy exercises and then getting harder. This helps build back strength.
The Biology of Shoulder Joint Recovery
Understanding the biology of shoulder joint recovery is key for effective rehab after a dislocation. It involves many biological processes working together to fix and grow back damaged tissues.
The healing starts right after the injury, with the body’s first step being inflammation. This phase is vital as it prepares the ground for repair. The inflammatory response brings cells and nutrients to the injured area, helping to clear out debris and damaged tissue.
Healing Processes in Shoulder Tissues
Shoulder tissue healing after a dislocation goes through several stages. These include inflammation, repair, and remodeling. In the repair phase, the body builds back damaged tissues with collagen and proteins. This is essential for the shoulder joint to regain its strength and integrity.
The remodeling phase, lasting several months to a year or more, refines the new tissue. It’s critical to have effective rehab strategies during this phase for the best recovery.
Factors Affecting Recovery
Many factors can affect how well someone recovers from a shoulder dislocation. These include the injury’s severity, the quality of the rehab program, and the person’s health and age. Knowing these factors helps create a rehab plan that’s just right for each person.
- The severity of the dislocation and any injuries it caused.
- Any health conditions the person might have.
- The quality of medical care and rehab received.
- How well the person sticks to the rehab program.
By considering these factors and customizing the rehab plan, people can improve their recovery chances. They can get their shoulder back to its best function.
Medical Interventions After Shoulder Dislocation
Dealing with a dislocated shoulder often means using a mix of treatments. These can range from simple methods to more complex surgeries. The right treatment depends on how bad the dislocation is, if there are other injuries, and the patient’s health and lifestyle.
Conservative Treatment Approaches
For many, the first step is conservative treatment. This is often used for first-time dislocations with minor injuries. It involves wearing a sling and then doing exercises to build strength and move better. Starting to move and exercise early is key to avoid stiffness and get back to normal.
Conservative treatments include:
- Using medicine to manage pain
- Physical therapy to improve movement and strength
- Changing activities to avoid making the injury worse
Surgical Interventions and Their Impact on Future Strength
For those with repeated dislocations, significant bone loss, or other injuries, surgery might be needed. Surgery can make the shoulder joint more stable and lower the chance of future dislocations. But, surgery also has risks and can affect future shoulder strength.
The effect of surgery on future strength varies. Some surgeries, like arthroscopic stabilization, aim to cause less damage and help you recover faster.
| Treatment Approach | Key Components | Impact on Future Strength |
| Conservative Treatment | Immobilization, rehabilitation, pain management | Generally preserves strength, but may not fully restore it in cases of severe injury |
| Surgical Intervention | Stabilization procedures, repair of associated injuries | Can improve stability and strength, but carries surgical risks and variable outcomes |
It’s important to understand the effects of these treatments when deciding on shoulder dislocation care. Both conservative and surgical methods have their roles. The best choice depends on the patient’s specific situation and needs.
Shoulder Strength After Dislocation: The Complete Recovery Process

Recovering shoulder strength after a dislocation is complex. It involves understanding the injury and the body’s healing. A full recovery needs a medical check, proper treatment, and a good rehab plan.
Realistic Strength Recovery Expectations
It’s key to have realistic hopes for shoulder strength recovery. The time it takes can vary a lot. It depends on the injury’s severity, treatment success, age, and health.
Most people can get back a lot of their strength in 3 to 6 months. But, full recovery might take longer.
Factors influencing recovery time include:
- The severity of the initial injury
- The presence of any associated injuries, such as fractures or rotator cuff tears
- The effectiveness of the treatment plan, whether conservative or surgical
- Adherence to the rehabilitation program
Potential Limitations in Strength Recovery
While many regain strength, some might face limits. Factors that could limit recovery include:
- Persistent instability or recurrent dislocations
- Chronic pain or discomfort
- Residual stiffness or limited range of motion
- Muscle atrophy or weakness due to prolonged immobilization or inadequate rehabilitation
Knowing these limits is key for a good rehab plan. It helps in overcoming challenges and achieving full recovery.
Factors That Enhance Strength Rebuilding
Several things can help rebuild shoulder strength. These include:
- Early mobilization and rehabilitation: Starting with gentle exercises early can prevent stiffness and aid healing.
- Progressive resistance training: Increasing exercise intensity can strengthen shoulder muscles.
- Proper nutrition and hydration: Good nutrition and hydration are vital for muscle repair and health.
- Professional guidance: Working with a healthcare professional or physical therapist can offer personalized advice and adjustments to the rehab plan.
By understanding the recovery process, knowing the limits, and using factors that help rebuild strength, people can improve their chances of full recovery.
The Rehabilitation Timeline for Dislocated Shoulders
The journey to heal a dislocated shoulder is complex, with several key stages. Knowing the timeline helps people set realistic goals and stick to their recovery plans.
Acute Phase Recovery
The first stage, the acute phase, lasts a few days to weeks after the injury. It focuses on easing pain and swelling. Gentle movements are started to avoid stiffness.
Pain management is key. This might include rest, ice, compression, and elevation (RICE), plus medication as advised by a doctor.
Intermediate Strengthening Phase
After the acute phase, the strengthening phase begins, usually 2-6 weeks later. This stage uses progressive resistance exercises to build muscle strength. The goal is to make the shoulder joint more stable and improve function.
Advanced Rehabilitation Milestones
The advanced phase starts around 6-12 weeks after the injury. It introduces more complex movements. This phase aims for full strength, better flexibility, and improved muscle control.
Functional training is a big part of this stage. It prepares people to go back to their usual activities or sports.
It’s vital to work with healthcare experts to make a recovery plan that fits. By following the timeline, people can get the best results from their shoulder rehabilitation.
Essential Rehabilitation Exercises for Shoulder Recovery
A good rehab program with specific exercises is vital for recovering from a shoulder dislocation. These exercises help regain strength, improve movement, and make the shoulder more stable.
Early Stage Mobility and Stability Exercises
In the early recovery stages, focus on exercises that help move the shoulder gently and prevent stiffness. These include:
- Pendulum exercises to loosen the shoulder joint
- Wall slides to improve flexion and abduction
- Scapular squeezes to enhance scapular stability
An orthopedic specialist, says,
“Early mobilization is critical in preventing chronic stiffness and improving outcomes in patients with shoulder dislocations.”
Progressive Resistance Training Techniques
After the shoulder starts moving better and is stable, it’s time for progressive resistance training (PRT). PRT helps strengthen the shoulder muscles with:
- Resistance band exercises for controlled strengthening
- Light dumbbell exercises for progressive overload
- Bodyweight exercises to enhance functional strength
It’s important to increase the difficulty of these exercises slowly to avoid injury and make sure the shoulder can handle more weight.
Functional Movement Patterns for Strength Development
The final rehab stage involves exercises that mimic daily activities or sports. This includes:
- Plyometric exercises to improve power
- Agility drills to enhance coordination and reaction time
- Task-specific training to ensure functional strength
Functional training not only rebuilds strength but also prepares the shoulder for everyday activities or sports.
Building Superior Shoulder Stability Post-Dislocation
Getting your shoulder stable after a dislocation takes a detailed plan. It focuses on the rotator cuff and scapular stabilizers. This approach helps regain strength and prevents future problems. It makes sure the shoulder joint is strong and stable.
Rotator Cuff Strengthening Protocols
The rotator cuff is key for shoulder stability. It includes muscles and tendons around the shoulder. Strengthening these muscles is vital for better stability and function.
Exercises like internal and external rotations with resistance bands or light dumbbells work well. Internal rotation helps the subscapularis muscle, while external rotation targets the infraspinatus and teres minor. Do these exercises carefully, avoiding any pain.
Scapular Stabilization and Control Techniques
Scapular stabilization is just as important. It gives a solid base for the rotator cuff to work well. Exercises like scapular squeezes, wall slides, and scapular push-ups are helpful. They strengthen the serratus anterior, trapezius, and rhomboid muscles, which are key for scapular stability.
Good scapular control comes from coordinated movements. Rehabilitation should mix these exercises for full strengthening.
Preventing Re-Dislocations Through Strategic Strength Training
Strategic strength training is key to preventing re-dislocations and keeping your shoulder healthy. After a shoulder dislocation, the chance of it happening again is high if you don’t take steps to prevent it.
Risk Factors for Recurrent Dislocations
Several factors can make you more likely to have a shoulder dislocation again. These include:
- Inadequate rehabilitation after the initial dislocation
- Weakness in the shoulder muscles, like the rotator cuff
- Poor scapular stabilization
- Participation in high-risk sports or activities
Knowing these risk factors is key to creating a good prevention plan. A study in A Journal found that a strong rehabilitation program can lower the risk of dislocations.
Getting a thorough assessment from a healthcare professional is vital. They can spot your specific risk factors and create a prevention plan just for you.
Evidence-Based Preventative Exercise Strategies
Preventative exercises are important in lowering the risk of re-dislocations. Proven exercises include:
- Rotator cuff strengthening exercises, like internal and external rotations
- Scapular stabilization exercises, such as scapular push-ups and rows
- Progressive resistance training to boost overall shoulder strength
A study in A Journal that exercises focusing on the rotator cuff and scapular stabilizers can greatly improve shoulder stability. This can significantly lower the risk of re-dislocation.
By adding these exercises to your strength training routine, you can greatly reduce your chance of a re-dislocation. This helps keep your shoulder healthy for the long term.
Measuring Progress in Post-Dislocation Rehabilitation
Knowing how to track progress in post-dislocation rehab is key. It lets people see how far they’ve come, spot areas needing more work, and tweak their rehab plans. This helps a lot in getting better.
Objective Strength Testing Methods
Testing strength objectively is a big part of checking how well you’re recovering. It uses set methods to see how strong and functional your shoulder is. Some common ways include:
- Isometric strength testing to measure the maximum force without moving the joint.
- Isokinetic strength testing to check strength as you move through a range.
These tests give important info on muscle strength. They help both doctors and patients see if their rehab is working well.
Functional Assessment and Performance Metrics
Functional assessment looks at how well your shoulder does daily tasks and specific activities. Performance metrics might include:
- Range of motion exercises to check flexibility.
- Functional movement patterns that mimic daily or sports activities.
By watching these metrics, people can see how well they’re doing functionally. They can spot any issues or imbalances that need fixing.
Rehabilitation progress is more than just getting strong. It’s about being able to do everyday and sports activities too. By mixing strength tests with functional checks, you get a full picture of your recovery.
Athletes and Shoulder Dislocation: Special Considerations
Shoulder dislocations are a big challenge for athletes. They need a detailed plan to get back to their sport safely. This plan aims to rebuild strength and ensure they can play without risk.
Sport-Specific Rehabilitation Approaches
Rehab programs for athletes must fit their sport and role. For instance, a football quarterback’s rehab is different from a baseball pitcher’s. Sport-specific rehabilitation means exercises that match the athlete’s sport demands.
“Rehab plans should meet the athlete’s specific needs,” says a sports medicine expert. “They should focus on the movements and stresses of their sport.”
Return-to-Competition Strength Benchmarks
Knowing when an athlete is ready to play again is key. Return-to-competition strength benchmarks check shoulder strength, stability, and function. Athletes must show big gains in these areas before they can play again.
- Restoration of full range of motion
- Significant improvement in strength and endurance
- Ability to perform sport-specific tasks without pain or instability
To meet these benchmarks, athletes need a structured rehab plan. This plan should get progressively harder. By focusing on their sport and meeting strength benchmarks, athletes can safely get back to playing and perform well.
Psychological Aspects of Shoulder Strength Recovery
Recovering from a shoulder dislocation is tough, both physically and mentally. People face big challenges during rehab that can slow down their healing.
One big challenge is the fear of getting hurt again. This fear can stop people from doing things they need to do to get stronger. It’s key to beat this fear to recover well.
Overcoming Fear of Re-Injury
To get over the fear of getting hurt again, there are ways to help. Doing small steps towards activities you’ve been scared of can build your confidence. Thinking about doing things right and succeeding can also help.
Learning the right way to move and using tools to support you can make you feel safer. This can lower your anxiety.
“The greatest glory in living lies not in never falling, but in rising every time we fall.” – Nelson Mandela
This quote shows the strength needed to face the fear of getting hurt again. It’s about keeping going through tough times.
Mental Strategies for Optimal Rehabilitation
There are mental ways to make rehab better. Setting goals helps you see how far you’ve come and keeps you going. Being kind to yourself and imagining success can also help.
Practicing mindfulness can help you deal with stress and feel better overall. This makes the whole rehab process better.
Recovering from a shoulder dislocation needs a mix of physical and mental work. Focusing on the mental side can really help you get better faster.
Conclusion
Getting your shoulder strength back after a dislocation needs a full plan. This includes knowing about the injury, getting the right medical help, and following a detailed rehab program. The road to getting strong again is long, with healing tissues, building muscles, and making the joint stable.
A good shoulder rehabilitation summary shows the need for a step-by-step recovery. It starts with rest and managing pain, then moves to strengthening exercises. Focusing on the rotator cuff and scapular muscles helps a lot. This way, people can get their shoulder working better and avoid future problems.
The journey to full recovery depends on the injury’s severity, the treatment’s success, and how hard you work at rehab. A recovery conclusion says that with the right steps, many can see big improvements in shoulder strength after dislocation. This lets them go back to their usual activities and even sports.
FAQ
How long does it take to recover from a shoulder dislocation?
Recovery time for a shoulder dislocation varies. It depends on the injury’s severity, treatment, and your health. Generally, it can take weeks to months to get back full strength and mobility.
What are the most effective exercises for strengthening the shoulder after a dislocation?
Good exercises include rotator cuff strengthening and scapular stabilization. Use progressive resistance training and functional movements to regain strength and prevent future dislocations.
Can a shoulder dislocation lead to long-term strength deficits?
Some people may not regain full strength after a shoulder dislocation. This is more likely with severe injuries or complications during recovery. The success of your rehabilitation and any underlying conditions play a big role.
How can I prevent recurrent shoulder dislocations?
To prevent future dislocations, strengthen your shoulder muscles and improve stability. Avoid risky activities. Evidence-based exercises like rotator cuff strengthening and scapular stabilization are very effective.
What is the role of physical therapy in recovering from a shoulder dislocation?
Physical therapy is key in recovering from a shoulder dislocation. It helps restore motion, strengthen muscles, and improve stability. A good rehabilitation program can greatly improve recovery and reduce injury risk.
Are there any specific rehabilitation protocols for athletes with shoulder dislocations?
Athletes need sport-specific rehabilitation. These programs include exercises that match the athlete’s sport. This ensures a safe and effective return to competition.
How can I measure my progress during post-dislocation rehabilitation?
Progress can be measured with strength tests and functional assessments. Use dynamometry for strength and check range of motion and daily activity ability.
What are the psychological challenges of recovering from a shoulder dislocation?
Recovering can be tough mentally, with fears of re-injury and anxiety. Mental strategies like positive self-talk and visualization can help overcome these challenges.
Can shoulder dislocation recovery be influenced by underlying health conditions?
Yes, health conditions like diabetes or neurological disorders can affect recovery. Managing these conditions and adjusting your rehabilitation plan can improve outcomes.
References
- Sengupta, D.K., & Herkowitz, H.N. (2003). Lumbar spinal stenosis: Treatment strategies and indications for surgery. Orthopedic Clinics of North America, 34(2), 281-295. https://pubmed.ncbi.nlm.nih.gov/12914268/