Last Updated on November 20, 2025 by Ugurkan Demir
At Liv Hospital, we focus on caring for those with genetic blood disorders like sickle cell anemia. This condition changes the shape of red blood cells because of a problem with hemoglobin.
Sickle cell disease (SCD) includes several blood disorders, with sickle cell anemia being the most common. We know how important this condition is for families and medical experts.
Key Takeaways
- Sickle cell anemia is a genetic blood disorder affecting hemoglobin production.
- The disease causes red blood cells to take on a characteristic sickle shape.
- Understanding the genetic basis of the disease is key to effective management.
- Improved care pathways have enhanced patient outcomes and quality of life.
- Liv Hospital is dedicated to providing patient-centered care and innovative health solutions.
What Is Sickle Cell Anemia?

To understand Sickle Cell Anemia, we need to know its genetic roots and how it affects the body. It’s a genetic disorder that messes with hemoglobin production. Hemoglobin is a protein in red blood cells that carries oxygen.
Definition and Basic Characteristics
Sickle Cell Anemia is caused by abnormal hemoglobin, called Hemoglobin S (HbS). This abnormal hemoglobin makes red blood cells look like sickles, mainly when oxygen levels are low. These sickle-shaped cells are more likely to break down and get stuck in small blood vessels, causing health problems.
- Abnormal hemoglobin production
- Sickle-shaped red blood cells
- Increased risk of cell destruction
- Potential for blood vessel obstruction
The Role of Hemoglobin S (HbS)
Hemoglobin S (HbS) is the key player in Sickle Cell Anemia. A gene mutation leads to HbS production instead of normal hemoglobin. When oxygen levels drop, HbS forms polymers, causing red blood cells to sickle.
The polymerization of HbS is key to Sickle Cell Anemia. It’s what makes red blood cells sickle.
Historical Background and Terminology
Sickle Cell Anemia has been called many names over the years. “Drepanocytose” is one term used for it. It was first identified in the early 20th century. Ever since, we’ve learned a lot about its genetics and molecular aspects.
Our understanding of Sickle Cell Disease has grown. This is shown in how we now use different terms to describe it.
The Genetic Basis of Sickle Cell Anemia

Sickle cell anemia comes from a mutation in the HBB gene. This gene is key to making a part of hemoglobin. The mutation creates an abnormal hemoglobin called hemoglobin S (HbS).
Mutation in the HBB Gene
The HBB gene is on chromosome 11. It tells our bodies how to make a beta-globin subunit of hemoglobin. A mutation changes a glutamic acid to valine at the sixth position. This creates HbS, the main cause of sickle cell anemia.
Autosomal Recessive Inheritance Pattern
Sickle cell anemia follows an autosomal recessive pattern. This means you need two copies of the mutated HBB gene to have the disease. Carriers, with one normal and one mutated gene, usually don’t show symptoms but can pass the gene to their kids.
| Genotype | Phenotype | Description |
| Normal/Normal | Normal | No sickle cell gene |
| Normal/Mutated | Sickle Cell Trait | Carrier of the sickle cell gene |
| Mutated/Mutated | Sickle Cell Disease | Has the disease |
Sickle Cell Trait vs. Sickle Cell Disease
People with sickle cell trait have one mutated gene and usually don’t show symptoms. But they can pass the trait to their children. Those with sickle cell disease have two mutated genes and face serious health issues like chronic anemia and pain crises.
Knowing how sickle cell anemia is inherited is key to genetic counseling. It also helps in creating treatments to manage the disease.
Visualizing Sickle Cell Disease Through Diagrams
Diagrams are key in explaining sickle cell disease. They help us see how the condition affects the body. We can also see the difference between normal and sickle-shaped red blood cells.
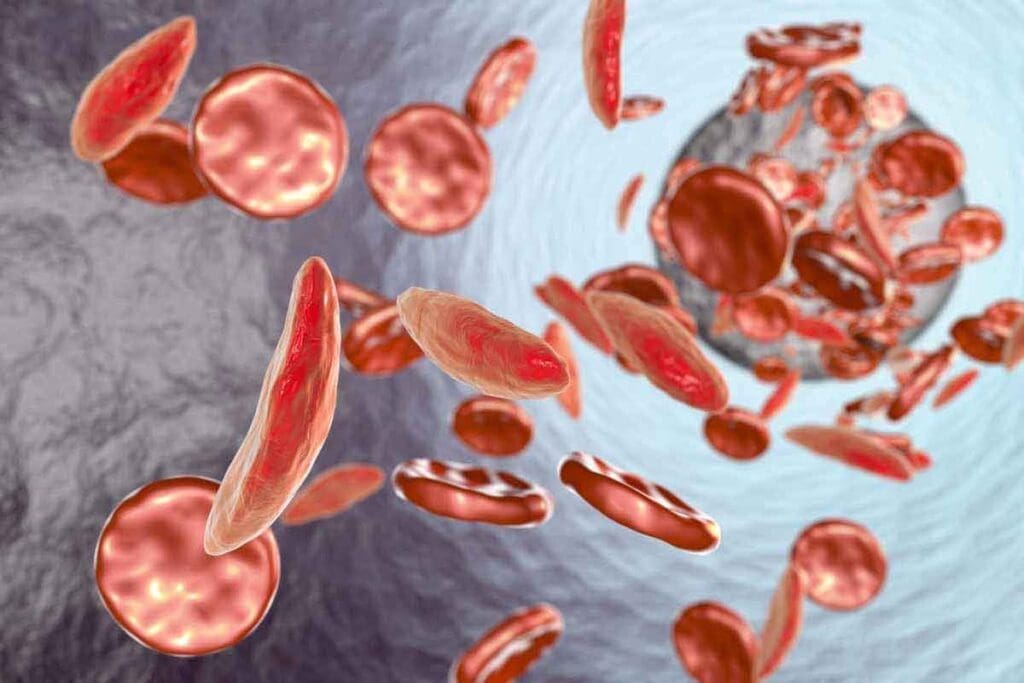
Normal vs. Sickle-Shaped Red Blood Cells
Understanding sickle cell disease starts with knowing the difference between normal and sickle-shaped red blood cells. Normal cells are flexible and disk-shaped, moving easily through blood vessels. Sickle-shaped cells, on the other hand, are rigid and crescent-shaped, making it hard for them to pass through smaller vessels.
How Sickle Cells Block Blood Vessels
Sickle cells can block blood vessels, causing many problems. When sickle cells clump together, they block blood flow. This leads to pain and damage to organs. It can also cause vaso-occlusive crises, a key feature of sickle cell disease.
The Process of Cell Sickling Under Low Oxygen
Cell sickling happens when red blood cells face low oxygen levels. In these conditions, the hemoglobin S (HbS) in sickle cells polymerizes. This makes the cells change shape and become rigid. When oxygen levels go back up, the cells can return to normal. But repeated episodes of sickling can cause cell damage.
The Molecular Mechanism of Sickle Cell Anemia
To grasp sickle cell anemia, we must look at hemoglobin’s structure and role. Hemoglobin is key in red blood cells, carrying oxygen to our body’s tissues. A mutation in the HBB gene causes abnormal hemoglobin, known as Hemoglobin S (HbS), in sickle cell anemia.
Hemoglobin Structure and Function
Hemoglobin is made of four chains: two alpha and two beta. In normal hemoglobin (HbA), the beta chains come from the HBB gene. The sickle cell mutation changes a glutamic acid to valine in the beta chain, creating HbS. This change affects hemoglobin’s properties, mainly when oxygen levels are low.
The structure of hemoglobin is vital for its job. Its tetrameric shape helps it bind oxygen cooperatively. This allows oxygen to be released to tissues. The HbS mutation creates a hydrophobic patch on the beta chains. This patch can interact with other HbS molecules, causing them to stick together.
How Hemoglobin S Polymerizes
When oxygen levels are low, HbS molecules stick together, forming long fibers. This is the main cause of sickle cell anemia. At first, this process can be reversed, but as the fibers grow, it becomes permanent.
- The polymerization of HbS is influenced by several factors, including the concentration of HbS, the presence of other hemoglobins, and the oxygen tension.
- Deoxygenation of HbS exposes the hydrophobic patches, facilitating the interaction between HbS molecules and the formation of polymers.
- The rate and extent of polymerization determine the severity of the disease.
Cell Distortion and Membrane Damage
The polymerization of HbS changes red blood cells into sickle shapes. This happens because the rigid fibers push against the cell membrane. This changes the cell’s shape and flexibility.
The repeated cycles of sickling and unsickling damage the cell membrane. The cells become less flexible and more likely to break down. This leads to anemia. Also, sickled cells can stick to the endothelium, causing vaso-occlusive crises.
Knowing these molecular mechanisms is key to finding new treatments. Treatments aim to stop or reverse HbS polymerization. This could help ease the symptoms and complications of sickle cell anemia.
Clinical Manifestations and Complications
Sickle cell anemia shows many symptoms that can really affect a person’s life. It impacts many parts of the body, causing different problems.
Chronic Anemia and Its Effects
Chronic anemia is a big problem in sickle cell anemia. It happens because red blood cells die early. This can make you feel tired, weak, and short of breath. It’s important to manage this to improve life for those with sickle cell anemia.
Vaso-Occlusive Pain Crises
Vaso-occlusive pain crises are a big issue in sickle cell disease. They happen when sickled red blood cells block blood vessels. This causes pain and tissue damage. Finding good ways to manage pain is key.
Increased Susceptibility to Infections
People with sickle cell anemia get sick more easily. This is because their spleen doesn’t work right and their immune system is weak. Getting sick can make their condition worse. It’s important to prevent infections with vaccines and antibiotics.
Organ Damage and Long-Term Complications
Sickle cell disease can damage organs over time. This includes stroke, bone damage, and heart and lung problems. It’s important to watch closely and act early to prevent these problems.
| Complication | Description | Management Strategies |
| Chronic Anemia | Premature destruction of red blood cells leading to fatigue and weakness | Blood transfusions, iron chelation therapy |
| Vaso-Occlusive Pain Crises | Obstruction of blood vessels by sickled red blood cells causes pain | Pain management medications, hydration |
| Increased Susceptibility to Infections | Impaired immune function increases the risk of infections | Prophylactic antibiotics, vaccinations |
| Organ Damage | Long-term damage to organs such as the spleen, kidneys, and heart | Regular monitoring, early intervention |
Epidemiology and Global Distribution
Sickle cell anemia shows a complex pattern around the world. It’s linked to areas where malaria was once common. It’s a big health issue in sub-Saharan Africa, the Mediterranean, and the Middle East.
Prevalence in African Populations
In sub-Saharan Africa, sickle cell disease is very common. Countries like Nigeria, the Democratic Republic of Congo, and Uganda have high rates. We’ll look at these rates and what they mean for health care.
Studies show sickle cell trait is found in 25-30% of some Africans. This is important for genetic advice and managing the disease.
Mediterranean and Middle Eastern Prevalence
In the Mediterranean and the Middle East, sickle cell disease is also common. Places like Greece, Turkey, and Saudi Arabia have seen many cases. This is tied to the history of malaria in these areas.
The Evolutionary Advantage: Malaria Protection
The sickle cell trait helps protect against malaria, mainly Plasmodium falciparum. People with this trait get less severe malaria. This has made the HbS allele more common in malaria areas.
Malaria protection is why the sickle cell trait is so common in these areas. This helps us understand why the disease is spread out the way it is.
Current Global Statistics
Worldwide, sickle cell disease affects millions. The World Health Organization says about 300,000 children are born with it each year. Most of these are in sub-Saharan Africa.
| Region | Estimated Prevalence | Annual Births with SCD |
| Sub-Saharan Africa | High | 240,000 |
| Mediterranean | Moderate | 10,000 |
| Middle East | Moderate | 8,000 |
| Global | – | 300,000 |
These numbers show we need to keep working on sickle cell disease worldwide.
Diagnosis and Modern Treatment Approaches
Today, diagnosing and treating sickle cell anemia is much better than before. Accurate diagnosis is key to managing the condition well.
Diagnostic Tests and Procedures
A blood test is used to find Hemoglobin S (HbS), the abnormal hemoglobin in sickle cell anemia. This test is often done on newborns in many places. If not done at birth, diagnosis might happen later due to symptoms or problems.
Genetic tests can also find the HBB gene mutation causing the disease. These tests can spot carriers of the sickle cell trait, too.
Traditional Management Strategies
Older ways to manage sickle cell anemia include:
- Vaccinations to prevent infections
- Antibiotics to treat infections
- Pain management through medication and hydration
- Blood transfusions to reduce sickling red blood cells
These methods have been used for many years to help manage the disease.
Recent Advances in Therapy
New treatments for sickle cell disease have emerged. Gene therapy is one of the most promising, aiming to fix the genetic issue. A study in Journal of Hematology & Oncology shows gene therapy’s promise in reducing sickle cell anemia’s severity.
New medicines can also lessen pain crises and improve life quality for patients. These new treatments are more focused and effective.
There’s a big change in how we manage sickle cell anemia. This change comes from better medical technology and understanding the disease’s genetics.
Living with Sickle Cell Anemia: Patient Care Pathways
Managing sickle cell anemia needs a detailed plan. We know patients need care that covers their health, feelings, and social life.
Comprehensive Care Models
Comprehensive care is key for sickle cell anemia. A team of doctors, nurses, and social workers work together. They focus on regular check-ups, watching for problems, and teaching patients.
- Regular health assessments to monitor the condition
- Access to specialized care, such as hematology and pain management
- Patient and family education on managing the condition
Pain Management Strategies
Pain control is vital for sickle cell anemia patients. It uses medicine and other methods. We make sure each patient gets a pain plan that fits them.
“Pain is a hallmark of sickle cell disease, and effective management requires a multidisciplinary approach.”
Medical Expert in Hematology
Preventive Measures and Lifestyle Adaptations
Preventive steps and lifestyle changes help manage sickle cell anemia. Patients should drink plenty of water, avoid extreme weather, and eat well. Exercise like walking or swimming can also help.
| Preventive Measure | Benefit |
| Staying hydrated | Reduces risk of dehydration-induced crises |
| Avoiding extreme temperatures | Minimizes risk of temperature-related complications |
Support Systems and Resources
Support and resources are essential for sickle cell anemia patients. We suggest joining support groups, online or in-person, for emotional support. It’s also important to have access to counseling for mental health.
With a complete care plan, patients with sickle cell anemia can manage their condition better. We aim to provide the support and resources needed for effective care.
Conclusion: Future Directions in Sickle Cell Research and Treatment
Understanding sickle cell anemia is complex. Yet, ongoing research is key to better patient care. New treatments, like gene therapy, aim to fix the disease’s root causes.
Recent therapy breakthroughs are exciting. We expect more progress soon. These advances will improve life for sickle cell patients globally. Our goal is to lead in healthcare, supporting patients everywhere.
We’re committed to finding new ways to help sickle cell patients. Our mission is to offer effective, tailored care. We support patients and families, giving them the help they need to succeed.
FAQ
What is sickle cell anemia?
Sickle cell anemia is a blood disorder caused by a specific gene. It makes red blood cells shape abnormally.
What is the genetic basis of sickle cell anemia?
It’s caused by a mutation in the HBB gene. This gene is inherited in an autosomal recessive pattern.
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait has one HbS gene. Sickle cell disease has two leading to more severe symptoms.
How do sickle cells affect the body?
Sickle cells can block blood vessels. This causes pain crises, chronic anemia, and makes infections more likely.
What is the role of hemoglobin S (HbS) in sickle cell anemia?
Hemoglobin S (HbS) is an abnormal hemoglobin. It changes shape under low oxygen, damaging red blood cells.
How is sickle cell anemia diagnosed?
Blood tests, like hemoglobin electrophoresis and genetic testing, are used for diagnosis.
What are the clinical manifestations of sickle cell anemia?
Symptoms include chronic anemia, pain crises, increased infection risk, and organ damage over time.
What is the prevalence of sickle cell anemia in different populations?
It’s common in African, Mediterranean, and Middle Eastern populations. It offers protection against malaria.
What are the current treatment options for sickle cell anemia?
Treatments include pain management, blood transfusions, and newer options like gene therapy.
How can patients with sickle cell anemia manage their condition?
Patients can manage through care models, pain strategies, preventive measures, and lifestyle changes. Support systems and resources also help.
What is the evolutionary advantage of the sickle cell trait?
The sickle cell trait offers protection against malaria. This is why it’s naturally selected in certain populations.
What are the long-term complications of sickle cell anemia?
Long-term complications include organ damage, like kidney issues and stroke risk. Other systemic effects also occur.
References
- GeneReviews® Editorial Board. (2013). Sickle cell disease: Genetics, pathophysiology, clinical features. https://www.ncbi.nlm.nih.gov/books/NBK1377/
- Kato, G. J., Piel, F. B., Reid, C., et al. (2018). Sickle cell disease. Nature Reviews Disease Primers, 4, 18010. https://www.nature.com/articles/nrdp201810
- World Health Organization. (2024, June). Sickle-cell disease fact sheet. https://www.who.int/news-room/fact-sheets/detail/sickle-cell-disease
- Centers for Disease Control and Prevention. (2023). Data & statistics on sickle cell disease. https://www.cdc.gov/sickle-cell/data/index.htm