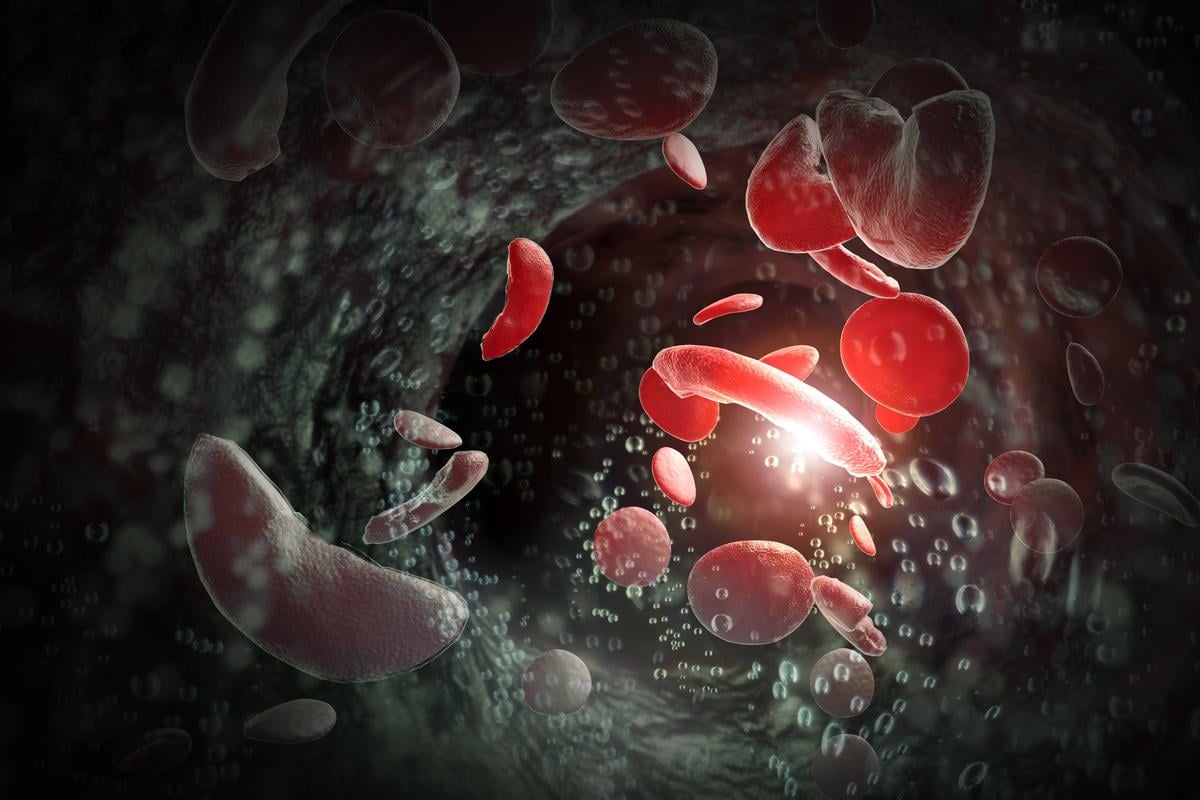
Sickle cell crisis is a serious condition marked by severe pain episodes, also called vaso-occlusive pain episodes. These are a key feature of sickle cell disease symptoms. Such episodes occur when abnormal red blood cells block blood vessels, leading to tissue ischemia and intense pain.
Vaso-occlusive pain episodes are not just painful. They also raise the risk of serious complications like organ damage and higher mortality. It’s important to understand these risks to manage and treat the condition effectively.
Key Takeaways
- Vaso-occlusive pain episodes are the most common complication of sickle cell crisis.
- These episodes can lead to tissue ischemia and organ damage.
- Frequent vaso-occlusive episodes are associated with increased mortality.
- Effective management of vaso-occlusive pain episodes is critical to prevent long-term complications.
- Patient-reported pain is an independent predictor of mortality in individuals with sickle cell disease.
Understanding Sickle Cell Disease and Its Pathophysiology
It’s important to know the genetic cause of sickle cell disease to understand how it works. Sickle cell disease (SCD) is a genetic disorder. It happens because of a mutation in the HBB gene, which codes for a part of hemoglobin.
The Genetic Basis of Sickle Cell Disease
SCD is passed down in an autosomal recessive pattern. This means a person needs two defective HBB genes (one from each parent) to have the disease. This genetic change leads to the creation of abnormal hemoglobin, known as sickle hemoglobin or HbS.
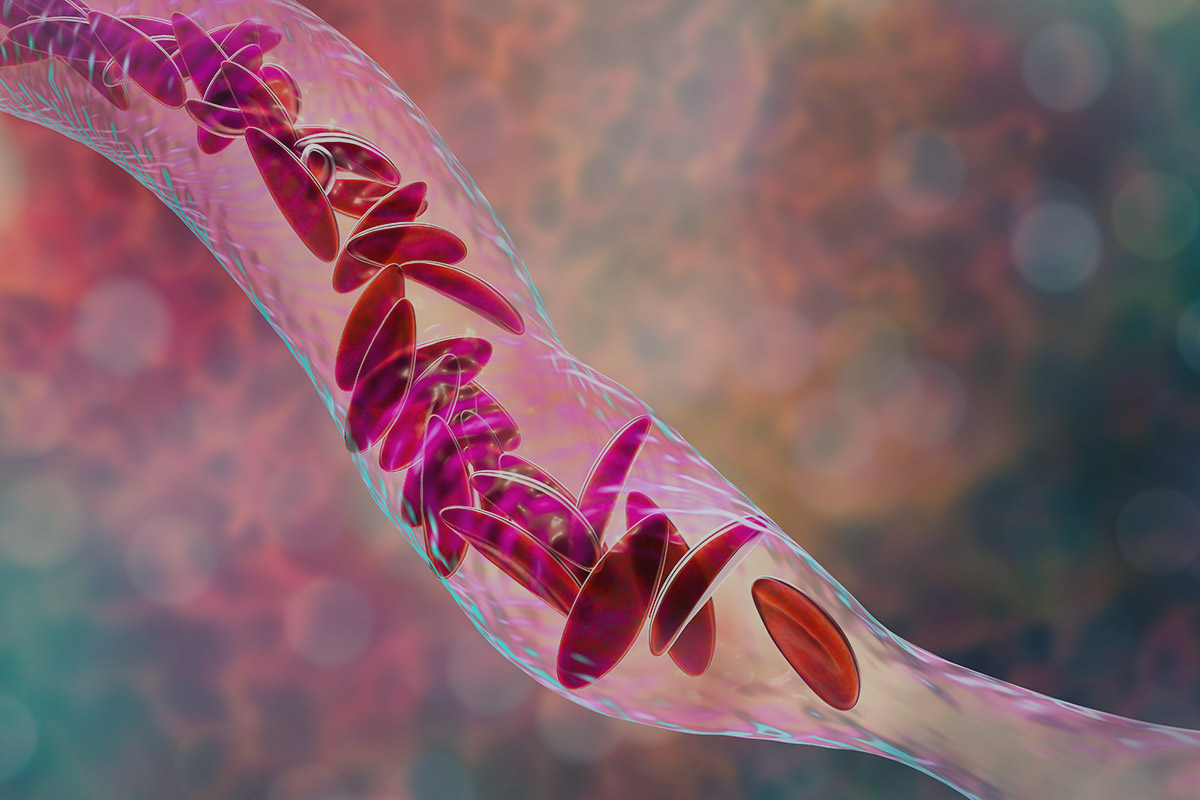
How Abnormal Hemoglobin Affects Red Blood Cells
Abnormal hemoglobin makes red blood cells bend into a sickle shape when oxygen levels are low. These sickled red blood cells break down faster and can block small blood vessels. This can cause many problems.
The main signs of SCD include:
- Anemia: Because red blood cells don’t last as long.
- Vaso-occlusive crises: When sickled red blood cells block blood vessels.
- Increased risk of infections: Because the spleen doesn’t work properly.
Common Sickle Cell Disease Symptoms and Their Progression
One of the most recognized sickle cell disease symptoms is vaso-occlusive pain episodes. Vaso-occlusive pain episodes are a big problem for sickle cell disease patients. These episodes happen when sickled red blood cells block blood vessels. This causes tissue ischemia and pain.
Vaso-Occlusive Pain Episodes as the Most Frequent Complication
Vaso-occlusive crises cause severe pain in different body parts. This includes the back, legs, arms, and chest. The pain can be sudden or last a long time, and it’s different for everyone.
Managing these episodes needs a few steps. This includes staying hydrated, using medicine for pain, and sometimes getting blood transfusions.
Triggers and Risk Factors for Crisis
Many things can set off vaso-occlusive crises. These include infections, not drinking enough water, extreme weather, and too much physical activity. Knowing what triggers these crises is key to avoiding them.
- Infections
- Dehydration
- Extreme temperatures
- Physical stress
Management Approaches for Pain Episodes
Handling vaso-occlusive pain episodes well needs a mix of prevention and quick action. Patients should drink plenty of water, stay away from extreme weather, and handle stress well.
When a crisis hits, pain management is very important. Doctors might use NSAIDs, opioids, or other painkillers. Sometimes, patients need to go to the hospital for severe cases.
Acute Chest Syndrome: The Deadliest Complication
SCD has many complications, but ACS is the deadliest. It’s a new lung issue seen on X-rays, often with fever, breathing problems, or chest pain. It’s a top reason for sickness and death in SCD patients.
Clinical Presentation and Diagnostic Criteria
ACS symptoms can vary but often include cough, chest pain, and trouble breathing. Doctors look for a new lung issue on X-rays and symptoms like fever and pain. A chest X-ray showing a new lung issue is key to diagnosis.
Key diagnostic features include:
- New pulmonary infiltrate on chest radiograph
- Fever
- Respiratory symptoms
- Chest pain
Why ACS Accounts for 25% of SCD Deaths
ACS is a big reason for death in SCD patients. It quickly gets worse and can lead to serious breathing problems. Its high death rate comes from its complex causes, like blockages, infections, and fat in the blood.
Treatment Protocols and Prevention Strategies
Quick action is key in treating ACS. Treatment includes:
- Supplemental oxygen and hydration
- Broad-spectrum antibiotics
- Pain management
- Blood transfusion in severe cases
Preventing ACS is also important. This includes:
- Regular check-ups and monitoring
- Pneumococcal vaccination
- Quick action on pain episodes
Understanding and treating ACS is vital for better outcomes in SCD patients.
Stroke and Neurological Complications in SCD Patients
SCD patients face a big risk of neurological problems, with stroke being the most severe. This risk is not just for kids; it also affects adults. So, ongoing care is key.

Age-Related Risk of Cerebrovascular Events
The risk of stroke in SCD patients grows with age. By age 19, about 11% have had a stroke. By 45, this number jumps to 24%. This shows why monitoring is important at all ages.
Silent Cerebral Infarcts vs. Overt Stroke
Neurological issues in SCD can show up as overt strokes or silent cerebral infarcts (SCI). It’s important to know the difference for good management.
Overt strokes have clear signs of brain damage. SCI, though, doesn’t show symptoms but can cause brain problems. Regular checks are vital.
Screening and Prevention Measures
SCD patients should get screened for stroke risk early, starting at 2. Transcranial Doppler (TCD) ultrasonography helps spot high-risk patients. Prevention includes chronic blood transfusions for those at high risk.
A leading doctor says, “Early detection and action are key to lowering stroke and brain problem risks in SCD patients.”
“Screening programs have greatly cut down stroke rates in kids with SCD.”
Renal Dysfunction and Progressive Kidney Damage
Sickle Cell Disease can cause serious kidney problems. Over 20% of adults with SCD face kidney issues. This greatly affects their quality of life.
Pathophysiology of Kidney Injury
In SCD, sickled red blood cells block tiny blood vessels in the kidneys. This causes damage and can harm kidney function over time.
Progression from Microalbuminuria to End-Stage Renal Disease
Microalbuminuria is an early sign of kidney damage in SCD patients. If not treated, it can lead to severe kidney failure. This means patients might need dialysis or a kidney transplant.
Management of Renal Complications requires a detailed plan. This includes:
- Monitoring for microalbuminuria and proteinuria
- Controlling blood pressure with ACE inhibitors or ARBs
- Avoiding harmful drugs for the kidneys
- Using hydroxyurea to manage SCD and slow kidney disease
Early detection and treatment of kidney problems are key. Understanding how kidney damage happens helps doctors take action. They can slow or stop kidney disease from getting worse.
Infection Susceptibility Due to Functional Asplenia
The spleen is key to our immune system. In SCD patients, the damage increases the risk. Functional asplenia, where the spleen doesn’t work right, is a big problem in sickle cell disease.
The Role of the Spleen in Immune Function
The spleen filters blood and stores lymphocytes. It keeps pathogens out of the bloodstream, protecting us from infections. In SCD, splenic damage from vaso-occlusive crises can lead to functional asplenia.
Common Pathogens and Infection Types
SCD patients with functional asplenia face a big risk of infections. Streptococcus pneumoniae is a major concern. Other pathogens like Haemophilus influenzae and Neisseria meningitidis are also dangerous. These infections can be deadly if not treated quickly.
Vaccination and Prophylactic Antibiotics
To lower infection risk, SCD patients should get vaccinated. Shots against pneumococcus, meningococcus, and Haemophilus influenzae type b are key. Prophylactic antibiotics, like penicillin, are also a must, mainly for kids. These steps can greatly cut down infection rates in SCD patients.
Additional Complications and Long-Term Effects
SCD is more than just its main symptoms. It can lead to many long-term problems. These issues can greatly affect a person’s quality.
Acute Splenic Sequestration
Acute splenic sequestration is very dangerous. It happens when red blood cells get stuck in the spleen. This causes a sudden drop in hemoglobin levels. It’s a medical emergency that needs quick attention to avoid severe anemia and death.
Priapism and Reproductive Health Issues
Priapism, or long-lasting erections, is a big problem for men with SCD. It can cause erectile dysfunction if not treated. SCD also affects reproductive health in both men and women. This means careful management is needed to lessen these effects.
Avascular Necrosis and Bone Complications
Avascular necrosis, like in the femoral head, is a big worry. It happens when blood stops reaching the bone, causing it to die. This might need surgery. For more on SCD management and complications, check out Frontiers in Pediatrics.
It’s key to know about these extra problems and the long-term effects of SCD. By tackling these issues, doctors can help patients live better lives.
Conclusion: Modern Management and Life Expectancy
Sickle cell disease (SCD) cuts life expectancy by over 20 years in high-income countries. Modern management and new healthcare solutions are key to a better quality of life and longer life for SCD patients.
LivHospital leads in providing the latest academic care with top health standards. It uses new healthcare solutions to improve SCD management. This helps tackle its many complications and boosts patient results.
Improving SCD patients’ life expectancy requires complete care. This includes managing pain, chest issues, stroke, and other problems. Modern care methods, like advanced treatments and prevention, are essential.
Healthcare providers like LivHospital can greatly change SCD patients’ lives. They focus on new healthcare solutions and modern management. This improves patients’ quality and life expectancy.
FAQ’s:
What is sickle cell disease?
Sickle cell disease (SCD) is a genetic disorder. It affects how red blood cells make hemoglobin. This makes the cells misshapen, and they break down.
What are the most common complications of sickle cell disease?
Common complications include vaso-occlusive pain episodes and acute chest syndrome. Stroke and renal dysfunction are also common.
What is a vaso-occlusive pain episode?
A vaso-occlusive pain episode is a painful crisis. It happens when sickled red blood cells block blood vessels. This reduces blood flow to organs and tissues.
What triggers a sickle cell crisis?
Triggers include dehydration, infection, extreme temperatures, and stress.
How is acute chest syndrome diagnosed?
It’s diagnosed with a chest X-ray and lab tests. These include oxygen saturation and blood counts.
What is the risk of stroke in SCD patients?
SCD patients face a higher risk of stroke, more so in children. This is due to abnormal blood flow and vessel damage.
How can renal complications be managed in SCD patients?
Managing renal complications involves monitoring kidney function and blood pressure. Keeping hydrated helps prevent kidney damage.
Why are SCD patients more susceptible to infections?
They are more at risk due to functional asplenia. This is when the spleen is damaged and can’t filter pathogens.
What are the common pathogens that infect SCD patients?
Common pathogens include Streptococcus pneumoniae, Haemophilus influenzae, and Salmonella species.
How can SCD patients prevent infections?
Preventing infections involves vaccination, prophylactic antibiotics, and good hygiene.
What is the role of LivHospital in managing SCD?
LivHospital aims to improve life expectancy and quality of life for SCD patients. They provide modern management and innovative healthcare solutions.
References
- National Heart, Lung, and Blood Institute. (2014). Evidence-based management of sickle cell disease: Expert panel report. Retrieved from https://www.nhlbi.nih.gov/health-topics/sickle-cell-disease/management
- Centers for Disease Control and Prevention. (2020). Data & Statistics on Sickle Cell Disease. Retrieved from https://www.cdc.gov/ncbddd/sicklecell/data.html























