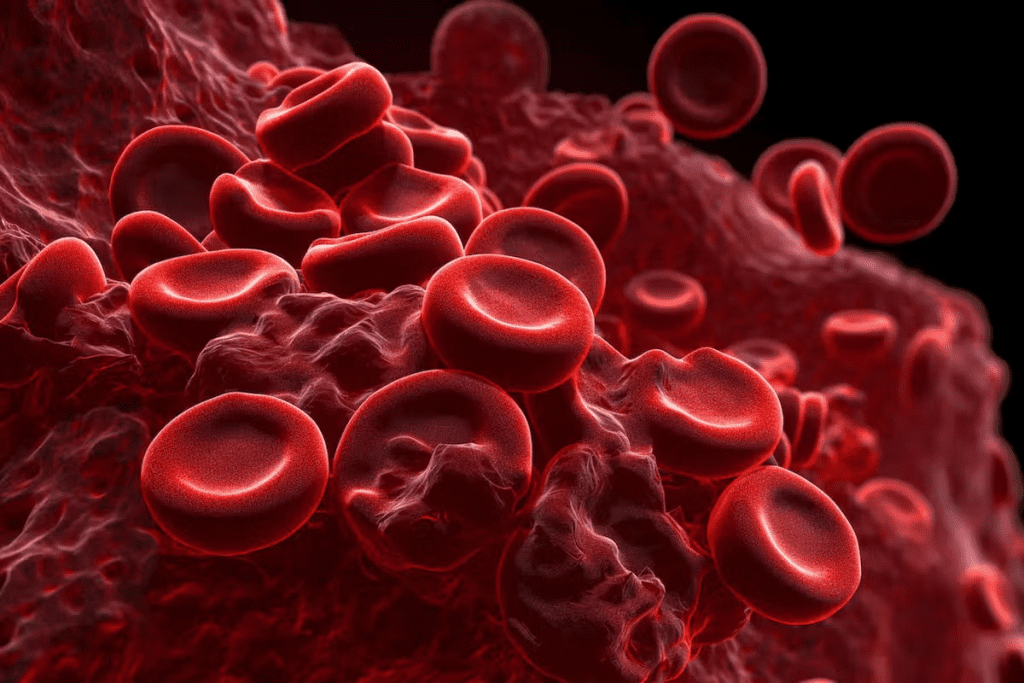
Sickle cell disease traits are linked to a genetic disorder that alters red blood cells, reducing their ability to carry oxygen effectively. A striking 100,000 people in the United States live with this condition. It causes chronic anemia, pain crises, and other serious health issues.
The genetic mutation behind sickle cell disease leads to abnormal hemoglobin S (HbS). This makes red blood cells misshapen and short-lived. As a result, the body doesn’t get enough oxygen, leading to anemia and various complications.
Key Takeaways
- Anemia in sickle cell disease is caused by a genetic mutation affecting hemoglobin production.
- The condition leads to the production of abnormal hemoglobin S (HbS).
- Red blood cells become misshapen and break down prematurely, resulting in anemia.
- Chronic anemia is a hallmark of sickle cell disease, along with recurrent pain crises.
- Understanding the genetic basis of SCD is key to finding effective treatments.
Understanding Sickle Cell Disease

It’s important to know about sickle cell disease to understand its global health impact. SCD is a genetic disorder that changes the hemoglobin in red blood cells. This makes them sickle-shaped, causing blood flow problems and health issues.
Definition and Prevalence
Sickle cell disease is caused by abnormal hemoglobin, called hemoglobin S. It’s inherited in a way that requires two defective genes. This is why it’s common in areas where malaria was once widespread, as it offers some protection against it. About 7% of the world’s population has the sickle cell trait.
The disease is most common in Africa, the Mediterranean, the Middle East, and parts of South Asia. In the U.S., it affects many, mainly those of African descent.
Historical Background
Sickle cell disease has been around for centuries, found in many cultures. It was first documented in the early 1900s by James Herrick. He noticed sickle-shaped red blood cells in a patient. Ever after, scientists have made big strides in understanding SCD’s genetics and molecular mechanisms.
Back then, SCD was often deadly, mainly in children. But, thanks to better medical care, people with SCD now live longer.
Global Distribution
The spread of sickle cell disease is tied to malaria. Places with lots of malaria also have more sickle cell trait. This is because the trait helps protect against malaria. So, SCD is common in sub-Saharan Africa, the Mediterranean, and parts of the Middle East and South Asia.
In the U.S., newborn screenings have found SCD in people from many ethnic backgrounds. This shows we need to be aware and screen for it in all populations.
The Genetic Basis of Sickle Cell Disease
A specific mutation in the β-globin gene causes Sickle Cell Disease. This mutation leads to abnormal hemoglobin, called Hemoglobin S (HbS).
Hemoglobin S Mutation
The hemoglobin S mutation happens when glutamic acid is swapped with valine at the sixth position of the β-globin chain. This change makes HbS form clumps under low oxygen, causing red blood cells to sickle.
This mutation is a point change in the HBB gene, which codes for the β-globin part of hemoglobin. Knowing about this mutation is key for diagnosing and treating Sickle Cell Disease.
Inheritance Patterns
Sickle Cell Disease follows an autosomal recessive inheritance pattern. This means a person needs two defective HBB genes, one from each parent, to have the disease.
Carriers, who have one normal and one mutated gene, usually don’t show all the disease symptoms. But they can pass the mutated gene to their kids.
Genetic Variations and Disease Severity
Genetic variations greatly affect how severe Sickle Cell Disease is. Things like other genetic changes, fetal hemoglobin levels, and having other hemoglobinopathies can change how the disease shows up.
For example, more fetal hemoglobin can make the disease less severe. It does this by stopping HbS from forming clumps.
Sickle Cell Disease Traits: Carrier Status vs. Disease
Carrying the sickle cell gene is not the same as having sickle cell disease. It’s important to know the difference. This helps us understand how sickle cell trait affects people and their children.
Heterozygous vs. Homozygous States
People can be either heterozygous or homozygous for sickle cell disease. Heterozygous individuals have one normal and one sickle cell gene. They are carriers but usually don’t have severe symptoms. Homozygous individuals have two sickle cell genes. They have the full disease and its symptoms.
| Genetic State | Hemoglobin Genes | Disease Status |
| Heterozygous | 1 Normal, 1 Sickle Cell | Carrier, generally asymptomatic |
| Homozygous | 2 Sickle Cell | Disease state, symptomatic |
Sickle Cell Trait Characteristics
People with sickle cell trait are usually healthy. They don’t show the severe symptoms of sickle cell disease. But, they might face problems at high altitudes or during intense exercise. Their red blood cells have both normal and sickle hemoglobin.
Protective Effects of Sickle Cell Trait
The sickle cell trait helps protect against malaria. This is a big plus in places where malaria is common. Studies show that having the sickle cell gene helps fight off some malaria parasites. This is why the trait is more common in malaria-prone areas.
In conclusion, knowing the difference between being a carrier and having sickle cell disease is key. It helps with genetic counseling and understanding the trait’s benefits against infections.
Normal Hemoglobin Function vs. Hemoglobin S
It’s important to know how normal hemoglobin and hemoglobin S differ. Normal hemoglobin, or Hemoglobin A (HbA), is key in moving oxygen around the body.
Structure and Function of Normal Hemoglobin
Normal hemoglobin is a protein in red blood cells. It carries oxygen from the lungs to the body’s tissues. It has four polypeptide chains and four heme groups, which hold iron.
Key characteristics of normal hemoglobin include:
- High affinity for oxygen, allowing it to pick up oxygen in the lungs.
- Ability to release oxygen to tissues, where it is needed for metabolism.
- A specific structure that prevents polymerization under normal conditions.
How Hemoglobin S Differs
Hemoglobin S (HbS) is an abnormal form of hemoglobin. It’s caused by a mutation in the HBB gene. This mutation changes glutamic acid to valine at the sixth position of the beta-globin chain.
| Characteristics | Normal Hemoglobin (HbA) | Hemoglobin S (HbS) |
| Structure | Normal alpha and beta chains | Mutated beta chains (Glu6Val) |
| Oxygen Affinity | High affinity for oxygen | Lower affinity for oxygen; prone to polymerization under low oxygen conditions |
| Polymerization | Does not polymerize | Polymerizes under low oxygen conditions, leading to sickling |
Oxygen Transport Abnormalities
The differences between HbA and HbS affect oxygen transport. HbS polymerizes under low oxygen, causing red blood cells to become rigid and break down. This leads to anemia and poor oxygen transport.
The oxygen transport issues caused by HbS are key in Sickle Cell Disease. They lead to pain episodes and organ damage.
The Sickling Process: Molecular Mechanisms
Understanding the molecular mechanisms behind sickling is key to treating sickle cell disease. The sickling process involves complex events that change red blood cells’ shape.
Triggers for Sickling
The main trigger for sickling is low oxygen levels. When red blood cells face hypoxia, hemoglobin S (HbS) polymerizes. This changes the red blood cell’s shape, starting the sickling process.
Polymerization of Hemoglobin S
The polymerization of HbS is a key event in sickling. In low oxygen, HbS molecules form long, rigid polymers. These distort the red blood cell membrane, making it sickle-shaped. This polymerization process is initially reversible but becomes permanent with repeated cycles.
Cellular Changes During Sickling
When red blood cells sickle, they undergo significant changes. These include changes in membrane flexibility and permeability. These changes lead to dehydration and increased rigidity, making cells more prone to hemolysis. Repeated sickling and unsickling cycles cause cumulative damage to red blood cells.
Reversibility of Sickling
At first, sickling is reversible; when oxygen levels rise, HbS polymers dissolve, and cells regain their shape. But with repeated sickling, cells become less able to return to normal. This leads to chronic hemolysis and complications of sickle cell disease.
Primary Mechanisms of Anemia in Sickle Cell Disease
Understanding anemia in SCD is key to managing the disease. Anemia in SCD comes from several factors that affect oxygen delivery to tissues.
Hemolysis: Destruction of Red Blood Cells
Hemolysis, or the destruction of red blood cells, is a major cause of anemia in SCD. The abnormal hemoglobin S makes red blood cells rigid and prone to destruction. This happens either inside or outside the blood vessels.
Intravascular hemolysis is when red blood cells are destroyed in the blood. This releases hemoglobin into the bloodstream. It can cause problems like a lack of nitric oxide, which is important for blood vessels.
Decreased Red Blood Cell Production
SCD also leads to a decrease in red blood cell production. The bone marrow struggles to make new red blood cells because of chronic inflammation and oxidative stress.
Splenic Sequestration
Splenic sequestration is another factor in anemia in SCD. The spleen can grow and trap red blood cells. This removes them from circulation, making anemia worse.
Cumulative Effects on Oxygen Delivery
The effects of hemolysis, decreased red blood cell production, and splenic sequestration reduce oxygen delivery to tissues. This can cause symptoms like fatigue, shortness of breath, and even organ dysfunction in severe cases.
The complex nature of these mechanisms highlights the need for a thorough approach to manage anemia in SCD.
Hemolytic Anemia in Detail
Hemolytic anemia is a key feature of sickle cell disease. It causes red blood cells to break down too early. This greatly affects the lives of those with sickle cell disease.
Intravascular Hemolysis
Intravascular hemolysis is when red blood cells break down inside blood vessels. This is a big part of hemolytic anemia in sickle cell disease. The sickle-shaped red blood cells are more likely to break down.
Mechanisms of intravascular hemolysis involve several cellular pathways. These pathways cause red blood cells to break down. This releases hemoglobin into the blood, which can cause more problems.
Extravascular Hemolysis
Extravascular hemolysis happens outside blood vessels, mainly in the spleen. The spleen filters out abnormal red blood cells. But in sickle cell disease, the spleen often doesn’t work right because of vaso-occlusion.
The spleen’s role in extravascular hemolysis is very important. It removes damaged red blood cells and stores others. If the spleen gets too full, it can trap red blood cells and platelets, causing severe anemia.
Markers of Hemolysis
There are several markers that show how severe hemolysis is in sickle cell disease. These include high levels of lactate dehydrogenase (LDH), bilirubin, and reticulocytes. Checking these markers helps doctors understand how bad the hemolytic anemia is.
| Marker | Significance |
| Lactate Dehydrogenase (LDH) | Elevated LDH levels indicate increased red blood cell destruction. |
| Bilirubin | High bilirubin levels suggest increased hemolysis, leading to jaundice. |
| Reticulocyte Count | An elevated reticulocyte count indicates the bone marrow’s response to anemia by producing more red blood cells. |
Consequences of Chronic Hemolysis
Chronic hemolysis in sickle cell disease has many serious effects. These include chronic anemia, jaundice, and a higher risk of gallstones and pulmonary hypertension.
“Chronic hemolysis is a major contributor to the morbidity associated with sickle cell disease, necessitating a wide range of management strategies to lessen its impact.”
Managing chronic hemolysis requires a variety of approaches. This includes medicines, blood transfusions, and supportive care. These help reduce symptoms and prevent further problems.
Clinical Manifestations of Anemia in Sickle Cell Disease
Anemia in SCD shows many symptoms, from sudden pain to ongoing tiredness. These symptoms greatly affect a person’s life and need careful management.
Acute vs. Chronic Symptoms
SCD patients face both sudden and ongoing symptoms of anemia. Sudden symptoms, like pain crises, happen when sickled blood cells block blood vessels. These crises can be caused by dehydration, infections, or extreme weather.
Long-term symptoms come from constant blood loss and anemia. These include feeling very tired, looking pale, and having trouble breathing. Long-term anemia can also cause heart problems and slow growth in kids.
Age-Related Presentations
Anemia symptoms in SCD change with age. Babies and young kids might not grow well, develop slowly, and get sick easily. Older kids and adults often feel very tired, have yellow skin, and a big spleen.
Severity Spectrum
Anemia in SCD can be mild or very severe. Some people have mild anemia with few symptoms. Others have severe anemia that greatly affects their life. How severe it is depends on how often they have pain crises and how much blood they lose.
| Symptom Category | Acute Symptoms | Chronic Symptoms |
| Pain | Severe pain due to vaso-occlusive crises | Ongoing pain due to chronic inflammation |
| Hemolysis | Acute hemolytic crises | Chronic hemolysis leading to anemia |
| Infections | Increased risk during acute illnesses | Ongoing risk due to splenic dysfunction |
It’s key to understand anemia symptoms in SCD to give the right care. Knowing the different symptoms and how severe they can be helps doctors tailor treatment plans for each patient.
Bone Marrow Dysfunction in Sickle Cell Disease
Sickle cell disease affects the bone marrow, leading to problems with making red blood cells. This is a big reason why people with the disease often have anemia.
Ineffective Erythropoiesis
Ineffective erythropoiesis means the bone marrow can’t make enough healthy red blood cells. In sickle cell disease, the abnormal hemoglobin S (HbS) causes problems. It makes red blood cell precursors die early or get destroyed.
Key factors contributing to ineffective erythropoiesis include:
- Abnormal hemoglobin polymerization
- Increased oxidative stress
- Enhanced inflammation within the bone marrow
These issues lead to fewer healthy red blood cells. This makes anemia worse.
Aplastic Crisis
An aplastic crisis is when the bone marrow stops making red blood cells. In sickle cell disease, infections like parvovirus B19 can cause this. It stops the bone marrow from making blood.
“Aplastic crisis in sickle cell disease patients can lead to severe anemia, necessitating immediate medical intervention, often in the form of blood transfusions.”
Managing an aplastic crisis includes blood transfusions. This helps until the bone marrow starts working again.
Bone Marrow Infarction
Bone marrow infarction is when bone marrow cells die because of bad blood flow. In sickle cell disease, vaso-occlusive crises can cause this. It makes it harder for the bone marrow to make blood cells.
The consequences of bone marrow infarction include chronic pain and further impairment of hematopoiesis.
In conclusion, sickle cell disease affects the bone marrow in many ways. It causes problems with making red blood cells, stops the bone marrow from working, and leads to cell death. Understanding these issues is key to managing the disease.
Vaso-Occlusive Events and Their Relationship to Anemia
Vaso-occlusion is a key part of sickle cell disease. It makes anemia worse in several ways. When sickled red blood cells block blood vessels, it causes pain and tissue damage.
This blockage not only causes immediate pain but also makes anemia more severe.
Mechanism of Vaso-Occlusion
The process of vaso-occlusion starts with hemoglobin S polymerizing in red blood cells. This makes them sickle-shaped. These cells then stick to blood vessel walls, blocking them.
Things like dehydration, infections, and stress can start this process.
Red blood cells can sometimes go back to normal shape. But, repeated sickling causes permanent damage. This makes vaso-occlusion worse.
How Vaso-Occlusion Worsens Anemia
Vaso-occlusion shortens the life of red blood cells and increases their destruction. Sickled cells block blood vessels, leading to tissue not getting enough oxygen. This can make the body try to make more red blood cells.
But, it’s often not enough to keep up with the loss of red blood cells.
Also, vaso-occlusive events can trap red blood cells in the spleen. This reduces the number of red blood cells in the blood, making anemia worse.
Vicious Cycle of Anemia and Vaso-Occlusion
Anemia and vaso-occlusion are in a cycle. Anemia means less oxygen for tissues, which can cause vaso-occlusive events. Then, vaso-occlusion makes anemia worse by destroying more red blood cells.
It’s important to break this cycle to manage sickle cell disease well.
Understanding how vaso-occlusive events and anemia are connected is key. It helps in finding better treatments for sickle cell disease.
Other Factors Contributing to Anemia in Sickle Cell Disease
Many factors beyond the main causes make anemia worse in Sickle Cell Disease (SCD). It’s key to know these factors for better care.
Iron Deficiency
Iron deficiency is a big problem for SCD patients. Even with lots of blood loss, some might not get enough iron. This can happen if they don’t eat enough iron or lose blood often.
Table 1: Factors Contributing to Iron Deficiency in SCD
| Factor | Description |
| Poor Dietary Intake | Inadequate iron intake due to dietary restrictions or preferences. |
| Chronic Blood Loss | Ongoing blood loss due to various reasons such as gastrointestinal ulcers. |
| Menstrual Blood Loss | Regular menstrual blood loss in females contributing to iron deficiency. |
Folate Deficiency
Folate is very important for making new blood cells. SCD patients might not have enough folate because they use more of it.
“Folate supplementation is often recommended for patients with SCD to prevent deficiency.”
Coexisting Conditions
Having other health issues can make managing anemia harder in SCD. For example, chronic kidney disease can lower the body’s ability to make new blood cells, making anemia worse.
Medication Effects
Some medicines for SCD can cause anemia as a side effect. For example, hydroxyurea helps reduce pain but can also lower blood cell counts, leading to anemia.
Good care for SCD means tackling all these issues to manage anemia well.
Diagnosis and Monitoring of Anemia in Sickle Cell Disease
Getting an accurate diagnosis of anemia in SCD is key. It uses many tools like lab tests and genetic analysis. Diagnosing and keeping track of anemia in Sickle Cell Disease (SCD) involves several steps. These steps include lab tests, imaging studies, and clinical checks.
Laboratory Tests
Laboratory tests are very important for diagnosing and tracking anemia in SCD. These tests include:
- Complete Blood Count (CBC) to check hemoglobin levels, hematocrit, and red blood cell indices.
- Hemoglobin electrophoresis to spot abnormal hemoglobin types.
- Reticulocyte count to see how the bone marrow is doing and how it’s responding to anemia.
- Lactate dehydrogenase (LDH) levels to check for hemolysis.
- Bilirubin levels to see how much hemolysis is happening.
Laboratory tests give vital info on how severe the anemia is and how well the bone marrow is responding.
| Laboratory Test | Purpose | Significance in SCD |
| CBC | Check hemoglobin, hematocrit, and RBC indices | See how bad the anemia is |
| Hemoglobin Electrophoresis | Find abnormal hemoglobin types | Confirm SCD diagnosis and find hemoglobin types |
| Reticulocyte Count | Look at bone marrow activity | Check how the bone marrow is handling anemia |
Imaging Studies
Imaging studies help check for problems linked to SCD and anemia. For example, they look for splenic sequestration or organ damage from chronic hemolysis. Common imaging methods include:
- Ultrasound to check splenic size and find sequestration.
- MRI to see organ damage and iron overload.
Genetic Testing
Genetic testing can confirm SCD by finding the genetic mutation that causes it. It’s very useful for prenatal testing and finding carriers.
Monitoring Disease Progression
Keeping a close eye on patients with SCD is key to managing anemia well and avoiding problems. This includes:
- Regular CBC and reticulocyte counts.
- Checking organ function often.
- Watching for signs of splenic sequestration or other sudden problems.
Good monitoring lets healthcare providers adjust treatment plans, which helps patients do better.
Treatment Approaches for Sickle Cell Anemia
The treatment for Sickle Cell Disease is changing fast. Many new ways to help patients are being tested. Sickle Cell Anemia needs a mix of treatments to handle its many symptoms.
Hydroxyurea Therapy
Hydroxyurea is a key treatment for Sickle Cell Disease. It helps lower the number of painful episodes and might cut down on blood transfusions. It has been shown to improve life quality for SCD patients in studies.
- Reduces frequency of painful crises
- May decrease the need for blood transfusions
- Improves quality of life for SCD patients
Blood Transfusions
Blood transfusions are vital for Sickle Cell Disease, mainly for those with severe anemia or sudden problems. Regular transfusions can lower the risk of serious issues by reducing sickled red blood cells.
- Reduces risk of stroke and other acute complications
- Improves oxygen delivery to tissues
- Can be used to manage severe anemia
Stem Cell Transplantation
Stem cell transplantation could be a cure for Sickle Cell Disease. This method replaces the patient’s bone marrow with healthy stem cells, often from a donor. Though it’s a cure, it’s risky and used only for severe cases.
Gene Therapy and Emerging Treatments
Gene therapy is a new hope for Sickle Cell Disease. It aims to fix the genetic problem causing the disease. Other new treatments, like CRISPR/Cas9, are also being looked at to fix the SCD mutation.
- Potential to cure SCD by correcting the genetic cause
- Gene-editing technologies like CRISPR/Cas9 are being researched
- Offers hope for future treatment options
Conclusion
Anemia in Sickle Cell Disease (SCD) is a complex issue. It comes from hemolysis and bone marrow problems. Knowing these causes is key to managing the disease well.
Looking at SCD causes and treatments, we see several options. These include hydroxyurea therapy, blood transfusions, and gene therapy. These aim to lessen pain and anemia severity.
To wrap up, treating anemia in SCD needs a broad approach. New research and treatments bring hope to those with SCD. They show progress in managing this condition.
FAQ
What is sickle cell disease?
Sickle cell disease is a genetic disorder that affects how the body makes hemoglobin. This leads to anemia and other health problems.
What causes anemia in sickle cell disease?
Anemia in sickle cell disease comes from several causes. These include the destruction of red blood cells, less production, and being trapped in the spleen.
What is the difference between sickle cell trait and sickle cell disease?
Sickle cell trait and sickle cell disease are different. Sickle cell trait means having one normal and one mutated gene. Sickle cell disease means having two mutated genes.
How does hemoglobin S differ from normal hemoglobin?
Hemoglobin S is an abnormal form of hemoglobin. It changes shape under low oxygen, causing red blood cells to sickle.
What are the symptoms of sickle cell anemia?
Symptoms of sickle cell anemia vary. They can range from sudden, severe pain to ongoing anemia.
What is the role of hydroxyurea in treating sickle cell disease?
Hydroxyurea is a treatment for sickle cell disease. It helps reduce painful crises and may lessen anemia’s severity.
Can gene therapy be used to treat sickle cell disease?
Gene therapy is being explored for sickle cell disease. It aims to fix the genetic mutation causing the condition.
How is anemia in sickle cell disease diagnosed?
Diagnosing anemia in SCD involves lab tests and clinical assessments. This ensures accurate diagnosis and monitoring.
What are the consequences of chronic hemolysis in sickle cell disease?
Chronic hemolysis in SCD can cause jaundice, gallstones, and a higher risk of infections.
How do vaso-occlusive events relate to anemia in sickle cell disease?
Vaso-occlusive events can make anemia worse. They reduce blood flow and increase red blood cell destruction.
Are there any nutritional deficiencies that can contribute to anemia in SCD?
Yes, iron and folate deficiencies can contribute to anemia in SCD. These are nutritional deficiencies.
What is the significance of bone marrow dysfunction in SCD?
Bone marrow dysfunction in SCD can lead to ineffective erythropoiesis and aplastic crisis. It can also cause bone marrow infarction, making anemia worse.
Reference
- Kato, G. J., Piel, F. B., Reid, C. D., Gaston, M. H., Ohene-Frempong, K., Krishnamurti, L., … & Vichinsky, E. P. (2018). Sickle cell disease. Nature Reviews Disease Primers, 4(1), 18010. https://pubmed.ncbi.nlm.nih.gov/29643497
- Ware, R. E., de Montalembert, M., Tshilolo, L., & Abboud, M. R. (2017). Sickle cell disease. The Lancet, 390(10091), 311“323. https://pubmed.ncbi.nlm.nih.gov/28159390
- Rees, D. C., Williams, T. N., & Gladwin, M. T. (2010). Sickle-cell disease. The Lancet, 376(9757), 2018“2031. https://pubmed.ncbi.nlm.nih.gov/21131035




































