Last Updated on November 20, 2025 by Ugurkan Demir

Learning about the genetics of sickle cell disease is key for families. At Liv Hospital, we focus on top-notch patient care and reliable advice. This helps patients understand their genetic health better.
Sickle cell disease is inherited in an autosomal recessive way. This means you need two mutated HBB genes, one from each parent, to have the disease. Carriers, with one mutated and one normal gene, are called sickle cell trait carriers. They usually don’t show symptoms but can pass the gene to their kids.
The HBB gene mutation causes abnormal hemoglobin, leading to sickle-shaped red blood cells. These cells stick together. We’ll dive into the genetic reasons behind sickle cell disease, including how it’s passed down and the risks it carries.
Key Takeaways
- Sickle cell disease is caused by a mutation in the HBB gene.
- The condition follows an autosomal recessive inheritance pattern.
- Carriers of the sickle cell trait typically do not show symptoms.
- Understanding the genetic underpinnings is key to managing the disease.
- Liv Hospital offers full care for patients with genetic conditions.
Understanding Sickle Cell Disease: A Genetic Overview
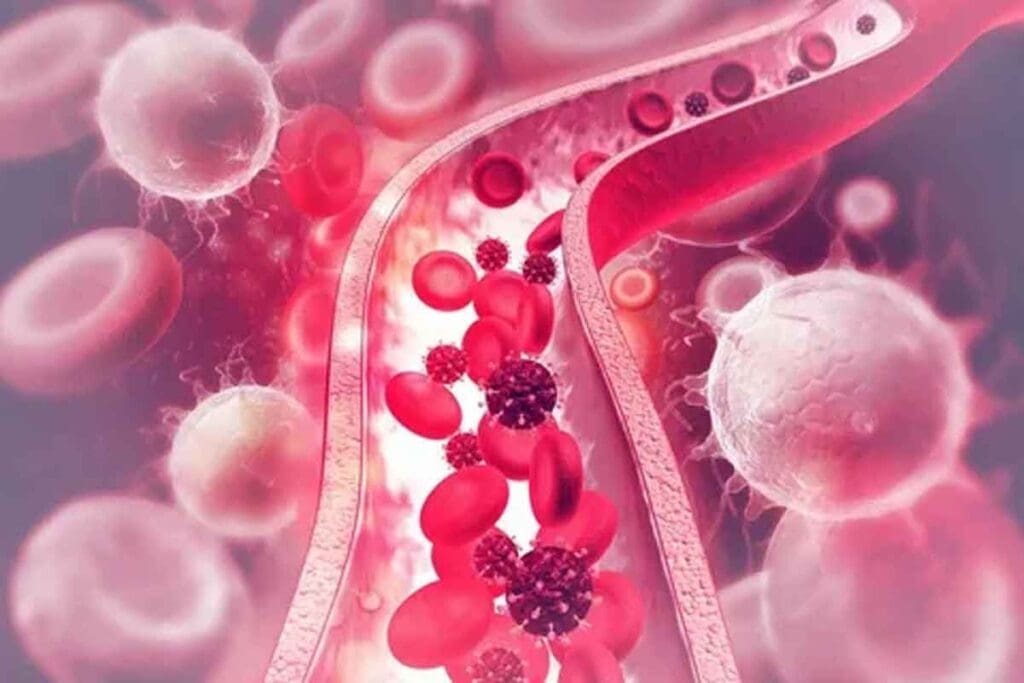
Sickle cell disease is a group of inherited blood disorders. It comes from a mutation in the HBB gene on chromosome 11. This mutation causes red blood cells to become sickle-shaped.
What is Sickle Cell Disease?
Sickle cell disease is inherited in an autosomal recessive pattern. It changes the hemoglobin in red blood cells, causing health problems. People with the disease often have pain, anemia and are more likely to get infections.
Key characteristics of sickle cell disease include:
- Abnormal hemoglobin production
- Sickle-shaped red blood cells
- Autosomal recessive inheritance
- Risk of pain episodes and infections
The Global Prevalence and Impact
Sickle cell disease is a big health problem worldwide, mainly in tropical and subtropical areas. The World Health Organization says it affects millions, mostly in Africa, the Mediterranean, and parts of India.
| Region | Prevalence |
| Africa | High |
| Mediterranean | Moderate |
| India | Moderate to High |
“Sickle cell disease is a major public health problem in many parts of the world, requiring extensive management strategies to improve the quality of life for those affected.”
Monogenic Nature of Sickle Cell Disease
Sickle cell disease is caused by a mutation in the HBB gene. This makes it a monogenic disorder. The mutation changes glutamic acid to valine at the sixth position of the beta-globin chain, creating sickle hemoglobin (HbS).
Understanding the genetic basis of sickle cell disease is key to developing tests and treatments. Genetic counseling is also vital for families with a history of the disease.
The Sickle Cell Inheritance Pattern Explained

Sickle cell disease is passed down in an autosomal recessive pattern. This means a person needs two mutated genes, one from each parent, to have the disease. Knowing this helps us understand how it spreads in families.
Autosomal Recessive Inheritance
The disease-causing gene is on a non-sex chromosome. A person with one mutated and one normal gene is a carrier. They usually don’t show symptoms but can pass the mutated gene to their kids.
If both parents are carriers, there’s a 25% chance their child will have the disease. There’s a 50% chance the child will be a carrier. And a 25% chance the child will have no mutated genes.
For more detailed information on sickle cell disease, visit MedlinePlus.
Patterns of Transmission in Families
The way sickle cell disease is passed down in families is predictable. When both parents are carriers, the risk of a child having the disease is high. Knowing this helps families prepare for the possibility of having a child with the disease.
Punnett Square Analysis of Sickle Cell Inheritance
A Punnett square is a tool that shows the chances of different genotypes in offspring. It’s useful for sickle cell disease when both parents are carriers. It helps predict the likelihood of a child inheriting the disease or being a carrier.
| Mother/Father | HbA | HbS |
| HbA | AA | AS |
| HbS | AS | SS |
In this table, “HbA” is the normal hemoglobin gene, and “HbS” is the sickle cell gene. “AA” is normal, “AS” is a carrier, and “SS” has sickle cell disease.
“Understanding the genetic basis of sickle cell disease is essential for providing appropriate care and support to affected families.” – Expert in Genetic Disorders
By looking at the inheritance pattern and using Punnett squares, families can understand their risks better. This helps them make informed health decisions.
The HBB Gene and Chromosome 11
The HBB gene is on chromosome 11. It’s key for making normal hemoglobin. Mutations here can cause sickle cell disease.
Location and Function of the Beta-Globin Gene
The HBB gene is on the short arm of chromosome 11 (11p15.4). It makes the beta-globin part of hemoglobin. This protein carries oxygen in red blood cells.
Mutations in the HBB gene can cause sickle cell disease. These changes make hemoglobin S, which deforms red blood cells.
The Role of Chromosome 11 in Sickle Cell Disease
Chromosome 11 is key for sickle cell disease because it has the HBB gene. The integrity of this gene is vital for normal hemoglobin. Any change can lead to sickle cell disease or trait.
Sickle cell disease follows an autosomal recessive pattern. This means you need two mutated HBB genes to have the disease. Carriers have one normal and one mutated gene and can pass the mutated gene to their kids.
Genetic Mapping of Sickle Cell Chromosomes
Genetic mapping finds genes on chromosomes and their connections. For sickle cell disease, it’s helped pinpoint the HBB gene on chromosome 11. It shows the mutations that cause the disease.
Researchers have mapped disease-causing mutations on chromosome 11. This info is key for genetic counseling and understanding the disease’s molecular basis.
The Molecular Basis: What Mutation Causes Sickle Cell Disease
The Glu6Val substitution is the main cause of sickle cell disease. It happens in the HBB gene, which makes the beta-globin part of hemoglobin. We’ll see how this mutation leads to abnormal hemoglobin, known as hemoglobin S, and its effects.
The Glu6Val Substitution
The Glu6Val substitution is a change where glutamic acid (Glu) is swapped with valine (Val) at the sixth spot of the beta-globin chain. This swap comes from a single nucleotide change (GAG to GTG) in the HBB gene. This mutation is the main reason for sickle cell disease, making hemoglobin S (HbS).
How the Mutation Alters Hemoglobin Structure
The change from glutamic acid to valine at the sixth spot of the beta-globin chain changes hemoglobin’s structure and function. When oxygen levels are low, hemoglobin S forms polymers. This makes red blood cells bend into a sickle shape.
This bending is because of the hydrophobic interactions between the valine residues. These interactions happen because the valine is exposed on the hemoglobin molecule’s surface.
“The polymerization of hemoglobin S is a critical event in the pathophysiology of sickle cell disease, leading to vaso-occlusive crises and other complications.”
Molecular Consequences of the Sickle Cell Mutation
The Glu6Val substitution has big effects. The polymerization of hemoglobin S makes red blood cells sickle. This also leads to:
- Red blood cells can’t bend well, getting stuck in small blood vessels.
- These sickled cells are fragile, leading to more hemolysis.
- Vaso-occlusive crises happen when blood vessels get blocked by sickled cells.
| Molecular Change | Effect on Red Blood Cells | Clinical Consequence |
| Glu6Val substitution | Polymerization of hemoglobin S | Sickling of red blood cells |
| Polymerization under low oxygen | Reduced deformability | Vaso-occlusive crises |
| Increased fragility | Hemolysis | Anemia |
Understanding sickle cell disease’s molecular basis is key for new treatments. By focusing on the Glu6Val substitution and its impact on hemoglobin, we can tackle this genetic disorder’s complexities.
Heterozygous vs. Homozygous Sickle Cell Conditions
Sickle cell disease shows up differently in people who are heterozygous or homozygous for the sickle cell gene. Knowing this helps us understand how the disease affects health in different ways.
Sickle Cell Trait: The Carrier State
People who carry the sickle cell gene but aren’t homozygous are called carriers. They have sickle cell trait. They usually don’t show symptoms but can pass the gene to their kids. Carriers might feel some effects, like pain, when they’re very active or at high altitudes.
Homozygous Sickle Cell Disease: Full Clinical Manifestation
Those with two sickle cell genes face serious health issues. They deal with chronic anemia, pain episodes, and a higher chance of infections. Over time, they might also face organ damage. The severity can vary, but they need constant medical care.
Compound Heterozygous States with Other Hemoglobinopathies
Some people have one sickle cell gene and another, like hemoglobin C or beta-thalassemia. This mix can lead to different health outcomes. For example, sickle-hemoglobin C disease might be less severe than homozygous sickle cell. But sickle-beta-thalassemia can be quite variable.
It’s key to understand these genetic mixes to give the right care and advice to those affected and their families.
Evolutionary Genetics and Population Distribution
The spread of sickle cell disease is tied to the fight against malaria. This battle has shaped the genes of people in malaria-prone areas.
Malaria Protection and Selective Advantage
The sickle cell trait helps protect against malaria. This has given people with the trait an edge in places where malaria is common. They are less likely to get severe malaria, which helps them live longer and have more children.
This advantage is strongest in those who have one normal and one sickle cell gene. They are called carriers. Studies show that these carriers have fewer malaria parasites and are less likely to die from it https://pmc.ncbi.nlm.nih.gov/articles/PMC8117455/.
Geographic Distribution of Sickle Cell Genetics
The spread of sickle cell disease follows malaria’s path. Where malaria was a big problem, the sickle cell trait is more common. This is true in sub-Saharan Africa, the Mediterranean, and parts of India.
Population Genetics and Founder Effects
Population genetics helps us understand sickle cell disease. The spread of the sickle cell gene can be changed by many things. For example, genetic drift and gene flow can play a part.
In some places, the sickle cell gene became more common because of founder effects. This happens when a small group with the gene starts a new population. This increases the gene’s frequency.
Knowing how sickle cell disease spreads is key to helping people. By studying its genetics, we can predict where it will be more common. This helps us plan better ways to manage it.
Genetic Testing and Diagnosis
Early diagnosis of sickle cell disease through genetic testing is key. It helps in providing the right care and management. Identifying sickle cell disease or the trait early in life is vital for effective management.
Prenatal and Newborn Screening
Prenatal and newborn screening programs are vital for early detection of sickle cell disease. They allow healthcare providers to offer timely support to families. Prenatal screening tests pregnant women to see if their fetus might have sickle cell disease. Newborn screening tests babies soon after birth.
Prenatal screening helps families make informed choices about their pregnancy. Newborn screening leads to early treatment, improving outcomes for affected children.
Blood Screening Techniques for Sickle Cell Anemia
Blood screening techniques are essential for diagnosing sickle cell anemia. The most common method is the sickle cell test, which finds hemoglobin S. Other methods include hemoglobin electrophoresis and high-performance liquid chromatography (HPLC), which identify different hemoglobins.
Modern Genetic Testing Approaches
Modern genetic testing has changed how we diagnose sickle cell disease. Techniques like polymerase chain reaction (PCR) and next-generation sequencing (NGS) pinpoint genetic mutations. These methods give detailed genetic info, helping in diagnosis, counseling, and planning.
We use these advanced genetic testing methods for accurate diagnosis. They support families dealing with sickle cell disease.
Hereditary Risks and Family Planning
For families with sickle cell disease, knowing about hereditary risks is vital. Sickle cell disease comes from a gene mutation and is passed down in a specific way. A child needs two copies of the mutated gene, one from each parent, to have the disease.
Calculating Inheritance Risk for Families
If both parents carry the sickle cell trait, each child has a 25% chance of having the disease. There’s a 50% chance the child will carry the trait like the parents. And a 25% chance the child won’t have the disease or carry the trait. Genetic counseling helps families understand these chances and plan better.
Genetic counseling is key for families with sickle cell disease history. It gives them detailed risk information and options for managing those risks. This way, families can understand the disease’s impact and explore reproductive choices.
Genetic Counseling for Affected Individuals
Genetic counseling does more than just assess risks for those with sickle cell disease. It’s a supportive space to talk about how the disease affects family planning. Counselors explain the chances of passing the disease to children and discuss reproductive technologies.
Genetic counseling also helps those who carry the sickle cell trait. It informs them about the risks of passing the trait or disease to their kids.
Reproductive Options for Carriers
Carriers of the sickle cell trait have several options. These include:
- Prenatal testing to check if the fetus has sickle cell disease
- Preimplantation genetic diagnosis (PGD) during IVF to choose unaffected embryos
- Adoption
- Using donor eggs or sperm to lower the risk of passing the mutated gene
Each option has its own considerations, like ethical, emotional, and financial aspects. Genetic counseling helps carriers and affected individuals make these complex decisions.
Understanding hereditary risks and the options available helps families make informed choices. We stress the need for thorough genetic counseling and support for families with sickle cell disease.
Conclusion: Advances in Understanding and Managing Sickle Cell Inheritance
Genetic understanding and management have greatly improved care for sickle cell disease patients. We now focus on the genetic causes, not just symptoms. This shift has changed how we treat the condition.
Research and new genetic testing, and therapy are key to better managing sickle cell disease. These advancements help improve patient outcomes and quality of life. Knowing how sickle cell is inherited helps us identify at-risk individuals and offer targeted care.
Genetic counseling and modern testing are now vital in managing sickle cell disease. We must keep researching and understanding genetics to improve care. Moving forward, using these advances is essential to support those with sickle cell disease fully.
FAQ
What is the genetic basis of sickle cell disease?
Sickle cell disease comes from a mutation in the HBB gene. This gene codes for a part of hemoglobin. The mutation makes abnormal hemoglobin, known as sickle hemoglobin or HbS.
How is sickle cell disease inherited?
It’s inherited in an autosomal recessive pattern. This means a person needs two copies of the mutated HBB gene to have the disease. They get one from each parent.
What is the role of the HBB gene in sickle cell disease?
The HBB gene tells our bodies how to make a part of hemoglobin. A mutation in this gene leads to sickle cell disease.
What type of mutation causes sickle cell disease?
A point mutation in the HBB gene causes it. This mutation changes glutamic acid to valine at the sixth position of beta-globin (Glu6Val).
What is the difference between being a carrier and having sickle cell disease?
Carriers have one normal and one mutated HBB gene. People with sickle cell disease have two mutated genes. Carriers usually don’t show symptoms but can pass the mutated gene to their kids.
How does the sickle cell trait protect against malaria?
The sickle cell trait helps fight malaria. The malaria parasite has trouble infecting red blood cells with sickle hemoglobin.
What are the methods used for genetic testing and diagnosis of sickle cell disease?
Tests include prenatal and newborn screenings. Blood tests and genetic tests like DNA sequencing and PCR are used to find the HBB gene mutation.
What is the importance of genetic counseling for individuals with sickle cell disease or carriers?
Genetic counseling is key. It helps people understand their risks and the risks of passing the disease to their kids. It also discusses reproductive options.
What reproductive options are available to carriers of sickle cell disease?
Carriers have many options. These include prenatal testing, preimplantation genetic diagnosis (PGD), and using donated eggs or sperm. These options help lower the chance of passing the disease to a child.
How does the geographic distribution of sickle cell disease relate to its genetics?
Sickle cell disease is more common in areas where malaria was common. The sickle cell trait protects against malaria. So, the gene is more common in these areas.
References
- Centers for Disease Control and Prevention. (2024). Sickle cell trait.
- National Heart, Lung, and Blood Institute. (2021). Sickle cell disease.