Sickle cell weight loss often stems from higher energy needs, reduced appetite during pain or illness, and nutrient gaps driven by chronic anemia and inflammation, making healthy weight maintenance difficult for many.
Many people with sickle cell disease struggle to keep a healthy weight because hypermetabolism, frequent pain crises, infections, and hospital stays can lower intake while raising calorie and protein needs. Malnutrition and anemia intensify this by diverting nutrients toward constant red blood cell production, limiting resources for growth and muscle maintenance. Practical help includes small, frequent, calorie- and protein-dense meals, correcting deficiencies like vitamin D and folate, and coordinated care with hematology and nutrition to align diet with treatments and recovery goals.
Key Takeaways
- Understanding the link between sickle cell disease and weight loss.
- The role of malnutrition in sickle cell disease.
- How anemia affects overall health and weight.
- Strategies for maintaining a healthy weight with sickle cell disease.
- The importance of complete care for patients with sickle cell disease.
The Nature of Sickle Cell Disease
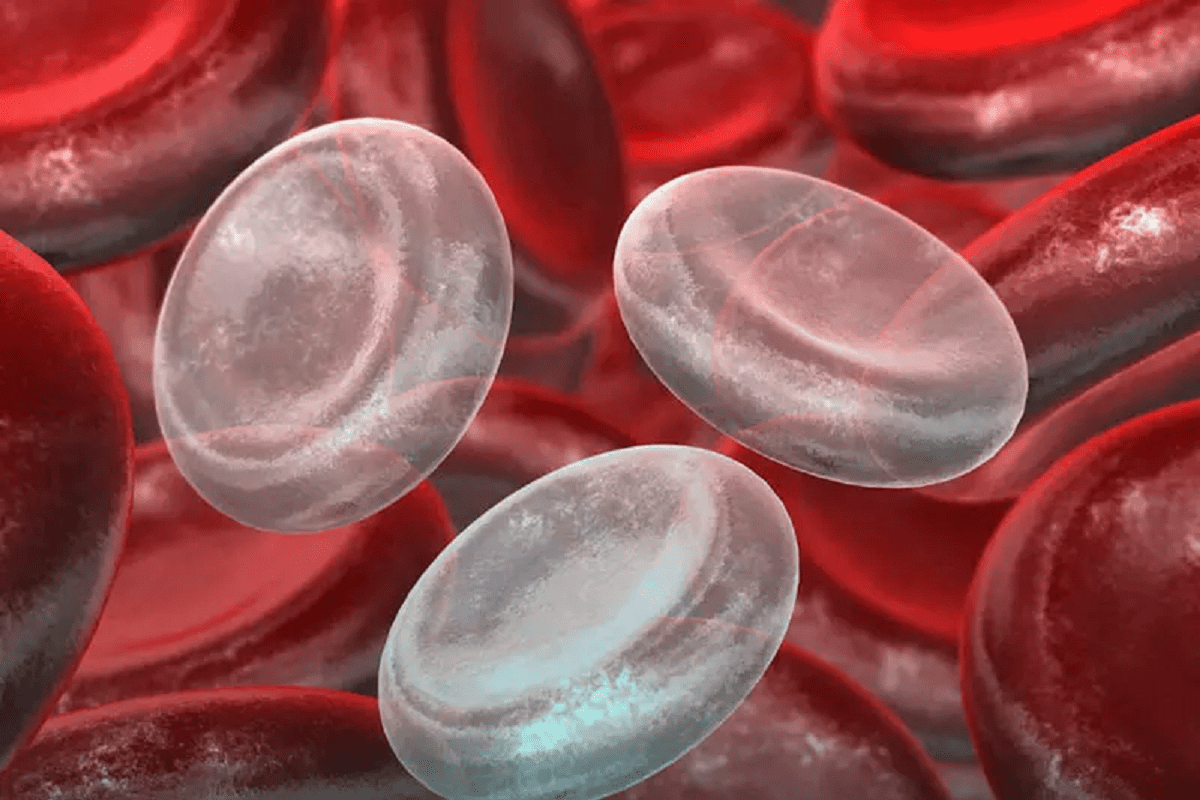
Sickle cell disease is a genetic disorder that affects how red blood cells carry oxygen. It changes the production of hemoglobin, a key protein in red blood cells.
Abnormal Hemoglobin and Red Blood Cell Formation
This disease causes red blood cells to become sickle-shaped, mainly when oxygen levels are low. This shape leads to early destruction of red blood cells. It also causes them to get stuck in small blood vessels, leading to health problems.
Prevalence and Demographics in the United States
Sickle cell disease is more common in people of African, Caribbean, and Middle Eastern descent. In the U.S., it affects about 100,000 people, mostly African Americans.
Types of Sickle Cell Disease
There are several types, with HbSS being the most common. It happens when someone gets two sickle cell genes, one from each parent. Other types include HbSC disease and HbS beta-thalassemia.
Common Body Composition Patterns
People with sickle cell disease often have lower body mass index (BMI) than others. This is due to chronic inflammation, higher energy use, and poor nutrition.
Statistical Evidence of Lower BMI
Research shows that those with sickle cell disease have lower BMI than healthy people. A study in the Journal of Pediatric Hematology/Oncology found children with the disease had much lower BMI z-scores than healthy kids.
| Population | Average BMI |
| Children with Sickle Cell Disease | 16.5 |
| Healthy Children | 18.2 |
Differences Between Children and Adults
The disease affects body composition differently in children and adults. Kids may have growth delays and lower BMI. Adults might face muscle wasting and decreased physical function.
Sickle cell disease is complex, affecting health and body composition in many ways. Understanding these impacts is key to proper care and support.
Sickle Cell Weight Loss: Primary Mechanisms

The complex interplay of increased energy expenditure and reduced energy intake leads to weight loss in sickle cell patients. It’s key to grasp these mechanisms to create effective management plans.
Increased Energy Expenditure
Patients with sickle cell disease often burn more energy. This is due to several reasons. Chronic inflammation, frequent infections, and the energy needed for red blood cell production are among them.
Key factors contributing to increased energy expenditure:
- Chronic inflammation
- Frequent infections
- Increased red blood cell turnover
- Organ damage
The basal metabolic rate (BMR) in sickle cell patients is often higher than in healthy people. This higher BMR contributes to weight loss.
| Group | Basal Metabolic Rate (BMR) |
| Sickle Cell Patients | 1,800 kcal/day |
| Healthy Individuals | 1,500 kcal/day |
Reduced Energy Intake
Reduced energy intake also plays a big role in weight loss for sickle cell patients. This decrease can stem from several factors. Decreased appetite, gastrointestinal issues, and challenges in consuming enough calories are among them.
Factors affecting energy intake:
- Decreased appetite due to chronic illness
- Gastrointestinal complications
- Dental problems
- Nutritional deficiencies
It’s vital to tackle both increased energy expenditure and reduced energy intake to manage weight loss in sickle cell disease patients. Understanding these primary mechanisms helps healthcare providers create targeted nutritional interventions. This can significantly improve patient outcomes.
Hypermetabolism in Sickle Cell Disease
Hypermetabolism in sickle cell disease affects how much energy patients use. It makes their metabolic rate go up, meaning they burn more energy.
Elevated Basal Metabolic Rate
The basal metabolic rate (BMR) is how much energy we use when we’re not moving. People with sickle cell disease often have a higher BMR. This is because their body is working harder to fight the disease.
This higher BMR is a big reason why these patients might lose weight and have nutritional problems.
Increased Oxygen Consumption
Patients with sickle cell disease also use more oxygen. Their body needs more oxygen to keep up with its fast metabolism. This can make them feel tired and can cause other health issues.
Energy Requirements During Crisis vs. Steady State
The energy needs of sickle cell disease patients change a lot. During a crisis, their body needs a lot more energy because of the inflammation and other changes. But when they’re not in a crisis, their energy needs are higher than normal but not as high as during a crisis. Knowing these different energy needs helps doctors give better nutrition advice.
Understanding the hypermetabolic state in sickle cell disease helps doctors create better nutrition plans. This supports patients’ health and well-being.
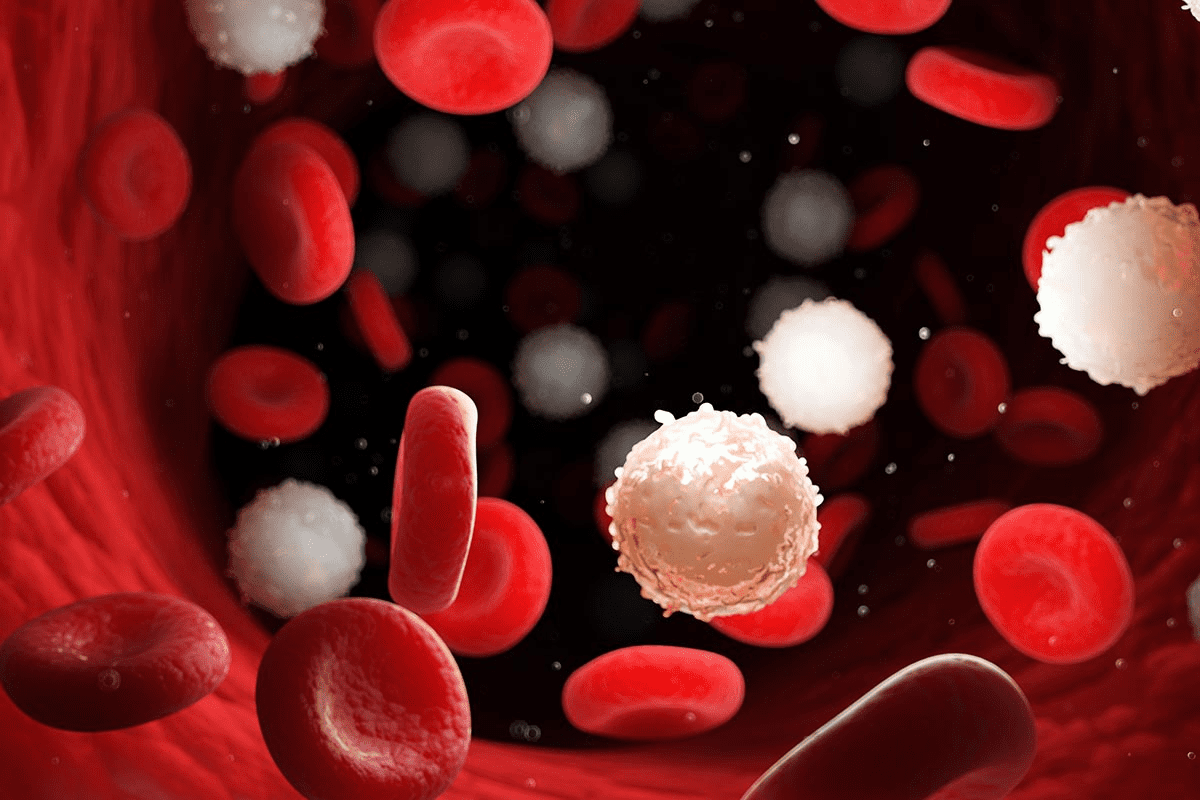
Chronic Inflammation and Cytokine Effects
Chronic inflammation is a big problem in sickle cell disease. It causes many issues that make life harder for patients. This inflammation is linked to high levels of pro-inflammatory cytokines.
Inflammatory Markers
SCD patients often have high levels of C-reactive protein (CRP). This shows they are fighting inflammation. High CRP levels can also mean their complications are worse.
Effects on Appetite Regulation
Chronic inflammation messes with how well patients eat. It makes them want to eat less. This is because pro-inflammatory cytokines lower appetite and change how the body uses food.
Cytokine-Induced Cachexia
Cytokines are key in causing cachexia. This is a condition of losing weight, muscle, and feeling tired. Chronic inflammation can lead to cachexia, making it harder to manage the disease.
Nutritional Deficiencies and Malnutrition
Sickle cell disease patients face many nutritional challenges. These challenges need careful management. The disease leads to various nutritional deficiencies, affecting their health and life quality.
Common Micronutrient Deficiencies
People with sickle cell disease often lack essential nutrients. This is due to several reasons. These include higher nutrient use, poor diet, and more nutrient loss because of the disease.
Some common nutrient gaps include:
- Vitamin D deficiency: important for bone health
- Zinc deficiency: key for immune function and healing
- Folate deficiency: vital for avoiding anemia
- Vitamin B6 deficiency: needed for many body functions
Protein-Energy Malnutrition
Protein-energy malnutrition (PEM) is a big worry for sickle cell disease patients. PEM happens when the body gets too few calories and protein. This results in weight loss and muscle wasting. The disease’s high energy use makes this worse.
| Condition | Impact on Nutrition | Consequences |
| Sickle Cell Disease | Increased energy expenditure, inadequate dietary intake | Protein-energy malnutrition, weight loss, muscle wasting |
| Chronic Inflammation | Altered metabolism, increased nutrient requirements | Malnutrition, impaired growth and development |
Impact on Growth and Development
Nutritional gaps and malnutrition deeply affect children with sickle cell disease. Good nutrition is key for normal growth and preventing disease complications.
Malnutrition can cause:
- Delayed growth and puberty
- Impaired cognitive development
- Increased susceptibility to infections
It’s vital to ensure sickle cell disease patients get the right nutrition. This helps manage their condition and improves their life quality.
Digestive System Complications
Digestive system problems are a big worry for people with sickle cell disease. These issues come from the disease itself, like chronic hemolysis and vaso-occlusive crises. Systemic inflammation also plays a role.
Liver and Gallbladder Issues
People with sickle cell disease often face liver and gallbladder problems. The disease can cause pigment gallstones from chronic hemolysis. This leads to gallbladder issues. Liver function can also be hurt by vaso-occlusive events, causing hepatic sequestration or transfusion-related iron overload.
- Chronic hemolysis can lead to bilirubin gallstones.
- Vaso-occlusive crises can cause liver damage.
- Iron overload from frequent transfusions can affect liver function.
Intestinal Blood Flow Problems
Intestinal blood flow can be affected in sickle cell disease. This is due to vaso-occlusive crises, causing acute abdominal pain. It can also lead to serious issues like intestinal infarction. This needs quick medical help.
“The risk of intestinal complications in sickle cell disease highlights the need for careful monitoring and fast action.” –
Sickle Cell Disease Expert
Malabsorption Syndromes
Malabsorption can happen due to intestinal damage from vaso-occlusive events. This can cause a lack of important nutrients. It makes managing sickle cell disease even harder.
- Regularly check nutritional status.
- Give the right nutritional supplements.
- Watch for signs of malabsorption.
Understanding these digestive system problems helps healthcare providers manage sickle cell disease better.
Pain Crisis and Reduced Food Intake
Pain crises are a big problem in sickle cell disease. They cause a lot of pain and make daily life hard. When a patient has a pain crisis, they often can’t eat well.
Acute Pain Episodes and Appetite
Acute pain episodes make it hard for patients to want to eat. The pain and nausea make food unappealing. This can lead to nutritional problems if not handled right.
Chronic Pain Management
Managing chronic pain is key for sickle cell disease patients. They use medicine, change their lifestyle, and try other therapies. These steps help lessen pain crises.
Medication Side Effects on Nutrition
Medicines for pain can affect nutrition. Some cause nausea or constipation. This makes it harder for patients to get the nutrients they need.
Growth Delays in Children with Sickle Cell
Sickle cell disease can greatly affect a child’s growth and development. It impacts physical growth, puberty, and more. Healthcare providers are very concerned about this.
Pediatric Growth Patterns and Milestones
Children with sickle cell disease often grow slower than their peers. They may gain height and weight more slowly. It’s important to watch their growth closely.
A study found a link between sickle cell disease and growth failure. This can lead to more health problems and even death.
“Growth failure in children with sickle cell disease is a multifactorial issue that requires a complete management plan.”
| Age Group | Average Height (cm) | Average Weight (kg) |
| 5-7 years | 115-120 | 18-22 |
| 8-10 years | 125-130 | 25-30 |
Puberty and Hormonal Impacts
Puberty can be tough for kids with sickle cell disease. Hormonal changes can make health problems worse. Delayed puberty is common.
Delayed puberty can hurt a child’s self-esteem and social life. Healthcare providers must help with these issues as part of their care plan.
- Watch growth and development closely
- Fix nutritional problems
- Offer psychological support
Long-term Developmental Consequences
Growth delays in children with sickle cell disease can have lasting effects. These effects can affect their health and quality of life. It’s important to understand these effects to manage the disease well.
As kids grow into adults, their healthcare needs change. It’s key to make sure they get the right care during this time. This helps reduce the long-term effects of sickle cell disease on their growth and development.
Muscle Wasting and Physical Deconditioning
Sickle cell disease (SCD) leads to muscle wasting and physical deconditioning. These issues greatly affect the quality of life and health of those with SCD.
Mechanisms of Muscle Breakdown
Muscle wasting in SCD comes from chronic inflammation, oxidative stress, and poor nutrition. Chronic inflammation releases pro-inflammatory cytokines. These cytokines promote protein breakdown, leading to muscle loss.
Impact of Reduced Physical Activity
SCD’s complications, like pain crises, reduce physical activity. This inactivity causes muscle loss and weakness. It worsens the physical deconditioning seen in the disease.
Sarcopenia in Sickle Cell Disease
Sarcopenia, or muscle loss, is a big problem in SCD. It’s caused by poor nutrition, chronic inflammation, and less activity. Sarcopenia hampers physical function, raises fall risks, and lowers quality of life.
Optimal Nutrition for Sickle Cell Patients
Good nutrition is key for sickle cell patients. A balanced diet can help manage the disease’s effects. It improves life quality and overall health.
Caloric Requirements and Meal Planning
Sickle cell patients need more calories due to their condition. A diet rich in calories is recommended to support their energy. The amount needed varies by age, sex, and disease severity.
Meal planning is important to meet these needs. Focus on foods high in nutrients like lean proteins, whole grains, fruits, and veggies. Eating smaller, frequent meals can help keep energy up and prevent tiredness.
| Age Group | Recommended Daily Caloric Intake | Meal Planning Tips |
| Children (4-8 years) | 1,200-1,600 calories | Include a variety of fruits and vegetables, whole grains, and lean proteins. |
| Teenagers (9-18 years) | 1,800-2,400 calories | Focus on nutrient-dense snacks and meals, including healthy fats and proteins. |
| Adults | 2,000-2,500 calories | Emphasize whole grains, lean proteins, and a variety of colorful vegetables. |
Protein Needs and Sources
Protein is vital for muscle health in sickle cell patients. We suggest a diet rich in quality protein sources. These include lean meats, fish, eggs, dairy, and plant-based options like beans and lentils.
The protein intake varies by age and health. Generally, sickle cell patients need 1.2 to 1.5 grams of protein per kilogram of body weight daily.
- Lean Meats: Chicken, turkey, and lean beef
- Fish: Salmon, tuna, and other fatty fish rich in omega-3 fatty acids
- Plant-based: Beans, lentils, tofu, and tempeh
- Dairy: Milk, yogurt, and cheese
Hydration Strategies
Drinking enough water is essential for sickle cell patients. It helps prevent dehydration and reduces the risk of crises. We recommend drinking plenty of water all day.
Here are some hydration tips:
- Drink at least 8-10 glasses of water a day
- Drink more water in hot weather or when sick
- Avoid caffeinated and sugary drinks that can dehydrate
- Eat hydrating foods like watermelon and cucumbers
Dietary Supplements and Micronutrients
People with sickle cell disease often struggle to get enough nutrients. This can cause a lack of important vitamins and minerals. Getting enough of these is key to managing the disease and staying healthy.
Essential Vitamins for Sickle Cell Patients
Vitamins are very important for those with sickle cell disease. Recommended vitamins include Vitamin D, Vitamin B6, and Vitamin B12. These help keep red blood cells healthy, support nerve function, and boost overall health.
Mineral Supplementation Guidelines
Minerals are also essential for sickle cell patients. Important minerals include iron, zinc, and magnesium. Always talk to a doctor before starting any mineral supplements.
Benefits of Omega-3 Fatty Acids
Omega-3 fatty acids can help reduce inflammation. This may ease some symptoms of sickle cell disease. You can find them in fatty fish, flaxseeds, and walnuts.
| Nutrient | Food Sources | Benefits |
| Omega-3 fatty acids | Fatty fish, flaxseeds, walnuts | Reduces inflammation, supports heart health |
| Vitamin D | Fatty fish, fortified dairy products, sunlight exposure | Maintains bone health, immune function |
Medical Management of Weight Issues
Managing weight in sickle cell disease is key for patient health. It involves using many methods. These include checking health, nutrition plans, and sometimes special diets.
Clinical Assessment Tools
Tools for checking health are very important. They help see how well a patient is doing. These tools include:
- Measuring weight, height, and BMI
- Looking at what a patient eats
- Tests to find out if they lack certain nutrients
Healthcare providers use these tools to understand what a patient needs. Then, they can make a plan just for them.
Therapeutic Nutrition Interventions
Special nutrition plans are made for sickle cell disease patients. These plans help with weight and nutrition. They might include:
| Intervention | Description | Benefits |
| High-Calorie Diets | More calories to help gain weight | Gain weight, feel more energetic |
| Protein Supplementation | More protein for muscle strength | Stronger muscles, better health |
| Micronutrient Supplements | Supplements for important vitamins and minerals | Fix nutrient gaps, better health |
When to Consider Medical Nutrition Therapy
Medical nutrition therapy is for complex cases. It’s for patients with big nutritional needs. This includes those who are very malnourished or losing weight too fast.
By using all these methods, healthcare providers can help manage weight in sickle cell disease patients. This ensures they get the care they need.
Safe Exercise Approaches for Weight Management
For those with Sickle Cell Disease, finding the right exercise balance is essential. Exercise helps manage weight and boosts health. But, it’s important to avoid exercises that might trigger crises.
Appropriate Physical Activities
Choosing the right exercise is key for Sickle Cell Disease patients. Low-impact activities like walking, swimming, and cycling are best. They’re less likely to cause injury or trigger a crisis.
These activities improve heart health and keep muscles strong without too much strain.
Exercise Precautions and Modifications
When exercising, Sickle Cell Disease patients should take precautions. Staying hydrated is key, and avoiding extreme temperatures helps prevent dehydration and crisis risk.
Adjusting exercises based on health and feeling can also manage risks.
Building Strength Without Triggering Crisis
Building strength is important for health, but it must be done carefully. Resistance training with light weights and more reps is effective without overdoing it.
It’s also important to listen to your body. Stop if you feel pain or discomfort, as it could signal a crisis.
Psychological Support and Body Image
Living with sickle cell disease is tough, both physically and emotionally. It affects not just the body but also mental health and body image.
Coping with Physical Appearance Concerns
People with sickle cell disease may see changes in their looks. This can be due to the disease or its treatment. Coping with these changes can be hard, affecting how they feel about themselves.
Healthcare providers are key in helping. They offer psychological support that fits each person’s needs. This support can include counseling and ways to improve body image.
Mental Health Resources
It’s important for those with sickle cell disease to have access to mental health resources. Mental health professionals can provide therapy and support groups. These places are where patients can share their stories and learn from others.
- Counseling services tailored to the needs of sickle cell patients
- Support groups for patients and their families
- Educational resources to help understand and manage the condition
Family and Community Support Systems
The support from family and community is very important. A strong support system offers emotional comfort and practical help. It’s key for feeling well overall.
Families can learn a lot by getting educated about the disease. They can also connect with other families through support groups. Community resources, like online forums and local groups, provide valuable support and information.
Conclusion: Integrated Approaches to Weight Management in Sickle Cell Disease
Managing weight for those with sickle cell disease needs a mix of strategies. This includes good nutrition, lifestyle changes, and medical care. An integrated care plan helps patients get better health and a better life.
FAQ
What is sickle cell disease and how does it affect weight?
Sickle cell disease is a genetic disorder that affects hemoglobin production. This leads to abnormal red blood cells. It can cause weight loss and malnutrition due to increased energy expenditure and reduced energy intake.
Why do sickle cell patients often experience weight loss?
Sickle cell patients often lose weight because of hypermetabolism and chronic inflammation. These conditions increase energy use and lower energy intake.
What are the nutritional needs of sickle cell patients?
Sickle cell patients need a balanced diet that meets their higher caloric needs. They also require adequate protein, essential vitamins, and minerals to manage their condition.
How can sickle cell patients manage their weight?
Sickle cell patients can manage their weight by following a tailored meal plan and staying hydrated. They should also engage in safe exercise practices and work closely with their healthcare provider.
What role do dietary supplements play in managing sickle cell disease?
Dietary supplements, like vitamins and minerals, can help address nutritional deficiencies in sickle cell patients. Omega-3 fatty acids may also provide anti-inflammatory benefits.
Can exercise help with weight management in sickle cell disease?
Yes, exercise can help with weight management in sickle cell disease. It’s important to follow safe exercise practices to avoid triggering a crisis. Patients should consult their healthcare provider to develop a suitable exercise plan.
How does chronic pain affect nutrition in sickle cell disease?
Chronic pain in sickle cell disease can lead to reduced food intake. This is due to decreased appetite or difficulties in eating. Effective pain management strategies are essential to maintaining adequate nutrition.
What are the long-term developmental consequences of growth delays in children with sickle cell disease?
Growth delays in children with sickle cell disease can lead to long-term developmental consequences. This includes delayed puberty and impacts on adult height and overall health.
How can family and community support systems help sickle cell patients?
Family and community support systems play a vital role in helping sickle cell patients cope with physical appearance concerns. They help manage their condition and maintain a positive body image.
What is the importance of psychological support for sickle cell patients?
Psychological support is essential for sickle cell patients to address body image concerns and manage stress. It helps maintain mental well-being. Access to mental health resources and support systems is vital.
References
CDC “ Prevention and Treatment of Sickle Cell Disease Complications. https://www.cdc.gov/sickle-cell/about/prevention-and-treatment.html