Acute appendicitis in children is the top surgical emergency for kids worldwide. It makes up 32% of all emergency surgeries for kids.
Spot the signs of appendicitis in kids early. Our essential guide provides the best red flags to ensure your child stays safe and healthy now.
We know that pediatric appendicitis is a serious issue that needs quick action. It shows how important it is to give kids the best care when they need surgery.
Key Takeaways
- Acute appendicitis is the leading childhood surgical emergency worldwide.
- It accounts for 32% of pediatric emergency surgeries globally.
- Timely intervention is key for the best results in pediatric care.
- Pediatric appendicitis needs full support and care.
- Knowing its commonness and risks is critical for doctors.
Overview of Pediatric Surgical Emergencies
It’s vital for healthcare providers to know about pediatric surgical emergencies. These emergencies need quick diagnosis and treatment to avoid serious problems.
Pediatric surgical emergencies affect kids all over the world. They come in many forms and need a detailed approach to handle them well.
Global Prevalence and Statistics
Pediatric surgical emergencies put a big strain on healthcare systems globally. Appendicitis and trauma are among the top reasons for these emergencies. In some places, trauma makes up almost 40% of all pediatric surgeries.
A study shows how important it is to know about these emergencies. This knowledge helps improve care for kids.
|
Condition |
Global Prevalence |
|---|---|
|
Appendicitis |
Significant variation across regions |
|
Trauma |
Up to 39.8% of total pediatric surgical cases |
Most Common Categories of Emergencies
Pediatric surgical emergencies fall into several main areas. These include gastrointestinal issues like appendicitis, trauma, and other rare conditions. Knowing these categories helps doctors plan better care.
“The ability to quickly diagnose and treat pediatric surgical emergencies is critical in reducing morbidity and mortality in children.” – Expert in Pediatric Surgery
Looking into pediatric surgical emergencies, we see many factors at play. These include understanding how common they are, their types, and their effect on healthcare. This knowledge is key to better care for kids.
Acute Appendicitis: The Leading Childhood Surgical Emergency

Acute appendicitis is a big deal for kids all over the world. It’s a serious condition that needs quick medical help to avoid big problems. We’ll look at how common it is in kids, and how it affects healthcare costs.
Statistical Overview and Epidemiology
Acute appendicitis is a big reason for belly pain in kids, leading to surgery. Recent numbers show it makes up about 37.5% of all surgeries for kids’ stomach issues. This shows how big of a deal it is for kids’ health.
There are many things that affect how common appendicitis is in kids. Age, gender, and where you live play a big role. Research shows that some groups get it more than others.
- The most common time for it is in the teens.
- Boys get it a bit more than girls.
- Some places have more cases than others.
Economic Impact on Healthcare Systems
Acute appendicitis costs a lot for healthcare systems. The money spent on diagnosis, treatment, and dealing with complications adds up. Getting it right quickly helps patients and saves money.
Several things affect how much it costs. For example:
- The price of surgeries and hospital stays.
- Costs for tests and lab work.
- Money lost because of complications from late diagnosis or treatment.
Understanding these points helps us tackle the challenges of acute appendicitis. By knowing the stats, causes, and costs, we can improve care for kids.
Pathophysiology of Appendicitis in Children

It’s important to understand how appendicitis works in kids to catch it early and treat it well. Appendicitis is a serious issue where the appendix gets inflamed and blocked. If not treated quickly, it can cause big problems.
Anatomical Considerations in Pediatric Patients
In kids, the appendix is smaller and moves more than in adults. This makes appendicitis harder to spot and deal with. The appendix’s size and where it is can really vary in kids, making it tough to diagnose. Things like a retrocecal appendix can also change how symptoms show up.
Progression of Inflammation and Obstruction
Appendicitis starts with the appendix getting blocked, usually by something like a fecalith. This blockage causes bacteria to grow too much, leading to more problems. As it gets worse, inflammation and lack of blood flow can happen, which might lead to a hole in the appendix and infection if not treated.
Differences Between Adult and Pediatric Appendicitis
Kids with appendicitis are different from adults in many ways. Kids often have a higher chance of the appendix bursting because they might not get diagnosed right away. This is because their symptoms can be hard to figure out and they might not be able to say what hurts. The way kids’ immune systems work and their appendix’s shape also play a part in these differences. Knowing these differences is key to helping kids get better.
What Causes Appendicitis in Kids?
The exact reason for appendicitis in kids is not fully known. But, research has found several possible causes and risk factors. Knowing these can help spot the problem early and treat it well.
Common Triggers and Mechanisms
Appendicitis happens when the appendix gets blocked. This blockage can be caused by hardened fecal matter, too much lymphoid tissue, or other things. This blockage can lead to too many bacteria and inflammation.
Key factors that may contribute to appendicitis include:
- Infection: Bacterial or viral infections can cause lymphoid hyperplasia, leading to appendix obstruction.
- Diet: A diet low in fiber may contribute to the formation of fecaliths.
- Genetics: Family history may play a role in the predisposition to appendicitis.
Risk Factors and Predispositions
Some things can make a child more likely to get appendicitis. These include:
|
Risk Factor |
Description |
|---|---|
|
Age |
Appendicitis is more common in children over 5 years old. |
|
Family History |
A family history of appendicitis may increase the risk. |
|
Dietary Factors |
A low-fiber diet may contribute to the risk of appendicitis. |
Knowing about these risk factors and triggers helps in spotting and treating appendicitis in kids early. While we can’t always prevent it, knowing the risks helps in quick diagnosis and treatment.
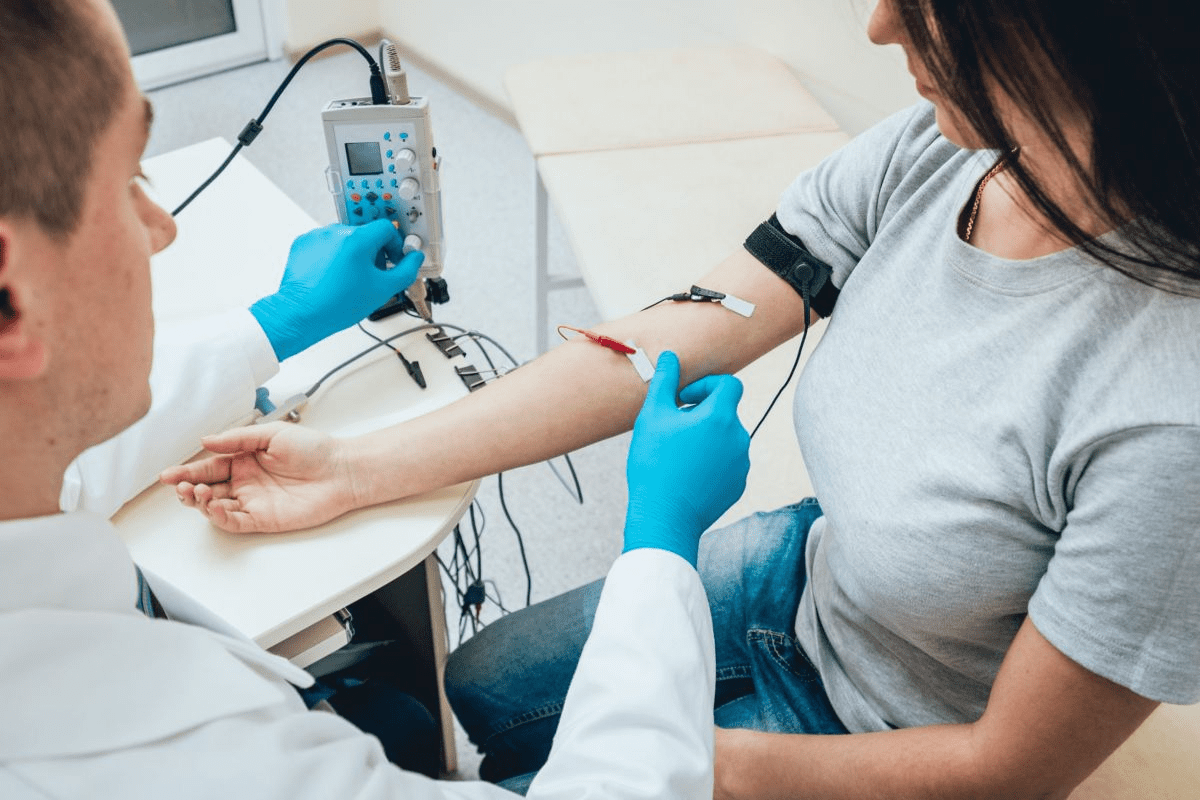
Signs of Appendicitis in Kids: Recognizing the Symptoms
<SEP-7213_image_4>
It’s important to know the signs of appendicitis in kids to get them help fast. This condition can get worse quickly. So, knowing the early signs and classic symptoms is key for parents and caregivers.
Early Warning Signs
The start of appendicitis often shows up with small symptoms. These can look like other, less serious problems. Early warning signs include:
- Abdominal pain or discomfort, first around the navel and then in the lower right abdomen
- Mild fever, usually under 101°F (38.3°C)
- Loss of appetite
- Nausea or vomiting
These symptoms can change depending on how bad they are. They might not be obvious right away. So, it’s important for caregivers to watch closely.
Classic Clinical Presentations
As appendicitis gets worse, classic clinical presentations become clearer. These include:
|
Symptom |
Description |
|---|---|
|
Abdominal Tenderness |
Tenderness in the lower right abdomen, often with muscle tension |
|
Rebound Tenderness |
Pain when pressure is released on the abdomen, showing irritation |
|
Fever |
Higher temperature, possibly over 101°F (38.3°C) as it gets worse |
These signs are important and mean you need to see a doctor right away.
Atypical Presentations in Different Age Groups
Appendicitis can show up differently in different ages. For example:
- In younger kids, symptoms might be vague, like being irritable or not wanting to walk
- In older kids and teens, symptoms can be more like those in adults, with clear pain and tenderness
Knowing these differences helps doctors diagnose appendicitis correctly in all ages.
Differential Diagnosis: Conditions Mimicking Appendicitis
When looking at appendicitis, many other conditions can look similar. These include both stomach and urinary problems. It’s key to get the right diagnosis.
When a child seems to have appendicitis, think of other reasons for their pain. Gastrointestinal conditions like inflammatory bowel disease and gastroenteritis can look like appendicitis. They all cause stomach pain, nausea, and vomiting.
Common Gastrointestinal Mimics
Finding the right diagnosis for these mimics can be tough. Here are some common ones:
- Inflammatory bowel disease: This includes Crohn’s disease and ulcerative colitis. They can cause pain and inflammation that looks like appendicitis.
- Gastroenteritis: This is an infection in the stomach and intestines. It can cause symptoms that seem like appendicitis.
- Intestinal obstruction: A blockage in the intestine can cause severe pain, nausea, and vomiting. It looks a lot like appendicitis.
Genitourinary Conditions
Some urinary problems can also seem like appendicitis. Here are a few examples:
- Urinary tract infections: These infections can cause pain and discomfort in the abdomen. It might look like appendicitis.
- Kidney stones: Stones in the kidneys or ureters can cause a lot of pain. This pain can spread to the lower abdomen.
- Ovarian torsion or rupture: In girls, ovarian problems can cause severe pain in the lower abdomen. It might be mistaken for appendicitis.
To get the right diagnosis, doctors need to do a full check-up. This includes talking to the patient, doing tests, and using imaging. By looking at all possible causes, doctors can make sure kids get the right treatment.
Diagnostic Approaches for Pediatric Appendicitis
Diagnosing appendicitis in kids needs a mix of clinical checks, lab tests, and imaging. We’ll dive into these methods to see how they help get a correct and quick diagnosis.
Clinical Evaluation and Scoring Systems
Checking a child’s health is key in finding appendicitis. It includes talking to the child and doing a physical exam. Scoring systems, like the Alvarado score, help doctors guess if it’s appendicitis based on what they find.
These scores use symptoms, signs, and lab results to sort patients by risk. But, they need to be used with care in kids because they can show different signs.
Laboratory Tests
Lab tests are important in diagnosing appendicitis. White blood cell count (WBC) and C-reactive protein (CRP) are key markers. High WBC and CRP levels suggest inflammation, but they’re not specific to appendicitis.
Other tests, like urinalysis, help rule out other pain causes, like UTIs.
Imaging Studies
Imaging is vital in diagnosing appendicitis. Ultrasound is often first because it’s safe and doesn’t use radiation. It can spot an inflamed appendix, but it depends on the skill of the person doing it.
Computed Tomography (CT) scans are very accurate but use radiation, which is a drawback for kids. Magnetic Resonance Imaging (MRI) is safe but might not be available or affordable for everyone.
Using all these methods helps doctors accurately diagnose appendicitis in kids. This leads to timely and right treatment.
When to Seek Emergency Care for Children’s Appendix Pain
If your child has appendix pain, knowing when to seek emergency care is key. Being aware of the signs can save lives. We’ll show you the important symptoms to watch for and how to talk to doctors.
Red Flag Symptoms Requiring Immediate Attention
Some symptoms mean your child needs help right away. These include:
- Severe abdominal pain that gets worse
- Vomiting, often with blood
- Fever over 101.5°F (38.6°C)
- Abdominal tenderness or guarding (muscle tension)
- Rebound tenderness (pain when pressure is released)
Spotting these symptoms early can greatly help your child. If you see any, go to the emergency room without delay.
Communicating Effectively with Healthcare Providers
When at the emergency room, clear talk with doctors is key. Be ready to share your child’s symptoms, health history, and any medicines. Here’s how to communicate well:
- Be clear about when and how long symptoms lasted
- Tell about any past similar issues or health problems
- Share all medicines, including how much and how often
- Ask about your child’s diagnosis, treatment, and future outlook
Preparing for the Emergency Room Visit
Getting ready can make the emergency room visit easier for you and your child. Here’s what to do:
|
Preparation Step |
Description |
|---|---|
|
Bring relevant documents |
Include your child’s insurance cards, identification, and any relevant medical records |
|
List medications and allergies |
Provide a complete list of your child’s medicines, dosages, and any allergies |
|
Stay calm and reassuring |
It’s important to stay calm and reassure your child that everything will be okay |
Being ready and knowing what to expect can help your child get the best care in the emergency room.
Treatment Options for Appendicitis in Children
Managing appendicitis in kids needs a special plan. This plan includes both surgery and non-surgery options. The right treatment depends on how bad the appendicitis is, the child’s health, and certain rules doctors follow.
Surgical Interventions
Removing the appendix, called an appendectomy, is a common treatment for kids. Surgery is often chosen because it stops serious problems like a burst appendix. The type of surgery depends on the doctor’s skill and the child’s health.
Pediatric Appendectomy Approaches
Doctors use different ways to do an appendectomy in kids. Laparoscopic surgery is a small cut method that uses a camera. It helps kids heal faster and feel less pain. Sometimes, an open surgery is needed if the appendix bursts or there are other issues.
Non-Operative Management
In some cases, not doing surgery is an option. This usually means using antibiotics to fight the infection. This choice is for early appendicitis without big problems. But, it’s important to watch the child closely because surgery might be needed later.
Choosing the right treatment is key. Parents and doctors need to work together. They must look at the latest research and guidelines to decide what’s best for each child.
Complications of Untreated Appendicitis
Untreated appendicitis can cause severe and dangerous problems. If the appendix bursts, it can lead to more serious health issues.
Pathophysiology of Ruptured Appendix
A ruptured appendix happens when the appendix bursts. This releases bacteria into the belly. It can cause peritonitis, an infection of the belly lining.
The appendix gets inflamed, builds up pressure, and then bursts. This is a serious emergency that needs quick help.
Acute Complications
Acute complications of untreated appendicitis include:
- Peritonitis: Infection of the abdominal lining
- Abscess formation: Pus accumulation around the appendix
- Sepsis: Blood infection that can spread to other parts of the body
|
Complication |
Description |
Treatment |
|---|---|---|
|
Peritonitis |
Infection of the abdominal lining |
Antibiotics, Surgery |
|
Abscess |
Pus accumulation around the appendix |
Drainage, Antibiotics |
|
Sepsis |
Blood infection |
Antibiotics, Supportive care |
Long-term Consequences and Morbidity
Long-term effects of untreated appendicitis can include:
- Adhesions: Scar tissue that can cause bowel obstruction
- Infertility: Damage to reproductive organs
- Chronic pain: Ongoing pain from scar tissue
It’s important to treat appendicitis quickly. This helps avoid these problems and ensures the best health outcomes.
Post-Operative Care and Recovery After Pediatric Appendectomy
The recovery after a pediatric appendectomy needs careful planning. It’s important to make sure your child gets the right care to recover well.
Hospital Recovery Protocol
Right after surgery, your child will be watched in the hospital’s recovery room. Our team will keep an eye on their health and manage pain. Most kids stay in the hospital for one to three days, based on the surgery and their health.
We want kids to start moving again soon. Early mobilization helps avoid problems and speeds up healing. We also teach parents how to care for their child at home, including managing pain and watching for infection signs.
Home Care Guidelines
At home, it’s key to follow a care plan. This means giving pain medicine as told, resting, and slowly getting back to normal. Watching for signs of complications like fever or severe pain is also important.
Eating well is important for getting better. We suggest a nutrient-rich diet like bananas, rice, applesauce, and toast (BRAT diet). Drinking lots of fluids is also key.
Care Plan for Appendicitis Recovery
A good care plan is vital for recovery. It should include check-ups with our team to see how healing is going. Keeping an eye on your child’s health and telling the doctor about any issues is also important.
By sticking to these guidelines and working with our team, you can help your child fully recover. Our aim is to give them the best care for their physical and emotional health during recovery.
Other Common Pediatric Surgical Emergencies
Pediatric surgical emergencies cover a wide range. They include traumatic and gastrointestinal issues. While appendicitis is a big worry, other emergencies need quick action to avoid serious problems.
Trauma-Related Emergencies
Trauma is a major cause of illness and death in kids. It leads to various surgical emergencies. Blunt trauma from car accidents or falls can cause spleen or liver injuries. Penetrating trauma is less common but can happen in older kids.
Handling trauma in kids needs a team effort. Pediatric surgeons, trauma experts, and others work together. They follow Advanced Trauma Life Support (ATLS) to keep the child stable and treat urgent injuries.
Gastrointestinal Emergencies
Gastrointestinal emergencies include intussusception, volvulus, and necrotizing enterocolitis (NEC). Intussusception is when part of the intestine slides into another, causing blockage and possible damage. Volvulus is when a part of the intestine twists, leading to damage if not treated fast.
Necrotizing enterocolitis mainly affects premature babies. It’s when part of the bowel dies due to lack of blood. Quick surgery is key to managing these serious conditions.
It’s vital to spot these issues early. Quick action can greatly improve a child’s chances of recovery from these emergencies.
Socioeconomic Factors Affecting Pediatric Surgical Outcomes
Socioeconomic disparities can deeply impact the results of surgeries in kids. These disparities show up in different ways, like access to healthcare and the quality of care. They also affect how quickly kids get the help they need.
Healthcare Access Disparities
Healthcare access is a big issue for kids from lower-income families. These kids often struggle to get the surgery they need on time. Reasons include not having health insurance, being far from hospitals, and not being able to afford care.
Table: Factors Contributing to Healthcare Access Disparities
|
Factor |
Description |
Impact on Pediatric Surgical Outcomes |
|---|---|---|
|
Lack of Health Insurance |
Limited or no health insurance coverage |
Delayed or foregone surgical interventions |
|
Geographical Distance |
Distance from healthcare facilities |
Increased travel time, delayed care |
|
Socioeconomic Constraints |
Financial limitations, lack of transportation |
Difficulty in accessing care, adherence to post-operative instructions |
Influence on Treatment Delays and Complications
Socioeconomic issues can cause delays in treatment, raising the risk of problems in kids’ surgeries. For example, not treating appendicitis quickly can lead to serious issues like perforation and peritonitis.
Early intervention is critical to avoid these complications. Raising awareness and educating the public about surgical emergencies is key.
Public Health Initiatives Addressing Disparities
There are many public health efforts to tackle these disparities. These include improving access to healthcare, better health insurance, and community-based programs.
For instance, programs that help pay for surgeries, improve healthcare in poor areas, and educate about health can help. These efforts aim to reduce the gap in care for all kids.
By tackling the socioeconomic factors that impact kids’ surgery outcomes, we can strive for fair healthcare for every child. This is true, no matter their background.
Prevention Strategies and Early Intervention
Teaching parents and caregivers is vital to prevent appendicitis issues in kids. Knowing the signs helps them get medical help fast. This can stop serious problems like rupture.
Education for Parents and Caregivers
It’s important to educate parents and caregivers. Early recognition of symptoms like belly pain, fever, and vomiting is key. They should watch for:
- Severe belly pain or tenderness
- Fever over 101°F (38.3°C)
- Vomiting or loss of appetite
- Abdominal swelling or tenderness
Knowing these signs can greatly help a child’s health. It’s also key to talk well with doctors. This ensures the child gets the right care.
Preventive Health Measures
Preventive steps can also help. A healthy diet full of fiber can prevent constipation linked to appendicitis. Being active also keeps the body healthy.
Some important steps include:
- Eating a balanced diet with lots of fiber
- Drinking plenty of water to avoid constipation
- Doing regular exercise
- Staying away from foods that upset the stomach
While you can’t always stop appendicitis, being healthy can lower risks. We suggest families talk to their doctors about these steps.
Advances in Pediatric Emergency Surgery
The field of pediatric emergency surgery has seen big changes. These changes come from new technologies and research. They are making care better for kids, improving their health now and in the future.
Technological Innovations
New technologies are leading the way in pediatric emergency surgery. Minimally invasive surgical techniques are becoming more common. They help kids heal faster and leave less scar tissue.
Advanced imaging technologies like 3D imaging and intraoperative MRI are also being used. They give surgeons the info they need to make better decisions during surgery.
Robotic-assisted surgery is another big step forward. It makes surgeries more precise and controlled. Studies show it’s improving results and allowing for more procedures on younger patients.
Research Directions and Future Treatments
Research is key to keeping pediatric emergency surgery moving forward. Scientists are working on personalized medicine approaches. These tailor treatments to each child’s unique needs.
There’s also a lot of focus on regenerative medicine. It aims to fix or replace damaged tissues. This could change how we treat some conditions.
In the future, artificial intelligence (AI) and machine learning will play a big role. They can analyze lots of data to predict outcomes and improve treatment plans. These advancements promise to make care even better for kids in emergency surgery.
Conclusion
Acute appendicitis is a big deal for kids, needing quick action to avoid serious problems. We’ve looked at how to handle pediatric surgical emergencies, focusing on appendicitis in young ones.
We talked about how common it is, why it happens, and how kids show symptoms. We also covered how doctors diagnose and treat it. Knowing this helps doctors and parents act fast when it’s needed.
Getting help early is the best way to deal with these emergencies. We’ve gathered important info to keep everyone informed and ready to help.
Improving care for kids in emergencies is a big goal. We need to keep learning and spreading the word. This helps doctors and parents work together better.
It’s also important to keep improving surgery for kids and finding ways to prevent these problems. We should support research and efforts to make sure all kids get the care they need.
FAQ
What are the early warning signs of appendicitis in children?
Early signs of appendicitis in kids include tummy pain, feeling sick, throwing up, not wanting to eat, and having a fever. Keep an eye on these signs. If they get worse or don’t go away, get medical help right away.
How is appendicitis diagnosed in pediatric patients?
Doctors use a few ways to figure out if a kid has appendicitis. They look at the symptoms, do lab tests, and might use imaging. They also use scores like the Alvarado score to guess if it’s appendicitis.
What are the treatment options for appendicitis in children?
Kids with appendicitis might need surgery or not. The choice depends on how bad it is and the kid’s health. We pick the best treatment for each child.
What is the recovery process like after a pediatric appendectomy?
After surgery, we follow a special plan to help kids recover well at home. We tell parents how to care for their child, including managing pain and keeping the wound clean. We also schedule follow-up visits.
Can appendicitis be prevented in children?
We can’t stop appendicitis for sure, but we teach parents and caregivers about its signs. We also encourage healthy habits like eating right and regular doctor visits.
What are the complications of untreated appendicitis?
If appendicitis isn’t treated, it can cause big problems. These include a burst appendix, abscesses, and peritonitis. We stress the need for quick diagnosis and treatment to avoid these issues.
How do socioeconomic factors affect pediatric surgical outcomes?
Money and access to healthcare can affect how well kids do after surgery. We work to make sure all kids get the care they need, no matter their background.
What advances are being made in pediatric emergency surgery?
Surgery for kids is getting better with new tech and research. We use less invasive methods and work on making surgery safer and more effective for kids.
How can parents prepare for an emergency room visit for suspected appendicitis?
Parents should know the signs of a serious problem and talk well with doctors. They should also have their child’s medical info ready.
What is the pathophysiology of a ruptured appendix?
A ruptured appendix happens when it bursts, spilling bad stuff into the belly. This can cause a big infection and serious problems.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK441864/