Last Updated on December 1, 2025 by Bilal Hasdemir
Pediatric brain tumors worry parents and doctors a lot. Every year, about 4,000 kids in the U.S. get diagnosed with primary brain tumors. This makes them the second most common cancer in kids, after leukemia.
Getting a diagnosis of a pediatric brain tumor can feel scary. These tumors can happen at any age, even when a child is just a baby. Their effect on families is huge. As we dive deeper, it’s key to know how often, what types, and how they affect childhood brain tumors.
Key Takeaways
- Pediatric brain tumors are rare but a big worry.
- Every year, about 4,000 kids in the U.S. get brain tumors.
- Brain tumors are the second most common cancer in kids.
- These tumors can happen at any age, even infancy.
- Knowing the signs and symptoms is key for early detection.
- Treatment choices depend on the tumor’s type and where it is.
Understanding Pediatric Brain Tumors
Pediatric brain tumors are abnormal growths in the brain of children. They can be either benign or malignant. These tumors are different from those in adults because they happen in developing brains.
These tumors are unique because they affect children’s developing brains. Their type and location can impact a child’s development and quality of life.
Definition and Basic Concepts
Pediatric brain tumors are classified based on their cell of origin and behavior. Common types include medulloblastoma, astrocytoma, and ependymoma. Knowing the tumor type is key for the right treatment.
The World Health Organization (WHO) classifies brain tumors. They use histological features and genetic characteristics. This helps predict the tumor’s behavior and guides treatment.
Difference Between Pediatric and Adult Brain Tumors
Pediatric brain tumors are different from adult ones. Adults often get glioblastoma, a fast-growing tumor. Children are more likely to get medulloblastoma or pilocytic astrocytoma.
The genetic mutations in pediatric brain tumors are unique. They reflect the developing brain’s biology. This is important for creating targeted therapies.
The Developing Brain and Cancer
The developing brain is more vulnerable to cancer and its treatment. Radiation therapy and chemotherapy can harm brain development. They are lifesaving but can have lasting effects.
It’s important to understand how tumors, brain development, and treatments interact. This requires a team effort from pediatric oncologists, neurosurgeons, and rehabilitation specialists. They work together to improve care and reduce long-term damage.
Prevalence and Epidemiology of Childhood Brain Tumors
Understanding childhood brain tumors is key to better treatments and outcomes. These tumors are rare but serious in kids. They deeply affect children’s lives.
Statistical Overview in the United States
In the U.S., brain tumors are a top cancer in kids. They make up about 26% of all childhood cancers. The rate is around 6 cases per 100,000 kids each year.
Key statistics include:
- About 4,300 new cases of primary brain tumors are found in kids aged 0-19 each year.
- Brain tumors are the second most common cancer in kids, after leukemia.
- Most brain tumors in kids happen before they turn 10.
Global Incidence Rates
Worldwide, childhood brain tumor rates vary a bit. But, the average is about 3-4 cases per 100,000 kids yearly.
Regional variations in rates come from differences in diagnosis, reporting, and possibly environment.
Age Distribution and Risk by Age
The risk of brain tumors changes with age in kids. Some tumors are more common in certain age groups.
- Infants and Toddlers (0-4 years): They often get medulloblastoma and ependymoma.
- School-age Children (5-9 years): They usually get astrocytomas and gliomas.
- Adolescents (10-19 years): Their tumors can be similar to those in younger kids, with some differences.
Trends in Pediatric Brain Tumor Rates
Recent studies show a slight rise in childhood brain tumors. But, it’s important to note that this might be due to better diagnosis, not more actual tumors.
Key trends include:
- Some types of tumors are being diagnosed more often, thanks to better imaging.
- Survival rates vary based on tumor type, age, and treatment.
Risk Factors for Pediatric Brain Tumors
Knowing the risk factors for pediatric brain tumors is key for early detection and prevention. The exact causes of these tumors in kids are not fully known. But, research has found several factors that might lead to their development.
Genetic Predispositions and Inherited Syndromes
Genetic predispositions are a big factor in pediatric brain tumors. Certain inherited syndromes, like Li-Fraumeni, neurofibromatosis, and tuberous sclerosis, increase a child’s risk. These syndromes come from genetic mutations that can cause tumors.
| Syndrome | Gene Mutation | Associated Risk |
| Li-Fraumeni Syndrome | TP53 | Increased risk of various cancers, including brain tumors |
| Neurofibromatosis | NF1/NF2 | Risk of developing neurofibromas and other tumors |
| Tuberous Sclerosis | TSC1/TSC2 | Risk of developing subependymal giant cell astrocytomas |
Environmental Factors
Some environmental factors might increase the risk of pediatric brain tumors. Ionizing radiation is a known risk because it can damage DNA, leading to tumors. Other exposures, like pesticides and electromagnetic fields, are being studied but their role is debated.
Prenatal and Early Life Exposures
Prenatal and early life exposures might also play a role in brain tumor risk. Maternal exposure to substances like tobacco and alcohol during pregnancy has been linked to brain tumor risk in kids. Also, infections during pregnancy and birth characteristics are being studied for their possible connection to brain tumors.
Myths vs. Facts About Causes
There are many myths about the causes of pediatric brain tumors. It’s important to separate myths from facts to provide accurate information and reduce fear. For example, there’s no strong evidence that mobile phone use causes brain tumors in kids. Knowing the facts can help families make informed decisions and reduce anxiety.
By understanding the risk factors and causes of pediatric brain tumors, we can work towards early detection and prevention. Ongoing research is key to uncovering more about these complex diseases.
Common Types of Pediatric Brain Tumors
It’s important to know about the different types of pediatric brain tumors. They are classified by the cells affected and where in the brain they are. We’ll look at the most common types, their features, symptoms, and treatment options.
Medulloblastoma
Medulloblastoma is the most common malignant brain tumor in kids. It happens in the cerebellum and grows fast. It can spread to other brain parts and the spinal cord. Symptoms include:
- Headaches and vomiting
- Unsteady gait and balance problems
- Double vision or other visual disturbances
Treatment for medulloblastoma includes surgery, chemotherapy, and radiation therapy.
Astrocytoma and Other Gliomas
Astrocytoma is a glioma that comes from astrocytes. These tumors can be low-grade (less aggressive) or high-grade (more aggressive). Symptoms vary based on the tumor’s location and grade:
- Seizures
- Headaches
- Weakness or numbness in the limbs
Treatment depends on the tumor’s grade and location. It may include surgery, chemotherapy, and radiation therapy.
Ependymoma
Ependymoma comes from ependymal cells in the ventricles and spinal cord. These tumors can happen anywhere in the ventricular system. Symptoms include:
- Headaches and nausea
- Weakness or numbness
- Difficulty with coordination and balance
Treatment usually involves surgery. Sometimes, radiation therapy is needed, based on the tumor’s grade and how much was removed.
DIPG (Diffuse Intrinsic Pontine Glioma)
DIPG is a very aggressive and malignant brainstem glioma that mainly affects kids. It starts in the pons, a part of the brainstem. It’s hard to treat because of its location. Symptoms include:
- Difficulty swallowing
- Double vision
- Weakness or paralysis of the face or limbs
Treatment options are limited, and the outlook is poor. Research is ongoing to find better treatments and improve quality of life.
In conclusion, knowing the specific type of pediatric brain tumor is key for effective treatment. Each tumor has its own characteristics, symptoms, and treatment challenges.
Signs of Brain Cancer in Infants
It’s vital to spot the early signs of brain cancer in babies. They can’t tell us how they feel. So, parents and caregivers must watch closely.
Early Warning Signs in Babies
Babies with brain tumors might show some early signs. These include:
- An unusually large head size or rapid growth
- Swelling or bulging of the soft spots on the head
- Frequent vomiting or nausea
- Seizures or convulsions
Watching for these signs is key. They can mean a serious problem.
Physical Symptoms to Watch For
Physical symptoms can differ but often include:
| Symptom | Description |
| Weakness or paralysis | Infants may show signs of weakness or paralysis in their limbs. |
| Vision changes | Abnormal eye movements or squinting can be indicative of vision problems. |
| Balance and coordination issues | As infants grow, difficulties with balance and coordination can become apparent. |
These symptoms need a doctor’s check-up right away.
Behavioral Changes
Behavioral changes can be small but are very important. These might include:
“Changes in feeding patterns, irritability, or lethargy can be indicative of neurological issues, including brain tumors.”
Parents often notice these changes first. Their observations are very important.
When to Seek Immediate Medical Attention
If an infant shows any of these signs, get help right away:
- Severe headache or vomiting
- Seizures or loss of consciousness
- Significant changes in behavior or physical condition
Early treatment can greatly help babies with brain cancer.
Brain Tumor Symptoms by Location
The location of a brain tumor greatly affects the symptoms it causes. Tumors can disrupt various brain functions, leading to different symptoms. Knowing these symptoms helps in early detection and treatment.
Cerebellar Tumor Symptoms
The cerebellum helps with movement, balance, and posture. Tumors here can lead to:
- Coordination and balance problems
- Difficulty with fine motor tasks
- Unsteady gait
- Slurred speech
Brain Stem Cancer Indicators
The brain stem manages essential functions like breathing and heart rate. Symptoms of brain stem tumors include:
- Difficulty swallowing
- Double vision
- Weakness or numbness in the face
- Respiratory problems
Frontal Lobe Tumor Signs
The frontal lobe handles decision-making and motor functions. Tumors here can cause:
- Changes in personality or behavior
- Difficulty with decision-making
- Weakness or paralysis on one side of the body
- Speech difficulties
Parietal Lobe Tumor Symptoms
The parietal lobe deals with touch and spatial awareness. Symptoms of parietal lobe tumors may include:
- Numbness or tingling sensations
- Difficulty with spatial awareness
- Problems with hand-eye coordination
- Difficulty with reading or writing
It’s key to recognize these symptoms for effective diagnosis and treatment of brain tumors. If you notice any of these symptoms, seek medical help right away.
Brain Tumor Symptoms in Children and Adolescents
It’s key for parents and doctors to know the signs of brain tumors in kids and teens. These tumors can show up in different ways in young people. This makes finding out what’s wrong harder.
Age-Specific Symptoms in Toddlers
Toddlers with brain tumors might seem cranky, throw up, or not grow well. These signs can look like other common issues. This can make it hard to figure out what’s really going on.
Warning Signs in School-Age Children
Kids in school might say they have headaches, throw up in the morning, or have trouble balancing. These problems can make it hard for them to do well in school and enjoy everyday activities.
Symptoms in Teenagers
Teenagers with brain tumors might have headaches, seizures, or act differently. They might also have trouble thinking clearly. These signs are similar to what adults might experience.
Vision Changes and Seizures as Indicators
Seeing double or blurry vision and having seizures are big warning signs. They mean a child or teen might have a brain tumor. These signs need to be checked by a doctor right away.
Parents and caregivers should know these signs. If they keep happening or get worse, it’s important to see a doctor.
| Age Group | Common Symptoms |
| Toddlers | Irritability, vomiting, failure to thrive |
| School-age Children | Headaches, morning vomiting, balance issues |
| Teenagers | Headaches, seizures, personality changes |
Diagnostic Procedures for Pediatric Brain Tumors
Diagnosing brain tumors in kids is a mix of clinical checks and advanced imaging. This process is tough but key for finding the best treatment.
Initial Assessment and Physical Examination
The first step is a detailed medical history and physical check. We look for signs like headaches, nausea, and changes in behavior. These could mean a brain tumor.
We also do a neurological exam. This checks vision, hearing, balance, and coordination. It helps find any brain tumor signs.
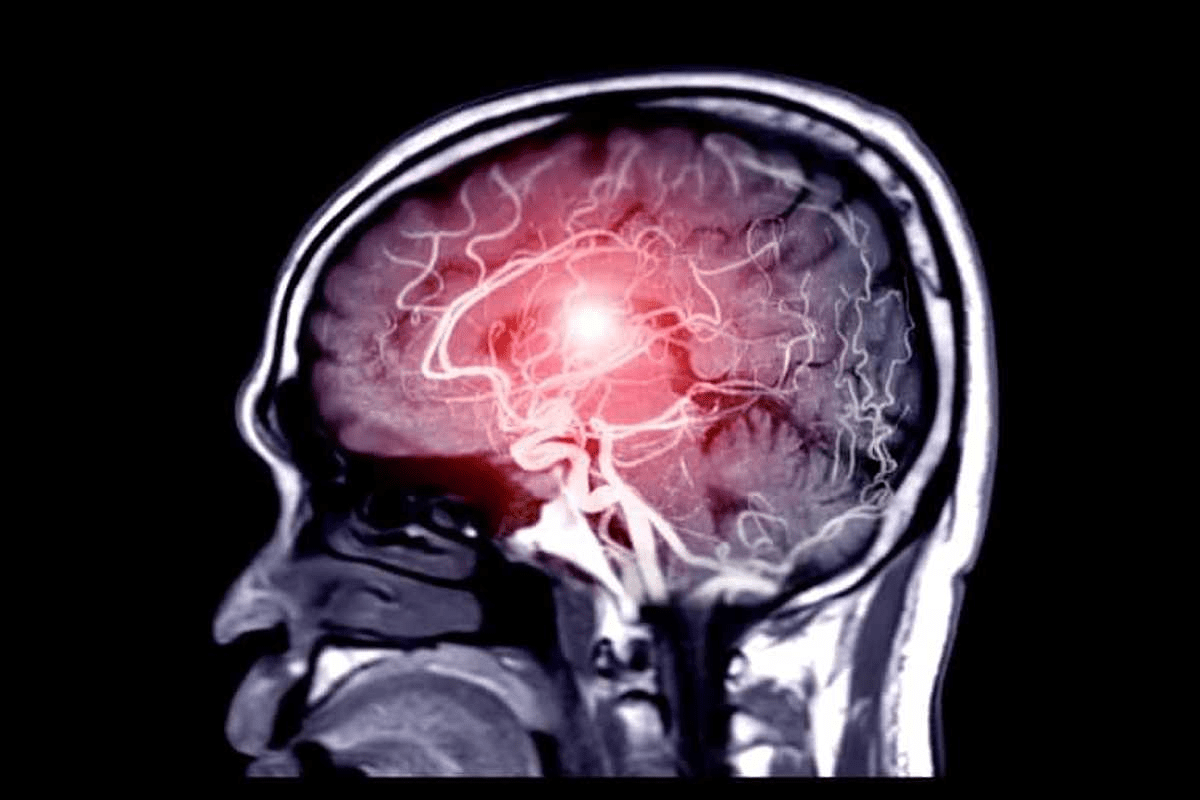
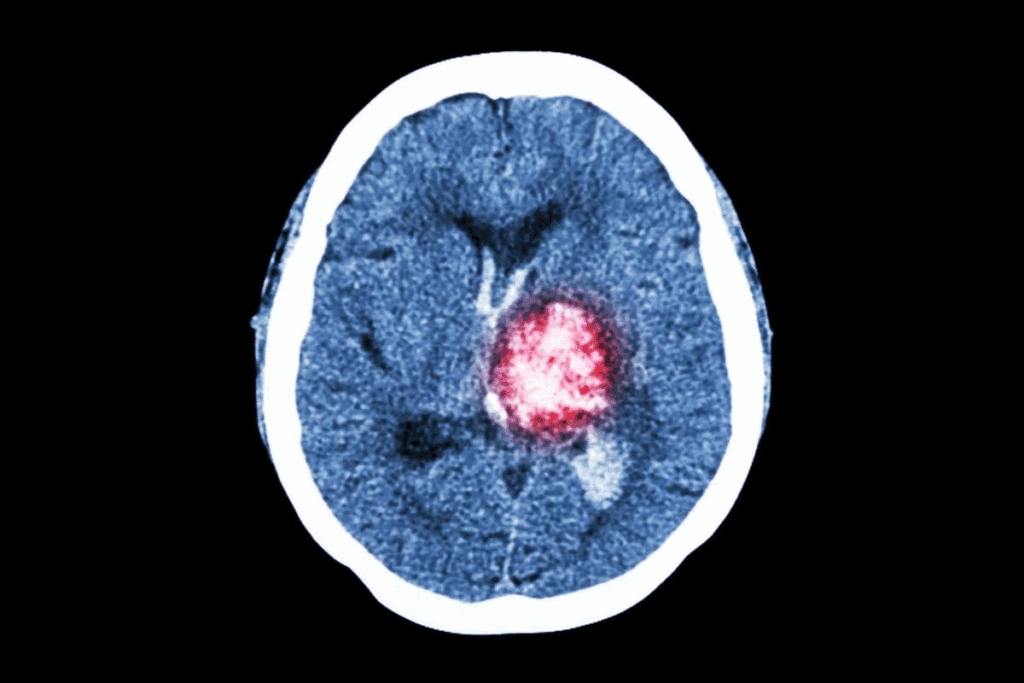
Imaging Techniques (MRI, CT Scans)
Imaging is key in finding brain tumors in kids. We use MRI and CT scans to see the tumor and where it is.
MRI gives detailed brain images without radiation. CT scans are quicker and good for emergencies.
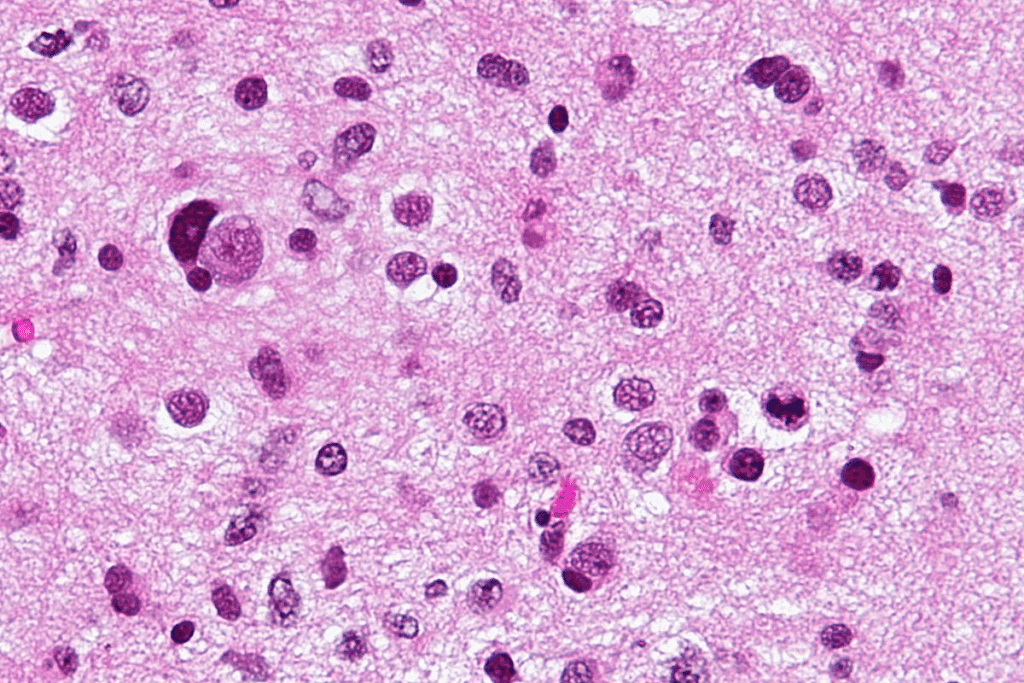
Biopsy and Pathological Examination
A biopsy takes a tumor sample for study. We then examine it to find out the tumor type and grade.
This info is vital for treatment planning. It tells us about the tumor’s aggressiveness and how it might react to treatment.
Newer Diagnostic Approaches
We’re also looking into new methods like liquid biopsy and advanced molecular diagnostics. These could make diagnosis more accurate and treatment more tailored.
Liquid biopsy finds tumor DNA in blood or cerebrospinal fluid. It’s a less invasive way to diagnose and track brain tumors.
| Diagnostic Method | Description | Advantages |
| MRI | Magnetic Resonance Imaging provides detailed brain images without radiation. | High-resolution images, no radiation exposure. |
| CT Scan | Computed Tomography scans quickly image the brain. | Quick, useful in emergencies. |
| Biopsy | Surgical removal of tumor tissue for examination. | Provides tumor type and grade. |
| Liquid Biopsy | Detection of tumor DNA in blood or cerebrospinal fluid. | Less invasive, possible for monitoring. |
Staging and Grading of Pediatric Brain Tumors
Staging and grading of pediatric brain tumors are key for effective treatment. They help doctors plan the best course of action. This improves chances of survival.
Understanding the Staging System
The staging system for pediatric brain tumors shows how far the tumor has spread. Unlike adult cancers, it doesn’t use the TNM system. Instead, it looks at the tumor’s spread, how much is left after surgery, and other specific factors.
For some tumors, like medulloblastoma, the system considers the child’s age, if the tumor has spread, and how much was removed. This info is vital for treatment planning and predicting the outcome.
Grade 1-4 Brain Tumors Explained
Brain tumors are graded from 1 to 4 based on their characteristics. Grade 1 is the least aggressive, and Grade 4 is the most. The grade is determined by how fast the tumor grows, how abnormal the cells are, and other microscopic features.
- Grade 1 Tumors: These grow slowly and have a good prognosis. Pilocytic astrocytomas are examples.
- Grade 2 Tumors: These are moderately differentiated and may come back. They are considered low to moderate grade.
- Grade 3 Tumors: These are anaplastic and more aggressive. They have a higher chance of coming back.
- Grade 4 Tumors: These are the most aggressive, grow quickly, and have a poor prognosis. Glioblastoma is an example.
Implications of Tumor Grade on Treatment
The tumor’s grade affects the treatment plan. Higher-grade tumors need more aggressive treatment, like surgery, radiation, and chemotherapy. Lower-grade tumors might just need surgery or be watched with regular scans.
Treatment choices also depend on the tumor’s location, the child’s age, and health. For example, young children might avoid radiation to protect their developing brains.
Survival Rates by Stage and Grade
Survival rates for pediatric brain tumors vary a lot. They depend on the tumor type, grade, and stage at diagnosis. Children with low-grade tumors usually have a better chance than those with high-grade tumors.
| Tumor Grade | 5-Year Survival Rate |
| Grade 1 | 80-90% |
| Grade 2 | 60-80% |
| Grade 3 | 30-60% |
| Grade 4 | Less than 30% |
Understanding the staging and grading of pediatric brain tumors is key for families. It helps them understand the diagnosis and treatment plan. It also sets the stage for discussing prognosis and the outcomes of different treatments.
Treatment Options for Childhood Brain Tumors
Childhood brain tumors need a team effort to treat. Doctors use many ways to fight these tumors. Each method has its own good points and possible downsides.
Surgical Interventions
Surgery is often the first step for many brain tumors in kids. The goal is to take out as much tumor as safe. This helps keep the brain working right.
Key considerations for surgical interventions include:
- The location and size of the tumor
- The child’s overall health and age
- The chance of problems after surgery
Radiation Therapy Considerations in Children
Radiation therapy is key for treating brain tumors in kids. It uses high-energy rays to kill tumor cells. But, it must be done carefully to protect the growing brain.
Radiation therapy considerations include:
- The type and dose of radiation
- The age of the child, as younger children are more susceptible to radiation effects
- The chance of long-term side effects on thinking and hormones
Chemotherapy Protocols
Chemotherapy kills tumor cells or stops them from growing. For kids, doctors pick the best drugs to be effective yet safe.
Chemotherapy protocols involve:
- Picking the right drugs for the tumor type
- Watching for side effects and adjusting doses as needed
- Using chemotherapy with surgery and radiation
Targeted Therapies and Immunotherapy
Targeted therapies and immunotherapy are new ways to fight brain tumors in kids. They aim to find and attack tumor cells more precisely. This might mean fewer side effects.
Benefits of targeted therapies and immunotherapy include:
- More precise targeting of tumor cells
- Potential for less harm compared to traditional chemotherapy
- Research is ongoing to find new targets and treatments
Long-term Prognosis and Quality of Life
When a child is diagnosed with a brain tumor, families and healthcare providers focus on the long-term prognosis. The goal is not just to treat the tumor. It’s also to ensure the child has the best quality of life.
Factors Affecting Prognosis
Several factors affect a child’s long-term prognosis with brain tumors. These include the tumor type and grade, the child’s age at diagnosis, and the initial treatment’s success. Tumor type and grade are key because they show how aggressive the tumor is and how it might respond to treatment.
The child’s overall health and how well they tolerate treatment also matter. Thanks to medical advancements, survival rates have improved. It’s important to stay up-to-date with the latest treatments.
Survival Statistics by Tumor Type
Survival rates vary by brain tumor type. For example, children with medulloblastoma have seen better survival rates thanks to new chemotherapy and radiation therapies. On the other hand, tumors like DIPG are harder to treat, with less hopeful outlooks.
| Tumor Type | 5-Year Survival Rate | 10-Year Survival Rate |
| Medulloblastoma | 70-80% | 60-70% |
| Astrocytoma | 80-90% | 70-80% |
| DIPG | <10% | <5% |
Long-term Side Effects of Treatment
Treatment for brain tumors can lead to long-term side effects. These can include cognitive, neurological, and endocrine issues. The severity of these effects depends on the treatment used and the child’s age during treatment.
There’s a growing need for supportive care to manage these side effects. This includes rehabilitation, psychological support, and educational help.
Cognitive and Developmental Outcomes
Cognitive and developmental outcomes are key to the long-term prognosis. Children treated for brain tumors may face challenges in learning, memory, and social development. Early intervention and tailored educational plans can help a lot.
A multidisciplinary care team is essential to address these needs. This way, we can improve the long-term quality of life for these children. We aim to support them in leading fulfilling lives.
Support Resources for Families
Dealing with pediatric brain tumors is tough for families. They need strong support systems. Care for these young patients includes medical treatment and many support resources.
Medical Support Teams
Medical teams are key in caring for kids with brain tumors. These teams have doctors, nurses, and specialists. They work together to meet each child’s needs.
Financial Assistance Programs
Families with pediatric brain tumors often need financial help. Treatment costs a lot. Many organizations offer aid for medical bills and travel.
| Program Name | Description | Eligibility Criteria |
| Children’s Cancer Foundation | Provides financial assistance for medical expenses and family support services. | Families with children diagnosed with cancer, including brain tumors. |
| Family Support Program | Offers aid for travel, accommodation, and other expenses related to treatment. | Families undergoing treatment for their child’s cancer. |
Support Groups and Counseling
Support groups and counseling help families deal with the emotional side of a brain tumor diagnosis. They offer a place to share, get support, and learn from others.
Educational Resources and School Reintegration
Helping kids with brain tumors stay in school is important. Schools and healthcare teams work together to help. They create plans for each child’s education.
With these support resources, families can handle the challenges of pediatric brain tumors. They ensure their child gets the care they need.
Conclusion
Understanding pediatric brain tumors is key for early detection and treatment. This overview has examined prevalence, risk factors, types, and symptoms. It has also covered diagnostic and treatment approaches, and the importance of comprehensive family care.
Pediatric brain tumors need a team effort for treatment. This includes surgery, radiation, chemotherapy, and special therapies. The outcome and life quality for kids depend on the tumor type, stage, and grade.
In wrapping up, we stress the need for awareness and support for families with pediatric brain tumors. With the right care and resources, we can help improve their lives. Our goal is to provide top-notch healthcare with care and skill, meeting the needs of patients from around the world.
FAQ
What are the most common types of pediatric brain tumors?
Pediatric brain tumors include medulloblastoma, astrocytoma, ependymoma, and DIPG. Each type has its own characteristics and treatment options.
What are the early warning signs of brain cancer in infants?
Signs of brain cancer in infants include a large head, vomiting, and lethargy. Also, changes in feeding or vision are important. Seek medical help if these signs don’t go away.
How do brain tumor symptoms vary by location?
Symptoms change based on where the tumor is. For example, cerebellar tumors affect balance. Brain stem tumors can cause swallowing or breathing problems.
What diagnostic procedures are used to identify pediatric brain tumors?
To find pediatric brain tumors, doctors use MRI, CT scans, biopsy, and pathological exams. New methods are being tested to improve diagnosis.
How are pediatric brain tumors staged and graded?
Tumors are staged and graded based on their severity. Staging shows how far the tumor has spread. Grading (1-4) shows how aggressive it is, affecting treatment and survival.
What treatment options are available for childhood brain tumors?
Treatments include surgery, radiation, chemotherapy, and targeted therapies. The choice depends on the tumor type, stage, and the child’s health.
What are the long-term prognosis and quality of life for children with brain tumors?
The prognosis and quality of life depend on the tumor type, treatment, and side effects. Cognitive and developmental outcomes are also key.
What support resources are available for families affected by pediatric brain tumors?
Families can find support through medical teams, financial help, support groups, counseling, and educational resources. These help with diagnosis and treatment challenges.
Can children survive a brain tumor?
Survival rates vary by tumor type, stage, and grade. Advances in treatment have improved survival chances. Many children can live fulfilling lives with the right care.
How common are brain tumors in children?
Brain tumors are rare in children but common in cancer cases. Knowing this can help raise awareness and encourage early detection.
What are the risk factors for pediatric brain tumors?
Risk factors include genetic predispositions, environmental exposures, and prenatal factors. Identifying these risks can help spot children at higher risk.
References
- Djouder, N., & Rigual, M. del Mar. (2025). CNIO researchers discover a new mechanism for rapid liver regeneration triggered by glutamate. Nature. https://www.cnio.es/en/news/cnio-researchers-discover-a-new-mechanism-for-rapid-liver-regeneration-triggered-by-glutamate/