Last Updated on November 25, 2025 by Ugurkan Demir

Heart block, also known as atrioventricular block or electrical blockage, happens when electrical signals don’t move right between the heart’s upper and lower chambers. A normal heart rate is between 60 to 100 beats per minute, showing a healthy adult. But, if heartbeats slow down, it could mean a heart block.Understand 7 signs of heart block, its types, and treatment options for managing this cardiac issue.
Knowing the signs of heart block is key for quick medical help. We’ll look at the different heart block types, their symptoms, and treatments. We’ll stress the need for early detection and expert care.
Key Takeaways
- Heart block refers to impaired electrical signal conduction between the heart’s chambers.
- A heart rate below 60 beats per minute may indicate a heart block.
- Early detection is critical for effective treatment.
- Different types of heart block need different treatments.
- Specialized care can greatly improve heart health outcomes.
What Is Heart Block? Understanding Electrical Conduction Problems

Heart block, or atrioventricular (AV) block, happens when electrical signals between heart chambers are delayed or blocked. This can cause irregular heartbeats. It affects the heart’s ability to pump blood efficiently.
Definition of Atrioventricular Block
Atrioventricular block is when signals between the heart’s upper and lower chambers are blocked. This can happen at different levels, causing various degrees of heart block.
There are three main types of heart block: first-degree, second-degree (split into Type 1 and Type 2), and third-degree (complete). Each type shows a different level of disruption in the heart’s electrical system.
Normal Cardiac Electrical Pathways
The heart’s electrical system follows a specific path. The sinoatrial (SA) node starts the electrical impulses. These signals then go through the atrioventricular (AV) node, the Bundle of His, and the bundle branches to the ventricles. This ensures the heart beats and pumps blood well.
This pathway is key for a regular heartbeat. Any problem here can cause arrhythmias or heart issues.
How Conduction Disruptions Occur
Disruptions in the electrical pathways can happen for many reasons. These include aging, heart diseases, ischemia, or some medications. These disruptions can cause symptoms from mild to severe, based on the blockage’s degree.
Knowing how disruptions happen is important for diagnosing and treating heart block. The type and severity of the block decide the treatment, which can be monitoring or a pacemaker.
Key factors that cause disruptions include:
- Age-related wear and tear on the heart’s electrical system
- Structural heart diseases that affect the heart’s anatomy
- Ischemia or myocardial infarction that damages the heart muscle
- Medications that alter the heart’s electrical activity
The 7 Signs of Heart Block You Should Never Ignore

Heart block symptoms can be subtle, but there are seven key indicators that should never be ignored. Recognizing these signs is key for timely medical help and preventing severe complications. Most people with heart block experience symptoms like dizziness, fatigue, and slow heart rate.
Unexplained Fatigue and Weakness
Unexplained fatigue and weakness are common in heart block. The heart’s trouble pumping blood can lower physical performance and endurance. This fatigue doesn’t go away with rest. It’s important to find the right cause to get the right care.
Dizziness and Lightheadedness
Dizziness and lightheadedness are serious symptoms that need quick attention. These happen when the brain doesn’t get enough blood flow, often because the heart can’t pump well. People might feel like they’re going to pass out or that things are spinning around them. Finding the cause is key to managing these symptoms.
Fainting Episodes (Syncope)
Fainting, or syncope, is a severe symptom that can mean a big problem with the heart’s electrical activity. When the heart’s conduction system fails, it can cause sudden loss of consciousness. Syncope is dangerous because it raises the risk of injury from falls. Quick medical check-up is needed to find the cause and treatment.
Shortness of Breath
Shortness of breath, or dyspnea, can happen with heart block because the heart can’t pump blood well. This can cause fluid to build up in the lungs, making it hard to breathe. This symptom can happen during activity or even when resting in severe cases. It’s important to understand how heart block and shortness of breath are connected for proper care.
| Symptom | Description | Possible Cause |
| Unexplained Fatigue and Weakness | Persistent tiredness and lack of energy | Inadequate blood flow due to disrupted heart rhythm |
| Dizziness and Lightheadedness | Feeling of impending faint or spinning sensation | Reduced blood flow to the brain |
| Fainting Episodes (Syncope) | Sudden loss of consciousness | Severe disruption of heart’s electrical activity |
| Shortness of Breath | Difficulty breathing | Inadequate heart pumping leading to fluid buildup in lungs |
Knowing the seven signs of heart block is key for getting medical help on time. By understanding these symptoms, people can get the right care and avoid serious problems.
First Degree Heart Block: The Initial Stage
Understanding first-degree heart block is key for early detection and management. It’s a condition where the electrical impulses that control the heartbeat are slowed. This happens as they move from the atria to the ventricles.
Electrical Delay Characteristics
In first-degree heart block, the electrical delay is shown by a long PR interval on an electrocardiogram (ECG). This means the impulse takes longer than usual to get from the atria to the ventricles.
The PR interval is considered long if it’s over 0.2 seconds. This is a key sign that helps doctors tell first-degree heart block apart from other heart block types.
Minimal or Absent Symptoms
Many people with first-degree heart block don’t show any symptoms. It might be found by chance during an ECG done for another reason.
In some cases, people might feel bradycardia (a slower heart rate). But this isn’t always the case.
ECG Findings and Diagnosis
Doctors diagnose first-degree heart block mainly by looking at ECGs. The ECG shows a long PR interval, which is a key sign of this condition.
ECG interpretation needs skill. But seeing a long PR interval without missing beats is a clear sign of first-degree heart block.
Monitoring vs. Treatment Approaches
For most people with first-degree heart block, it’s not serious and doesn’t need treatment. But, it’s important to keep an eye on it to make sure it doesn’t get worse.
Monitoring usually means regular ECGs and check-ups. If symptoms show up or the condition gets worse, doctors might suggest treatments like pacing.
Second Degree Heart Block Type 1: Wenckebach Phenomenon
The Wenckebach phenomenon is a type of second-degree heart block. It shows a delay in electrical signals. Knowing about it helps in giving the right care and management.
Progressive Conduction Delay Pattern
In Wenckebach phenomenon, signals from the atria to the ventricles get delayed. This delay gets longer until a beat is blocked. On an electrocardiogram (ECG), this looks like the PR interval gets longer and then a P wave is not followed by a QRS complex.
Key Features of Wenckebach Phenomenon:
- Progressive prolongation of the PR interval
- Eventual block of a P wave
- Normal QRS complex duration
Common Symptoms and Their Severity
People with Wenckebach phenomenon might feel dizzy, lightheaded, or tired. These feelings come from the heart’s irregular rhythm. Some might not feel anything and only find out during an ECG for another reason.
“The presence of symptoms can vary widely among individuals with Wenckebach phenomenon, necessitating a thorough clinical evaluation to determine the best course of action.” –
Cardiology Expert
Causes and Risk Factors
Wenckebach phenomenon can happen for many reasons. It can be due to aging, heart diseases, or some medicines. Knowing the cause helps in managing it better.
| Cause/Risk Factor | Description |
| Age-related degeneration | Wear and tear on the heart’s conduction system over time |
| Structural heart diseases | Conditions like coronary artery disease or cardiomyopathy |
| Medications | Certain drugs that affect heart conduction, such as beta-blockers |
Management Strategies
Managing Wenckebach phenomenon depends on symptoms and the cause. For those without symptoms, just watching might be enough. But for those with symptoms, doctors might change medicines, treat heart issues, or even suggest a pacemaker.
Understanding Wenckebach phenomenon helps doctors find the best ways to help patients. This improves how well patients do.
Second Degree Heart Block Type 2: Mobitz II
Understanding second-degree heart block type 2, or Mobitz II, is key. It shows a serious problem with the heart’s electrical system. This condition blocks electrical impulses between the heart’s upper and lower chambers sometimes.
Sudden Conduction Failure Characteristics
In Mobitz II, electrical impulses are blocked suddenly and without warning. This is different from Mobitz I, where the delay gets worse over time. This sudden blockage is very concerning because it can cause a big drop in heart rate without any warning.
Serious Symptoms and Warning Signs
Symptoms of Mobitz II are often more severe than other heart block types. People might feel dizzy, faint, or have trouble breathing. These symptoms are important warning signs of a serious problem. A doctor said, “Mobitz II is a big warning sign for complete heart block, and we need to act fast.”
Increased Risk for Complete Block
Mobitz II is linked to a higher risk of complete (third-degree) heart block. In complete heart block, all electrical impulses are blocked. This can lead to a very slow heart rate and serious health risks. It’s very important to catch and treat Mobitz II early to avoid these dangers.
Treatment Necessities
Treatment for Mobitz II is often needed to stop it from getting worse. The main treatment is getting a permanent pacemaker. This device helps keep the heart rate steady by sending out electrical impulses.
“Pacemaker therapy has changed how we treat Mobitz II. It has greatly improved patient outcomes and quality of life,” a cardiologist said.
In summary, Mobitz II is a serious heart block that needs quick attention and treatment. Knowing its signs, symptoms, and treatment options is key to managing it well.
Third Degree (Complete) Heart Block: When Signals Stop
Third-degree heart block, also known as complete heart block, is a serious condition. It happens when electrical signals between the heart’s chambers are blocked. This leads to severe bradycardia and can be life-threatening.
Complete AV Dissociation Explained
In complete heart block, electrical impulses from the atria can’t reach the ventricles. This means the atria and ventricles beat on their own. The ventricles beat very slowly, usually between 20-40 beats per minute.
“The ventricles rely on an escape pacemaker to maintain a ventricular rate,” says a leading cardiologist. “This rate is often too slow to keep the heart pumping enough blood.” This can cause symptoms like dizziness, fainting, and shortness of breath.
Recognizing Life-Threatening Symptoms
Patients with third-degree heart block often have severe symptoms. These include:
- Severe fatigue and weakness
- Dizziness and lightheadedness
- Fainting episodes (syncope)
- Shortness of breath
- Chest pain
These symptoms show the heart can’t meet the body’s needs. If you see these signs, get medical help right away.
Emergency Situations and Response
In third-degree heart block, emergencies can happen if the heart rate gets too slow. Or if there’s a long pause in heart activity. Quick action is needed to stop cardiac arrest.
Emergency response may include:
- Cardiopulmonary resuscitation (CPR)
- Temporary pacing to restore a stable heart rate
- Administration of medications to increase heart rate
Long-term Management Requirements
Managing third-degree heart block long-term usually means getting a permanent pacemaker. This device helps the heart beat normally and improves blood flow. It helps reduce symptoms and improves life quality.
Seeing a cardiologist regularly is key to check the pacemaker’s work. They might also suggest lifestyle changes to help manage the condition.
Comparing Different Types of Heart Block: What You Need to Know
Heart block is not just one condition. It’s a range of disorders that affect the heart’s electrical system. Knowing the different types is key to finding the right treatment. The severity of heart block goes from first-degree to third-degree, which is the most severe.
Progression From First to Third Degree
The severity of heart block increases from first-degree to third-degree. First-degree heart block causes a delay in electrical signals. Second-degree heart block blocks some signals. Third-degree (complete) heart block blocks all signals.
Symptom Severity Comparison
Symptoms of heart block vary by type and severity. First-degree heart block usually has no symptoms. Second-degree heart block can cause dizziness and shortness of breath. Third-degree heart block has severe symptoms like syncope and heart failure.
Prognosis Differences
The outlook for heart block patients varies by type and severity. People with first-degree heart block usually have a good prognosis. Those with second-degree heart block may have a more variable outcome. Third-degree heart block has a poorer prognosis due to serious complications.
Treatment Approach Variations
Treatment for heart block depends on the type and severity. First-degree heart block often needs just monitoring. Second-degree and third-degree heart block may require more treatments, like pacemaker implantation. Treatment is chosen based on the individual’s health and needs.
What Causes Heart Block? Understanding the Underlying Factors
Knowing what causes heart block is key to managing it well. Heart block isn’t just one thing. It’s a condition caused by many factors affecting the heart’s electrical system.
Many things can lead to heart block. We’ll look at each one to understand it better.
Age-Related Degeneration
As we get older, our heart’s electrical system can wear out. This can cause heart block. It makes the heart’s signals slow down or stop, affecting its rhythm.
Structural Heart Diseases
Heart diseases can also cause heart block. Conditions like coronary artery disease and heart valve problems can harm the heart’s electrical paths. For example, coronary artery disease can lead to ischemia, causing heart block.
Some heart diseases that can lead to heart block include:
- Coronary artery disease
- Heart valve disorders
- Cardiomyopathy
- Congenital heart defects
Ischemia and Myocardial Infarction
Ischemia, or reduced blood flow to the heart, can damage the electrical system. This can lead to heart block. A heart attack is a severe form of ischemia that can cause significant damage, leading to heart block.
Ischemia can cause different types of heart block, depending on the damage. Understanding this is key to treating it quickly and effectively.
Medication-Induced Conduction Problems
Some medicines can affect the heart’s electrical system, causing heart block. Drugs that slow the heart rate or affect the electrical pathways can lead to problems.
Some medicines that might cause these problems include:
- Beta-blockers
- Calcium channel blockers
- Anti-arrhythmic drugs
It’s important to watch how these medicines affect the heart’s electrical system. This helps prevent or manage heart block.
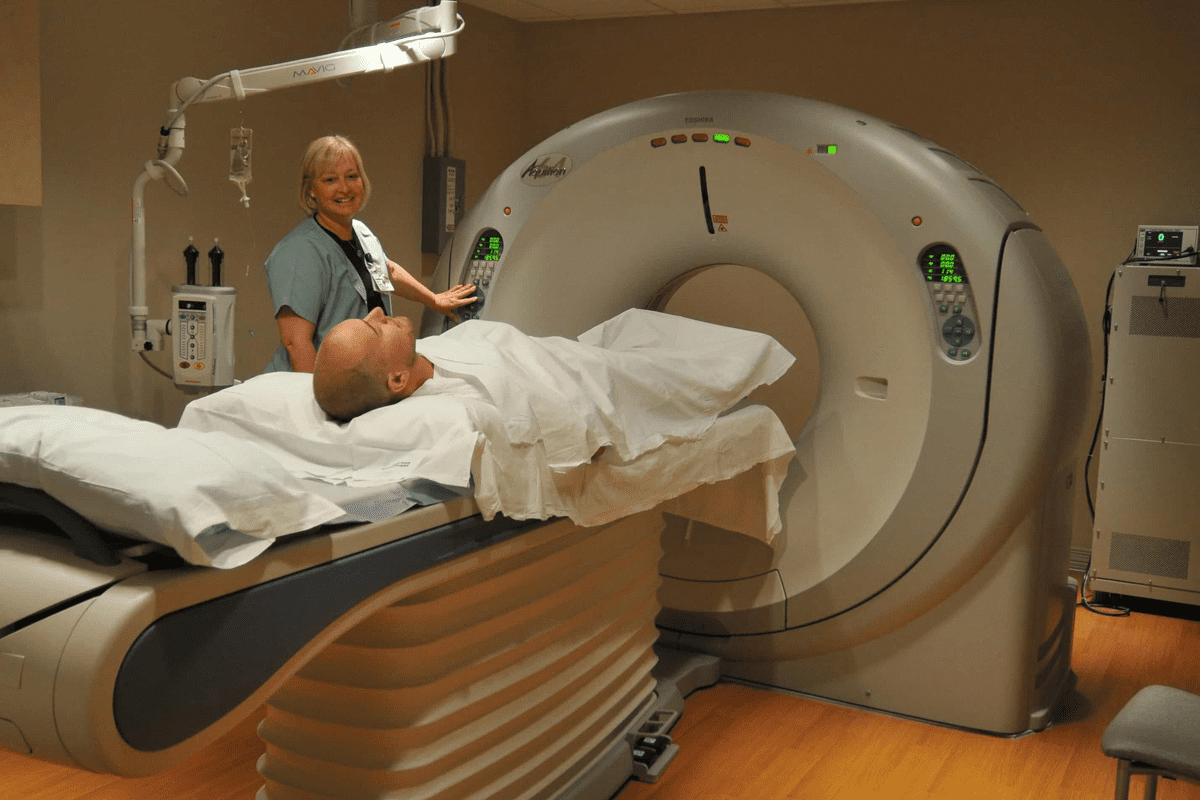
Diagnosing Heart Block: From Symptoms to Confirmation
To find out if someone has heart block, doctors use many methods. They start with a check-up and then do more tests. This way, they can figure out the best treatment.
Initial Clinical Evaluation
The first step is a detailed check-up. Doctors look at the patient’s past health and any symptoms like dizziness or shortness of breath. They also do a physical exam to see if there are any signs of heart problems.
They also check the patient’s medicines. Some drugs can affect the heart’s rhythm. This helps decide if more tests are needed.
Electrocardiogram (ECG) Patterns
An electrocardiogram (ECG) is key in diagnosing heart block. It shows how the heart’s electrical activity works. Certain patterns on the ECG can show if there’s heart block.
For example, a first-degree heart block shows a long PR interval on the ECG. A third-degree heart block shows no connection between the heart’s upper and lower chambers. We look at these patterns to confirm the diagnosis and understand how serious it is.
Holter and Event Monitoring
For those with symptoms that come and go, doctors might suggest a Holter or event monitor. A Holter monitor records the heart’s activity for 24 to 48 hours. It shows how the heart works during everyday life.
Event monitors are used for longer periods and can be turned on by the patient during symptoms. They help us see how symptoms relate to heart rhythm problems, helping us diagnose heart block.
Electrophysiology Studies
In some cases, an electrophysiology study (EPS) is done. This test directly checks the heart’s electrical system. Catheters are used to record electrical activity from inside the heart.
This test gives detailed info about the heart’s electrical system. It helps us find the best treatment for the patient.
By using all these tests, doctors can accurately diagnose heart block. Then, they can create a treatment plan that fits the patient’s needs.
How to Treat Heart Block: From Observation to Intervention
Heart block treatment varies widely. It can range from simple monitoring to complex interventions. The choice depends on the heart block type, its severity, the patient’s health, and symptoms.
Monitoring Approaches for Mild Cases
Patients with first-degree heart block or mild second-degree heart block might just need monitoring. They’ll have regular check-ups and ECGs to watch the condition. Regular monitoring helps doctors step in if things get worse.
Medication Adjustments and Considerations
Heart block can sometimes be caused by medications. Adjusting or discontinuing these can help manage it. For example, if beta-blockers or certain anti-arrhythmics are causing problems, other options might be better.
Temporary Pacing Methods
For those with symptomatic heart block, temporary pacing might be needed. This uses a temporary pacemaker to keep the heartbeat steady until a permanent fix is found.
Permanent Pacemaker Implantation
Advanced heart block often requires a permanent pacemaker implantation. This involves surgery to put in a device that controls the heartbeat. The decision to get a pacemaker depends on how bad the symptoms are and the heart block type.
Effective heart block treatment needs a personalized approach. By knowing the different options, doctors can give the best care to patients with heart block.
Living with Heart Block: Lifestyle Modifications and Management
For those with heart block, a heart-healthy lifestyle is key. It helps reduce symptoms and boosts well-being. A good plan includes lifestyle changes, medical care, and regular check-ups.
Physical Activity Guidelines and Limitations
Staying active is vital for heart health, but heart block patients must be careful. Moderate-intensity exercises like brisk walking or swimming are best. Always talk to a doctor before starting any new exercise, if you feel dizzy or faint.
High-intensity workouts can worsen symptoms. Instead, try gentle exercises like yoga or tai chi. They help with flexibility and stress.
Dietary Considerations
Eating right is important for heart block management. Lowering sodium intake helps prevent fluid buildup and high blood pressure. Eat more fruits, veggies, whole grains, and lean proteins.
- Eat foods high in potassium, like bananas, to balance sodium.
- Drink lots of water to stay hydrated.
- Limit caffeine and alcohol, as they can affect heart rhythm.
Stress Management Techniques
Stress can make heart block symptoms worse. Managing stress is key. Try meditation, deep breathing exercises, and progressive muscle relaxation to relax.
Doing hobbies, spending time with family, and getting enough sleep also help manage stress.
Regular Medical Follow-ups
Regular doctor visits are essential for heart block care. They help monitor the condition and adjust treatments as needed. This also catches any complications early.
Stick to your follow-up schedule and tell your doctor about any symptom changes or health issues.
Conclusion: Navigating Life with Heart Block
Understanding heart block is key to managing it. With the right treatment, people with heart block can stay active. Managing heart block means using medicine, changing lifestyle habits, and keeping an eye on health.
Knowing the signs of heart block helps get medical help fast. This can prevent serious problems. Eating well, exercising, and managing stress are all important for heart health.
Good heart block management helps reduce symptoms and stops the condition from getting worse. With the right care, people with heart block can live well and stay healthy.
FAQ
What is heart block, and how does it affect the heart?
Heart block happens when the heart’s electrical signals get mixed up. This can make the heart beat too slow or irregularly. It might need medical help to fix.
What are the different types of heart block?
Heart block comes in three main types: first-degree, second-degree (split into Type 1 and Type 2), and third-degree (complete). Each type has its own level of seriousness.
What are the signs and symptoms of heart block?
Signs of heart block include feeling very tired, dizzy, or faint. You might also have trouble breathing or notice your heart beating oddly. These signs mean you should see a doctor right away.
How is heart block diagnosed?
Doctors use tests like ECGs and Holter monitors to find heart block. They also do electrophysiology studies. These help figure out how bad it is.
What causes heart block?
Heart block can come from getting older, heart diseases, or heart attacks. Some medicines can also cause it. Knowing why it happens helps in treating it.
How is heart block treated?
Treatment for heart block varies. For mild cases, doctors might just watch it. For more serious ones, they might use medicines, temporary pacing, or even implant a pacemaker. The treatment depends on how bad it is.
Can lifestyle modifications help manage heart block?
Yes, changing your lifestyle can help. This includes exercising, eating right, managing stress, and seeing your doctor regularly. These steps can improve your life with heart block.
What is the difference between first-degree and third-degree heart block?
First-degree heart block is a minor delay in signals, often without symptoms. Third-degree heart block is a total block, causing serious problems and needing urgent care.
How does second-degree heart block type 1 differ from type 2?
Type 1 second-degree heart block, or Wenckebach, shows a slow delay in signals. Type 2, or Mobitz II, has sudden stops in signals. Type 2 is more serious and can lead to complete block.
What is the prognosis for individuals with heart block?
The outlook for heart block depends on its type and how bad it is. With the right treatment, many people can live active and happy lives.
Can heart block be prevented?
Some heart block causes can’t be stopped, but you can lower your risk. This includes managing health conditions, living a healthy lifestyle, and watching your medicines.
References:
- Martinez-Lemus, L. A. (2012). The dynamic structure of arterioles. Basic & Clinical Pharmacology & Toxicology, 110(1), 5-11. https://pubmed.ncbi.nlm.nih.gov/21989114/