
Osteoporosis is a bone disease that affects millions. It makes bones weak, raising the risk of fractures. Bisphosphonate treatment is a key way to fight this.Guide on taking bisphosphonate treatment for osteoporosis, focusing on safe administration and adherence tips.
These drugs stop bones from breaking down. This slows bone loss and lowers the chance of fractures in both men and women. Knowing how to take bisphosphonates right can help patients get the most from their osteoporosis treatment.
Key Takeaways
- Bisphosphonates are a first-line treatment for osteoporosis.
- Proper administration is key for effective treatment.
- Bisphosphonates reduce fracture risk by slowing bone loss.
- Knowing how to take bisphosphonates is vital for maximum benefits.
- Managing osteoporosis well means using medicine and making lifestyle changes.
Understanding Osteoporosis and Its Impact
It’s important to know about osteoporosis to tackle its effects on people and communities. Osteoporosis weakens bones, making them more likely to break.
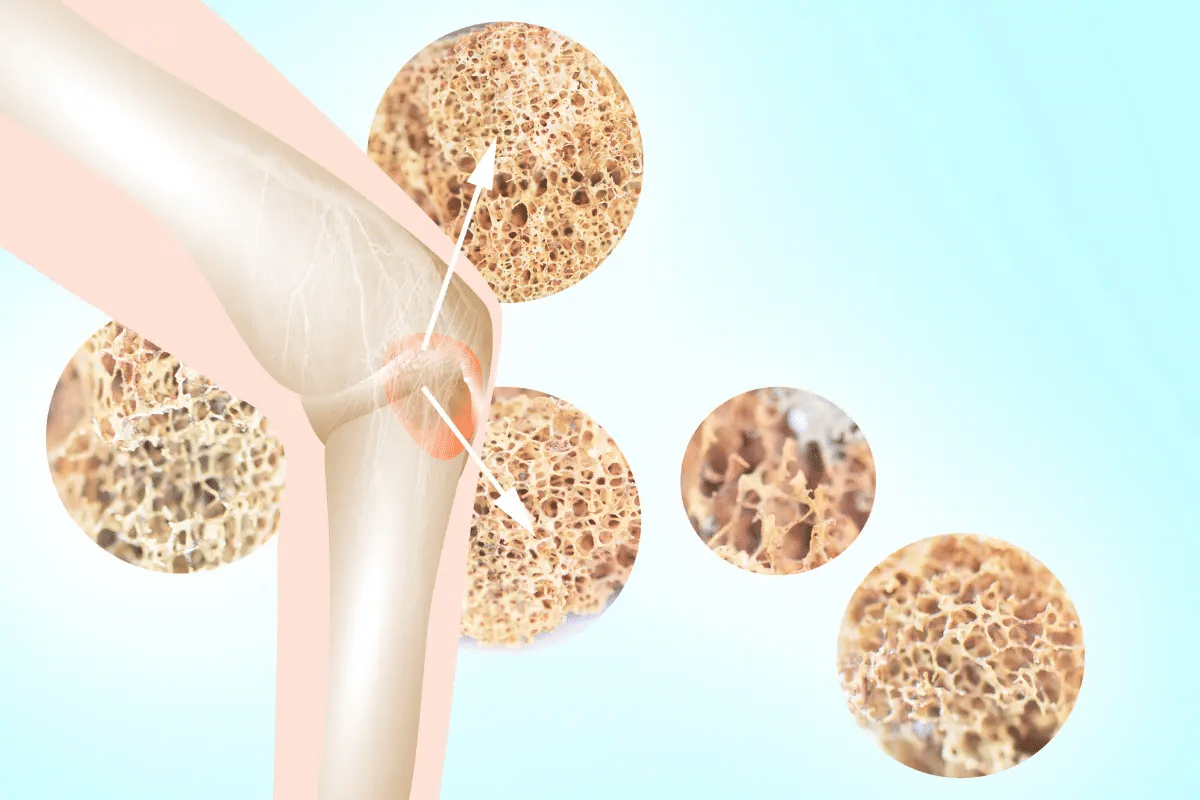
What Is Osteoporosis?
Osteoporosis is called a “silent disease” because it often goes unnoticed until a bone breaks. It happens when the body loses more bone than it makes, leading to weaker bones.
Key characteristics of osteoporosis include:
- Reduced bone mass
- Deterioration of bone tissue
- Increased risk of fractures
Risk Factors and Prevalence
Several factors can increase the risk of osteoporosis. These include:
- Age: The risk grows with age.
- Gender: Women are more at risk than men.
- Family history: Having relatives with osteoporosis or fractures.
- Lifestyle factors: Being inactive, smoking, and drinking too much alcohol.
Osteoporosis affects millions globally, impacting their lives and healthcare costs. Studies show it’s common among the elderly.
Consequences of Untreated Osteoporosis
Untreated osteoporosis can cause serious problems, including:
- Vertebral fractures, leading to loss of height and spinal deformity.
- Non-vertebral fractures, like hip fractures, which can be deadly.
- Chronic pain and disability.
People with low bone density or past fractures might be advised to take bisphosphonates. Conditions like Paget’s disease or bone cancer also require this treatment. Studies show bisphosphonates can lower the risk of fractures by 33 to 49 percent over 3 years or more.
Grasping these aspects of osteoporosis is key to creating effective treatments and better patient care.
The Science Behind Bisphosphonate Treatment
It’s important to understand how bisphosphonates work to manage osteoporosis. These medications are used to slow bone loss and lower fracture risk.
How Bisphosphonates Work
Bisphosphonates stop bone loss by slowing down bone resorption. This action is key in reducing fracture risk in people with osteoporosis. They bind to bone surfaces, reducing osteoclast activity. Osteoclasts are cells that break down bone.
By reducing bone resorption, bisphosphonates increase bone mineral density (BMD). BMD is a key measure of bone health. Studies show bisphosphonates can boost BMD in the spine and hip. These areas are common fracture sites.
Effectiveness in Reducing Fracture Risk
Many studies prove bisphosphonates’ effectiveness in lowering fracture risk. They reduce bone turnover, lowering the risk of vertebral and non-vertebral fractures. Data show that about 12.4 months of treatment can prevent one non-vertebral fracture per 100 postmenopausal women with osteoporosis.
- Reduction in vertebral fractures
- Decrease in non-vertebral fractures
- Increase in bone mineral density
Clinical Evidence Supporting Use
Many clinical studies back the use of bisphosphonates for osteoporosis treatment. These studies show bisphosphonates reduce fractures and increase BMD in both men and women. For example, the Fracture Intervention Trial (FIT) showed their effectiveness in lowering fracture risk.
“Bisphosphonates have become a cornerstone in the treatment of osteoporosis due to their ability to reduce bone resorption and lower fracture risk.”
Types of Bisphosphonates Available
Bisphosphonates come in different forms to help manage osteoporosis. These medicines are key in treating and stopping osteoporosis from getting worse. They help lower the chance of fractures.
Oral Bisphosphonates
Oral bisphosphonates are the most used type of bisphosphonate. They include alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva). It’s important to take them correctly. They should be taken first thing in the morning, at least 30 minutes before eating or drinking anything but water.
“Following the right way to take oral bisphosphonates is key,” says a top osteoporosis treatment guide. “Stay upright and only drink plain water for 30 minutes after taking the medicine.”
Intravenous Bisphosphonates
Intravenous bisphosphonates are for those who can’t take oral ones or have stomach problems. Pamidronate, ibandronate, and zoledronic acid (Reclast/Zometa) are given through a vein. This method is done in a doctor’s office and puts the medicine straight into the blood.
Choosing between oral and intravenous bisphosphonates depends on several things. These include what the patient prefers, how well they can handle stomach issues, and the doctor’s advice. Both types are effective in lowering the risk of fractures in people with osteoporosis.
Proper Administration of Oral Bisphosphonates
To get the most out of oral bisphosphonates, patients need to follow certain rules. These drugs, like alendronate, risedronate, and ibandronate, are used to treat osteoporosis.
Morning Timing Requirements
Oral bisphosphonates must be taken first thing in the morning on an empty stomach. This is key because it helps the drug absorb better without food or other meds getting in the way.
Food and Beverage Restrictions
After taking these drugs, wait 30 to 60 minutes before eating or drinking anything else. This ensures the drug is absorbed correctly.
- Avoid eating or drinking anything except plain water.
- Don’t take other medications, vitamins, or supplements.
- Wait at least 30 to 60 minutes before having coffee, juice, or any other beverage.
Posture and Position After Taking
To avoid esophageal irritation, stay upright for at least 30 minutes after taking oral bisphosphonates. Avoid lying down or bending over, as these can cause the drug to go back into the esophagus.
Staying upright is key to avoiding side effects.
Administration Frequency
The frequency of oral bisphosphonates varies. Some are taken daily, while others are taken weekly or monthly.
- Daily: Some medications are prescribed to be taken once a day.
- Weekly: Many patients take oral bisphosphonates once a week.
- Monthly: Some oral bisphosphonates are taken once a month.
By following these guidelines, patients can make their oral bisphosphonate treatment more effective and reduce side effects.
Receiving Intravenous Bisphosphonate Treatments
People with osteoporosis might get help from intravenous bisphosphonate treatments. These are given at a doctor’s office or infusion center. This is good for those who can’t take oral bisphosphonates or if they don’t work well.
Preparing for IV Administration
Before getting intravenous bisphosphonates, tell your doctor about any health issues, allergies, or medicines you’re on. Zoledronic acid, a common one, is given once a year in a 5 mg dose. You might need blood tests to check your kidney function, as these treatments can affect it.
What to Expect During Treatment
During the treatment, you’ll sit or lie down comfortably. It usually takes 15-30 minutes, based on the drug and your situation. It’s important to watch for any bad reactions during the treatment.
Post-Infusion Care and Monitoring
After the treatment, you’ll be watched for a bit to see if you have any side effects. It’s key to follow what your doctor says about aftercare. This might include drinking lots of water and handling side effects like flu-like symptoms or reactions at the injection site.
Frequency of IV Treatments
How often you get intravenous bisphosphonate treatments depends on the drug and your health. For example, zoledronic acid is given once a year. Treatment usually lasts 3–5 years, based on how you respond and your risk factors.
Managing Possible Side Effects and Complications
It’s important for patients with osteoporosis to know about bisphosphonate side effects. These drugs are effective but can cause various side effects, from mild to severe.
Common Side Effects
Oral bisphosphonates can lead to side effects like muscle cramps/pain, difficulty swallowing, heartburn, abdominal pain, headache, and rash. These issues can affect how well you live.
To lessen these problems, patients are told to stay upright and not eat or drink for at least 30 minutes after taking the drug.
Rare but Serious Complications
A serious issue with bisphosphonates is osteonecrosis of the jaw (ONJ). This is when the jawbone starts to break down. To lower this risk, a dental check-up is advised before starting treatment.
Drug Interactions and Contraindications
Bisphosphonates can interact with other drugs, like calcium supplements, antacids, and certain antibiotics. This can change how well they work. It’s key to tell your doctor about all the medicines and supplements you’re taking.
|
Medication/Supplement |
Potential Interaction |
|---|---|
|
Calcium Supplements |
Reduces bisphosphonate absorption |
|
Antacids |
Interferes with bisphosphonate absorption |
|
Certain Antibiotics |
May increase risk of gastrointestinal side effects |
When to Contact Your Healthcare Provider
If you’re on bisphosphonates and notice severe or ongoing side effects, signs of ONJ (like jaw pain or swelling), or any odd symptoms, reach out to your doctor. Regular check-ups are vital to track how well the treatment is working and to handle any side effects.
Knowing about possible side effects and taking steps to prevent them can help patients safely use bisphosphonates for osteoporosis.
Duration and Monitoring of Bisphosphonate Treatment
Bisphosphonate treatment for osteoporosis needs a personal touch. It aims to get the most benefits while avoiding risks.
Recommended Treatment Timeframes
Most doctors suggest bisphosphonate treatment for 3 to 5 years. But, the right time can change based on many factors. These include how severe the osteoporosis is and if there are fractures.
Key considerations for determining treatment duration include:
- Patient’s age and overall health
- Severity of osteoporosis
- Presence of vertebral or other fractures
- Response to treatment
Drug Holidays: When and Why
A “drug holiday” means stopping bisphosphonate treatment for a while. It’s a way to reduce long-term side effects while keeping some benefits.
Guidelines suggest a drug holiday after 3 to 5 years of treatment. This is for those at lower risk of fractures. The decision depends on the patient’s fracture risk and health.
“The decision to stop or continue bisphosphonate therapy should be made on an individual basis, taking into account the patient’s risk factors and response to treatment.” – American Association of Clinical Endocrinologists
Monitoring Bone Density and Treatment Response
It’s important to check bone density regularly during treatment. This is usually done with Dual-Energy X-ray Absorptiometry (DXA) scans.
Key aspects of monitoring include:
- Assessing changes in bone mineral density (BMD)
- Evaluating the occurrence of new fractures
- Adjusting treatment plans as necessary
Laboratory Tests During Treatment
Laboratory tests are key to checking if bisphosphonate treatment is safe and working. They look at kidney function, calcium levels, and bone turnover markers.
These tests help doctors spot problems early. They make it easier to decide on treatment.
Complementary Approaches to Support Bisphosphonate Therapy
To get the most out of bisphosphonate therapy, it’s key to add other ways to help bones. Bisphosphonates are a big part of treating osteoporosis. But, mixing them with other methods can make treatment work better.
Calcium and Vitamin D Supplementation
Eating well with lots of calcium and vitamin D is important for strong bones. Calcium supplements give your body what it needs for bones. Vitamin D helps your body use calcium. Always take the supplements your doctor tells you to, to help your bisphosphonate therapy.
“Adequate calcium and vitamin D intake is essential for maintaining bone health, particulary in patients undergoing bisphosphonate therapy.”Nutrition and Bone Health Guidelines
Weight-Bearing Exercise and Physical Activity
Weight-bearing exercise is a big part of managing osteoporosis. Walking, running, and lifting weights can make bones stronger and lower fracture risk. Being active also makes you feel better overall.
Fall Prevention Strategies
Stopping falls is key to avoiding fractures, which is very important for people with osteoporosis. Simple steps like clearing tripping hazards, better lighting, and using handrails can help a lot. Also, exercises that boost balance and strength can prevent falls.
- Remove tripping hazards from your home
- Improve lighting in hallways and stairways
- Use handrails on stairs
- Engage in balance-improving exercises
Lifestyle Modifications
Changing your lifestyle can also help with bisphosphonate therapy. Quit smoking, drink less alcohol, and keep a healthy weight. Eating right and staying active are also key to a healthy life.
By adding these extra steps to your treatment, you can make bisphosphonate therapy work better. This will help improve your bone health a lot.
Conclusion
Managing osteoporosis with bisphosphonate treatment needs a full plan. It’s important to give the treatment right and keep an eye on how it’s working. This treatment can really cut down the chance of breaking bones.
Bisphosphonates help slow down bone loss and lower fracture risk. Whether to take them by mouth or through an IV depends on what’s best for each patient.
Other steps are also key in fighting osteoporosis. Taking calcium and vitamin D, doing exercises that make bones stronger, and avoiding falls are all important. They help make the treatment work better.
Healthcare teams can make treatment plans that really help patients. They know about the different bisphosphonates, how to use them, and the side effects. They also know about other ways to help. This way, they can make a plan that really helps each patient. This approach can make a big difference in how well patients do and how happy they are with their life.
FAQ
What is osteoporosis and how is it treated?
Osteoporosis makes bones weak, leading to more fractures. Bisphosphonates are a key treatment. They help lower fracture risk.
How do bisphosphonates work in treating osteoporosis?
Bisphosphonates stop bone breakdown. This increases bone density and lowers fracture risk.
What are the different types of bisphosphonates available for osteoporosis treatment?
There are oral and intravenous bisphosphonates. Examples include alendronate, risedronate, ibandronate, and zoledronic acid.
How should oral bisphosphonates be taken?
Take oral bisphosphonates in the morning. Do it on an empty stomach with a full glass of water. Stay upright for 30 minutes after.
What are the possible side effects of bisphosphonate treatment?
Side effects can include stomach issues. Rare but serious problems are jaw osteonecrosis and atypical femoral fractures.
How long should bisphosphonate treatment be continued?
Treatment usually lasts 3 to 5 years. Sometimes, a break from treatment is recommended after this time.
What is a drug holiday in bisphosphonate treatment?
A drug holiday is a temporary stop in treatment. It’s usually after 3 to 5 years to avoid long-term side effects.
Can osteoporosis be cured with bisphosphonate treatment?
Bisphosphonates can manage osteoporosis and reduce fracture risk. But, they don’t cure it.
What complementary approaches can support bisphosphonate therapy?
Calcium and vitamin D supplements, exercise, fall prevention, and lifestyle changes help with treatment.
How is treatment response monitored during bisphosphonate therapy?
Bone density tests and lab tests like serum CTX or bone-specific alkaline phosphatase monitor treatment success.
Is there a cure for osteoporosis?
There’s no cure for osteoporosis yet. But, treatments like bisphosphonates can manage it and reduce fracture risk.
Can osteoporosis be treated with other medications beside bisphosphonates?
Yes, other drugs like denosumab, teriparatide, and raloxifene are used. They might be for specific patients or with bisphosphonates.
References
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMcp1513724









