Last Updated on November 27, 2025 by Ugurkan Demir

Choosing the right sleep apnea surgery is key for effective treatment. Obstructive sleep apnea can really affect your daily life. It can cause symptoms like snoring, morning headaches, and feeling irritable.
At places like Liv Hospital, we focus on new solutions for those who can’t handle simpler treatments. Surgery for obstructive sleep apnea has improved a lot. Now, there are many sleep apnea procedures that work well, with success rates over 80% in some cases.
How to choose the best sleep apnea procedure, considering success rates and recovery time for various surgeries.
Key Takeaways
- There are many surgical ways to treat obstructive sleep apnea.
- It’s important to know about each procedure to make a good choice.
- Sleep apnea surgery offers different options based on your body and health.
- Places like Liv Hospital look for new ways to help you effectively.
- Success rates for sleep apnea surgery can be over 80% in some cases.
Understanding Sleep Apnea and Its Impact

Sleep apnea is a condition where breathing stops during sleep. It has different types and serious health effects. Knowing about these helps find the best treatment.
Types of Sleep Apnea: Obstructive, Central, and Mixed
Sleep apnea is divided into three types: Obstructive Sleep Apnea (OSA), Central Sleep Apnea (CSA), and Mixed Sleep Apnea. Obstructive Sleep Apnea happens when the airway blocks during sleep. This is often due to relaxed throat muscles or obesity. Central Sleep Apnea is caused by brain problems that affect breathing muscles. Mixed Sleep Apnea is a mix of OSA and CSA.
- Obstructive Sleep Apnea (OSA): The most common, often linked to snoring and airway blockage.
- Central Sleep Apnea (CSA): Less common, linked to brain issues affecting breathing.
- Mixed Sleep Apnea: A mix of OSA and CSA, making diagnosis and treatment complex.
Health Consequences of Untreated Sleep Apnea
Untreated sleep apnea can cause serious health problems. These include cardiovascular disease, stroke, and diabetes. The pauses in sleep and low oxygen levels can harm the heart and increase blood pressure.
- Increased risk of heart attack and stroke from chronic oxygen lack and inflammation.
- Worsening of hypertension, leading to heart disease.
- Changes in metabolism, like insulin resistance, raising the risk of type 2 diabetes.
Prevalence Statistics and High-Risk Demographics
Obstructive sleep apnea affects 2-4% of middle-aged adults in the United States. It’s more common in older adults, males, and those with obesity. Knowing this helps find who might need surgery.
Demographic | Prevalence of Sleep Apnea |
Middle-aged adults | 2-4% |
Older adults | Higher than 4% |
Males | Higher prevalence compared to females |
When Conservative Treatments Fail

If treatments like CPAP therapy and oral appliances don’t work, it’s time to look at other options. Many people keep having trouble sleeping, even with these treatments.
CPAP Compliance Challenges
CPAP therapy is a top choice for sleep apnea. But, some people find it hard to use because of discomfort or feeling trapped. Studies show up to 50% of users struggle to stick with CPAP, showing the need for other ways to help.
Limitations of Oral Appliances
Oral appliances can help with mild to moderate sleep apnea. But, they might not work for everyone, like those with severe apnea or dental issues. How well they work depends on the apnea’s severity and the person’s body.
Lifestyle Modifications and Their Effectiveness
Changing your lifestyle, like losing weight or exercising, can help with sleep apnea. Weight loss, in particular, can lessen sleep apnea in obese people. Yet, these changes might not be enough for everyone, mainly those with severe apnea.
If these methods don’t work, surgery could be an option. It’s important to understand the issues with CPAP, the limits of oral appliances, and how lifestyle changes can help. This helps find the best treatment plan.
Determining Surgical Candidacy
The journey to sleep apnea surgery starts with checking if you’re a good candidate. This step is key to finding out who can really benefit from surgery.
Required Diagnostic Testing
We use detailed tests to figure out if surgery is right for you. Sleep studies show how bad sleep apnea is and where it’s happening. Sleep studies, like polysomnography, tell us how often and long apneic events last.
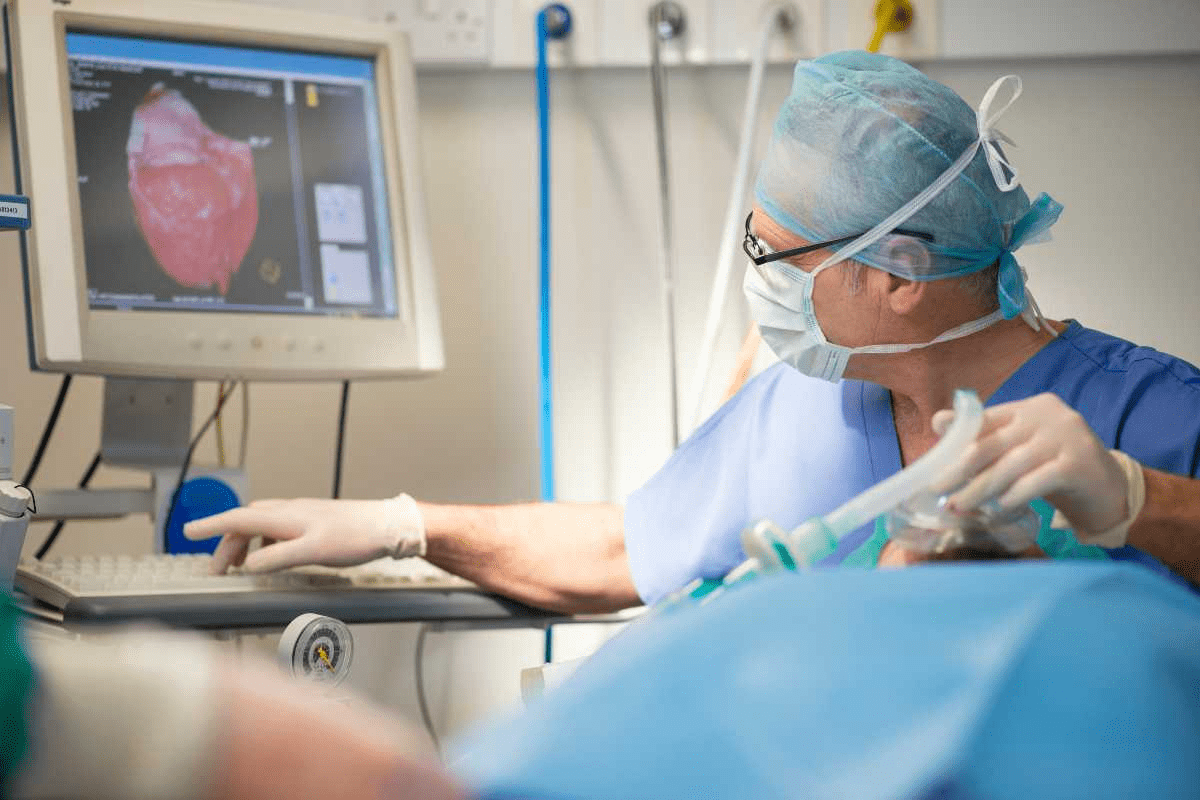
Imaging tests like CT scans or MRI look at your airway. They help spot any problems that might be causing sleep apnea.
Medical Clearance Considerations
Getting medical clearance is also very important. We check your health to make sure surgery is safe for you. This means looking at any health issues you already have, like high blood pressure or diabetes, and how they might affect surgery risks.
If you have serious health problems, we might need to check them more closely before surgery. We want to make sure surgery is as safe as possible for you.
Age and Health Factors
Age and health are also big factors. While age itself isn’t a reason not to have surgery, older people might need more checks. This is because they might have other health issues.
For example, surgeries like Uvulopalatopharyngoplasty (UPPP) can work well for some people. Success rates are around 40-70%, mainly for those with mild to moderate sleep apnea. We decide on surgery based on your health and how it might help you.
Common Sleep Apnea Procedure Options
Sleep apnea surgery has many options, based on how severe and where the blockage is. We’ll look at the different surgeries, how they match up with blockage sites, and the difference between first and second tries.
Overview of Surgical Approaches
Sleep apnea surgery aims to improve airflow in the upper airway. This reduces apneic events. Maxillomandibular advancement (MMA) surgery is very effective, with success rates of 80-90%. Other methods include uvulopalatopharyngoplasty (UPPP), hypoglossal nerve stimulation, and tissue reduction.
Matching Procedures to Obstruction Sites
The right surgery depends on where the blockage is. Tests like sleep endoscopy pinpoint the problem area. For example, UPPP is good for the palate. More complex cases might need MMA.
Procedure | Site of Obstruction | Success Rate |
UPPP | Palate | 40-50% |
MMA | Multiple sites | 80-90% |
Hypoglossal Nerve Stimulation | Tongue base | 60-70% |
First-line vs. Secondary Interventions
Sleep apnea surgeries are divided into first-line and secondary treatments. First-line interventions are less invasive, like UPPP or palatal implants. Secondary interventions, such as MMA or hypoglossal nerve stimulation, are for those who didn’t get better with the first try.
Knowing the different surgeries and how they fit the blockage helps us tailor treatments. This gives patients with sleep apnea the best chance at success.
Tissue Reduction Surgical Techniques
Tissue reduction surgeries are key for those with sleep apnea who haven’t seen improvement with other treatments. These surgeries aim to lessen or reshape tissue in the upper airway. This helps improve airflow and reduce symptoms.
Uvulopalatopharyngoplasty (UPPP)
Uvulopalatopharyngoplasty, or UPPP, is a common surgery. It removes or reshapes parts of the uvula, soft palate, and tonsils. This method aims to widen the airway and lessen blockages. Studies show UPPP can help reduce sleep apnea severity in some patients.
Laser-Assisted Uvulopalatoplasty (LAUP)
Laser-Assisted Uvulopalatoplasty, or LAUP, uses a laser to reshape the uvula and soft palate. It’s done in several outpatient procedures, making it less invasive for some. Yet, its success can vary, and it might not work for everyone.
Radiofrequency Tissue Ablation
Radiofrequency tissue ablation is a minimally invasive method. It uses radiofrequency energy to reduce tissue in the upper airway. This technique treats obstructions at different levels, like the tongue base and palate. It’s often chosen for its minimal discomfort and quick recovery.
Advances in surgery are improving outcomes for sleep apnea patients. For example, hypoglossal nerve stimulation has shown over 80% success rates. It can be done on an outpatient basis, making it a promising option or addition to tissue reduction surgeries.
The right tissue reduction technique depends on several factors. These include the obstruction site, sleep apnea severity, and the patient’s health. A detailed evaluation by a sleep specialist is essential to choose the best surgical approach.
Key Considerations:
- The site and severity of airway obstruction
- Patient’s overall health and medical history
- Potential risks and benefits of each procedure
- Expected outcomes and recovery times
Understanding the various tissue reduction surgical techniques helps patients make informed decisions. This way, they can work towards better sleep quality.
Skeletal Procedures for Severe Cases
In severe sleep apnea cases, surgery on the skeletal structure can help. These surgeries aim to move or stabilize the jaw and nearby bones. This improves the airway’s openness.
Maxillomandibular Advancement (MMA)
MMA is a surgery that moves the upper and lower jaw forward. This makes the airway bigger. It has been shown to greatly lessen sleep apnea by enlarging the upper airway.
This surgery moves the jaw. MMA tackles the main cause of sleep apnea. It brings relief to those with severe cases.
Genioglossus Advancement
Genioglossus advancement is a surgery for sleep apnea. It moves the genioglossus muscle forward. This muscle is key for tongue movement.
By moving this muscle, the surgery stops the tongue from blocking the airway at night. It cuts down on apnea episodes.
Hyoid Suspension
Hyoid suspension is a surgery that keeps the hyoid bone in place. The hyoid bone is in the neck. It prevents it from blocking the airway.
This surgery is often paired with MMA. Together, they make the airway more stable. This improves sleep quality.
These skeletal surgeries offer hope for those with severe sleep apnea. They haven’t seen results from other treatments. Knowing about these surgeries helps patients make better choices for their care.
Innovative Nerve Stimulation Approaches
New nerve stimulation methods are showing promise for sleep apnea treatment. These advancements give hope to those who haven’t found relief with traditional treatments.
Hypoglossal Nerve Stimulation Technology
Hypoglossal nerve stimulation uses a device to control the tongue nerve. This keeps the airway open during sleep. Studies show it can reduce sleep apnea by over 80%.
The device is implanted to detect breathing and stimulate the tongue nerve. This helps keep the airway open. It’s great for those with moderate to severe sleep apnea.
Patient Selection Criteria
Choosing the right patients for this treatment is key. They usually have:
- Moderate to severe obstructive sleep apnea
- Can’t tolerate CPAP therapy
- Specific body features that fit the implant
They need thorough evaluations, including sleep studies and body checks, to see if they qualify.
Advantages of Outpatient Application
Hypoglossal nerve stimulation is often done as an outpatient procedure. This means less hospital time, making it easier for patients.
Being an outpatient also means quicker recovery. Patients can get back to their daily life faster. But, they must follow post-op instructions carefully for the best results.
Key benefits of hypoglossal nerve stimulation include:
- High success rate in reducing sleep apnea severity
- Minimally invasive procedure
- Outpatient treatment option
- Improved quality of life for patients with moderate to severe sleep apnea
Nasal and Adjunctive Procedures
Nasal and adjunctive procedures are key in treating sleep apnea. They address specific issues that can cause sleep apnea. This makes the treatment plan more effective.
Septoplasty and Turbinate Reduction
Nasal obstructions are common in sleep apnea patients. Septoplasty and turbinate reduction help improve breathing. They correct nasal septum deviations and reduce turbinate bone size.
Septoplasty straightens the nasal septum, which can be deviated. Turbinate reduction makes the turbinate bones smaller. Together, they help patients breathe better during sleep.
Palatal Implants and Stiffening Techniques
Palatal implants and stiffening techniques stabilize the soft palate. Palatal implants stiffen the soft palate with small implants. Stiffening techniques, like palatal stiffening, use materials or methods to stiffen it.
These methods are great for patients with severe palatal obstruction. They help reduce sleep apnea symptoms and improve sleep quality.
Tonsillectomy and Adenoidectomy
Tonsillectomy and adenoidectomy remove tonsils and adenoids. These surgeries are often done together, mainly in kids, to treat sleep apnea.
In adults, tonsillectomy can help if large tonsils block the airway. Removing tonsils and adenoids can improve airflow and reduce sleep apnea symptoms.
Combination Approaches
Combining nasal and adjunctive procedures often leads to better results. For example, a patient might have septoplasty, turbinate reduction, and tonsillectomy at the same time. This addresses multiple obstruction sites.
Procedure | Purpose | Benefits |
Septoplasty | Corrects nasal septum deviation | Improves nasal airflow |
Turbinate Reduction | Reduces turbinate bone size | Enhances nasal breathing |
Palatal Implants | Stiffens the soft palate | Reduces palatal obstruction |
Tonsillectomy/Adenoidectomy | Removes tonsils and adenoids | Eliminates tonsillar obstruction |
Understanding nasal and adjunctive procedures helps us tailor treatments. This improves outcomes and enhances quality of life for patients.
Preparing for Sleep Apnea Surgery
Thinking about sleep apnea surgery? It’s key to know the prep steps for a smooth process. We’ll walk you through what to do, easing your worries and aiming for the best results.
Preoperative Testing Requirements
Before surgery, we need to check your health with some tests. These might include blood work, heart tests, and sleep studies. We team up with your doctor to get all the info we need.
Preoperative testing is key to spot any health issues that could impact your surgery or healing. We use this info to make sure we’re focusing on what’s best for you, keeping risks low and outcomes high.
Medication Adjustments
Some meds can affect your surgery or recovery. We’ll review your meds and make changes if needed. This might mean stopping or changing meds that could raise bleeding risks or interact with anesthesia.
Telling us about all your meds, including supplements and over-the-counter drugs, is vital for your safety. We’ll give you clear directions on managing your meds before and after surgery.
Setting Realistic Expectations
Knowing what to expect from your surgery is important. We’ll talk about the possible benefits and risks, and what to expect during recovery. This includes info on managing pain, post-op care, and follow-up visits.
By setting clear expectations, we help you get ready for recovery and aim for the best results from your surgery.
Hospital vs. Outpatient Settings
The place of your surgery depends on your procedure’s complexity and your health. We’ll go over the pros and cons of hospital and outpatient settings with you. This way, you can choose what’s best for you.
Whether you have surgery in a hospital or an outpatient setting, our team is dedicated to giving you top-notch care and support every step of the way.
Recovery and Post-Operative Care
Understanding the recovery process is key for a smooth surgery outcome. Each person’s recovery is unique. We aim to guide you through the post-operative period.
Procedure-Specific Recovery Timelines
Recovery times vary based on the surgery type. For example:
- Tissue reduction surgeries, like uvulopalatopharyngoplasty (UPPP), need more time, often weeks for full recovery.
- Skeletal procedures, such as maxillomandibular advancement (MMA), may require a longer hospital stay and recovery that can last months.
- Nerve stimulation approaches, like hypoglossal nerve stimulation, usually have a quicker recovery, allowing for normal activities in a few weeks.
Pain Management Strategies
Managing pain is key for a comfortable recovery. We use several methods, including:
- Medication: A mix of pain relievers to manage discomfort.
- Cold compresses: To reduce swelling and ease pain.
- Rest: Enough rest is vital for healing.
- Soft diet: Eating soft foods can help during the initial recovery phase.
Potential Complications and Warning Signs
While surgery is generally safe, complications can occur. Be aware of:
- Infection: Signs include fever, increased pain, or swelling.
- Bleeding: Excessive bleeding or trouble controlling it.
- Swelling: Severe swelling that affects breathing or causes discomfort.
- Changes in speech or swallowing: Persistent difficulty speaking or swallowing.
It’s important to watch for these signs and seek medical help if they appear.
Follow-up Sleep Studies
After recovery, follow-up sleep studies are vital. They help us see:
- The decrease in sleep apnea events.
- Improvement in sleep quality.
- Any remaining sleep apnea that might need more treatment.
By monitoring surgery outcomes, we can adjust care for the best results.
Conclusion
We’ve looked into sleep apnea surgery, a good option for those who haven’t found relief with other treatments. It’s important to know about the different surgeries and when they’re used.
Sleep apnea surgery includes many procedures to help with obstructive sleep apnea. Knowing about these options, how well they work, and what recovery is like helps patients make better choices.
At our place, we aim to give top-notch care to everyone, including international patients. Our team works hard to give each patient the right treatment for their needs.
In short, sleep apnea surgery is a hopeful solution for those tired of sleep apnea. We suggest talking to our experts to find the best treatment. This is the first step to better sleep.
FAQ
What is sleep apnea surgery?
Sleep apnea surgery is a set of procedures to treat obstructive sleep apnea. These include reducing tissue, moving the jaw, and using nerve stimulation.
Is there a surgery for sleep apnea?
Yes, there are several surgeries for sleep apnea. Each has its own use and success rate.
What are the different types of sleep apnea surgery?
There are many types of sleep apnea surgery. These include reducing tissue, moving bones, and using nerve stimulation.
How is a patient determined to be a suitable candidate for sleep apnea surgery?
To see if you’re a good candidate, you’ll need a detailed check-up. This includes tests to see how bad your sleep apnea is and if you’re healthy enough for surgery.
What is the success rate of sleep apnea surgery?
The success of sleep apnea surgery varies. It depends on the type of surgery and your specific situation. Some surgeries work better than others.
What is hypoglossal nerve stimulation, and how does it work?
Hypoglossal nerve stimulation is a new way to treat sleep apnea. It uses the hypoglossal nerve to move the tongue and keep the airway open.
What are the benefits of outpatient sleep apnea surgery?
Outpatient surgery for sleep apnea has many benefits. You get to go home sooner and avoid the hassle of a hospital stay.
How do I prepare for sleep apnea surgery?
Preparing for surgery involves several steps. You’ll need to have tests done, adjust your medications, and know what to expect after surgery.
What is the recovery process like after sleep apnea surgery?
Recovery after surgery varies. You might feel some pain, swelling, and need to rest a bit. But it’s different for everyone.
Are there any potentially dangerous complications or warning signs to watch out for after sleep apnea surgery?
Yes, watch out for signs like trouble breathing, severe pain, or infection. If you notice these, get medical help right away.
How is the effectiveness of sleep apnea surgery assessed?
Doctors check how well surgery worked with follow-up sleep studies. These studies show if the surgery helped reduce sleep apnea.
Can sleep apnea surgery be combined with other treatments?
Yes, surgery can be used with other treatments. This can help treat sleep apnea more effectively.
What are the risks associated with sleep apnea surgery?
Sleep apnea surgery, like any surgery, has risks. These include infection, bleeding, and problems with anesthesia.
Is sleep apnea surgery a permanent solution?
Sleep apnea surgery can be very effective. But, it’s not always permanent. Some people might need more treatment or help later on.
References
National Center for Biotechnology Information. (2025). How to Choose Sleep Apnea Surgery Options Choosing. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11476387/