Last Updated on November 4, 2025 by mcelik

Did you know that nearly 250,000 adults in the United States are diagnosed with spinal stenosis each year? This condition makes the spinal canal narrower. It can cause pain, numbness, and weakness in the back and legs. But can it also cause headaches?Learn if Spinal Stenosis Symptoms can cause headaches and how nerve compression affects the neck.
Understanding the connection between spinal stenosis and headaches is crucial for those affected by this condition. As we look into the symptoms and effects of spinal stenosis, we see it affects more than just the back and legs. It can also impact other health areas, like headaches.
Key Takeaways
- Spinal stenosis is a condition characterized by the narrowing of the spinal canal.
- Symptoms of spinal stenosis include pain, numbness, and weakness in the back and legs.
- There is a possible link between spinal stenosis and headaches.
- Knowing the symptoms of spinal stenosis is important for managing and treating it.
- Spinal stenosis affects nearly 250,000 adults in the United States each year.
Understanding Spinal Stenosis: Definition and Overview
Spinal stenosis is when the spinal canal gets narrower. This can press on nerves in the spine, causing symptoms.
What Is Spinal Stenosis?
Spinal stenosis means the spaces in the spine get smaller. This can squeeze nerves. It often happens in the lower back (lumbar spine) and neck (cervical spine).
It can be caused by aging, injuries, or certain diseases.
How Common Is Spinal Stenosis?
Spinal stenosis is common, mainly in older people. Studies show it affects many over 50. Knowing this helps doctors diagnose and treat it.
The Anatomy of the Spine
The spine, or backbone, is complex. It has vertebrae, discs, and nerves. It supports the body and protects the spinal cord.
The spinal canal, made by vertebrae, holds the spinal cord and nerves. Knowing the spine’s anatomy helps understand spinal stenosis and its effects.
The spine has different parts: the cervical (neck), thoracic (upper back), and lumbar (lower back) spines. Each part has its role and can face different issues. Spinal stenosis can happen anywhere, causing various symptoms based on where and how much it narrows.
Types of Spinal Stenosis
It’s important to know about the different types of spinal stenosis. Each type affects a different part of the spine. This knowledge helps doctors diagnose and treat the condition better.
Cervical Spinal Stenosis
Cervical spinal stenosis happens when the neck’s spinal canal gets smaller. This can press on the spinal cord. Symptoms include neck pain, arm numbness, and trouble walking.
Cervical stenosis is serious because it can harm the spinal cord. If not treated, it can cause severe problems.
Lumbar Spinal Stenosis
Lumbar stenosis affects the lower back’s spinal canal. It can cause leg pain, numbness, or weakness. Walking can also lead to cramping or tiredness.
Lumbar spinal stenosis is the most common type. It often comes from wear and tear on the spine.
Thoracic Spinal Stenosis
Thoracic spinal stenosis is rarer and affects the middle spine. It can cause pain, numbness, or weakness in the chest or legs. Finding this type can be hard because it’s not common.
Doctors use tests and imaging to diagnose thoracic spinal stenosis.
| Type of Spinal Stenosis | Region Affected | Common Symptoms |
| Cervical Spinal Stenosis | Neck Region | Neck pain, numbness or tingling in arms, difficulty walking |
| Lumbar Spinal Stenosis | Lower Back | Pain, numbness, or weakness in legs, cramping or fatigue when walking |
| Thoracic Spinal Stenosis | Middle Portion of Spine | Pain, numbness, or weakness in chest or legs |
Common Spinal Stenosis Symptoms and Warning Signs

It’s important to know the symptoms of spinal stenosis early. This condition narrows the spinal canal, causing various symptoms. These symptoms can affect your daily life and quality of life.
Neck and Back Pain
Neck or back pain is a common symptom of spinal stenosis. Cervical spinal stenosis can cause neck pain that may spread to the shoulders or arms. Lumbar spinal stenosis leads to lower back pain and leg pain.
Key characteristics of neck and back pain associated with spinal stenosis include:
- Pain that worsens with certain activities, such as standing or walking
- Pain that improves with rest or specific postures, like sitting or bending forward
- Sharp or dull pain that can radiate to other areas, such as the arms or legs
Numbness and Tingling
Numbness and tingling are common symptoms due to nerve compression. These feelings can happen in the neck, back, arms, or legs. For example, cervical spinal stenosis can cause numbness in the hands or fingers. Lumbar stenosis might cause similar feelings in the feet or toes.
Numbness and tingling can be intermittent or constant and may be accompanied by other sensations, such as:
- Burning or prickling sensations
- Weakness in the affected limbs
- Difficulty controlling the bladder or bowels in severe cases
Muscle Weakness
Muscle weakness is a significant symptom of spinal stenosis. It can affect the arms, legs, or hands, making daily tasks hard. For instance, lumbar spinal stenosis can cause leg weakness, making it hard to stand or walk.
Walking Problems and Balance Issues
Walking problems and balance issues are common in lumbar spinal stenosis. The condition can cause pain, numbness, or weakness in the legs. This makes it hard to maintain balance or walk long distances. In severe cases, it can lead to neurogenic claudication, where pain or weakness in the legs worsens with walking and improves with rest.
Strategies to manage walking problems include:
- Physical therapy to improve strength and flexibility
- Using assistive devices, such as canes or walkers, for support
- Modifying activities to avoid exacerbating symptoms
Recognizing these symptoms early is key to managing spinal stenosis effectively. If you’re experiencing any of these warning signs, it’s important to see a healthcare professional for a proper diagnosis and treatment plan.
The Connection Between Spinal Stenosis and Headaches

Many people with spinal stenosis, like cervical stenosis, often get headaches. The narrowing of the spinal canal in the neck can cause these symptoms.
How Cervical Stenosis Affects the Head
Cervical stenosis happens when the neck’s spinal canal gets smaller. This puts pressure on the spinal cord. This pressure can cause neck pain, numbness, and tingling in the arms. It can also lead to headaches because the nerves send pain signals to the brain.
The mechanisms by which cervical stenosis causes headaches are quite complex, involving nerve compression and pain signal transmission to the brain. It involves nerves getting compressed and sending pain signals to the brain. These signals are what the brain interprets as headache pain.
Nerve Compression and Referred Pain
Nerve compression is a big reason for headaches in cervical stenosis. When nerves in the neck are squished, they can send pain signals to other areas, like the head. This is called referred pain.
“The pain from cervical stenosis can be referred to the head, leading to headaches. Understanding the source of the pain is key for effective treatment.”
Referred pain happens because nerves in the neck are connected to nerves in the head and face. When these nerves get compressed, pain can be felt in places other than the neck.
Research Evidence on the Connection
Studies have shown a link between cervical stenosis and headaches. They found that people with severe cervical stenosis are more likely to have headaches.
This research shows that treating cervical stenosis can help with headaches. It’s important to get a proper diagnosis and treatment.
Types of Headaches Associated with Spinal Stenosis
Headaches linked to spinal stenosis can be different, like cervicogenic, tension, and occipital neuralgia. Knowing these types is key for the right diagnosis and treatment.
Cervicogenic Headaches
Cervicogenic headaches start in the neck and move to the head. They get worse with certain neck movements or positions.
- Characteristics: Pain usually starts in the neck and spreads to the head, often on one side.
- Triggers: Sustained neck positions, neck movements, or pressure on the neck.
Tension Headaches
Tension headaches are common with spinal stenosis. They feel like a band or squeezing around the forehead.
Key Features:
- Dull, aching pain on both sides of the head.
- Tightness or pressure in the neck and scalp.
Occipital Neuralgia
Occipital neuralgia causes sharp, stabbing pain in the neck and back of the head. It’s due to irritated occipital nerves.
- Symptoms: Sudden, severe pain on one side of the head, often described as stabbing or shooting.
- Causes: Compression or irritation of the occipital nerves, sometimes related to spinal stenosis.
It’s important to know the specific headache type for proper treatment. Each headache type has its own signs and needs different treatments.
Causes and Risk Factors of Spinal Stenosis
As we age, our spines change, sometimes leading to spinal stenosis. This is when the spinal canal gets narrower. Knowing what causes and increases the risk of spinal stenosis is key to managing it well.
Age-Related Changes
Age is a big risk factor for spinal stenosis. As we get older, our spines naturally change, narrowing the spinal canal. Degenerative changes like bone spurs and thickened ligaments can press on nerves, causing symptoms.
Genetic Factors
Genetics also play a part in spinal stenosis. If your family has a history of spinal issues, you might be more likely to get it. Studies show that genetics can affect how the spine degenerates, possibly leading to spinal stenosis.
Injuries and Trauma
Spinal injuries and trauma can also cause spinal stenosis. Traumatic injuries like fractures or dislocations can immediately narrow the spinal canal. Such injuries can also speed up degenerative changes, raising the risk of spinal stenosis over time.
Other Medical Conditions
Some medical conditions can make you more likely to get spinal stenosis. For example, people with osteoarthritis or spondylolisthesis are at higher risk due to the degenerative changes these conditions bring. Other factors like being overweight or not being active can also increase the risk.
Knowing the causes and risk factors of spinal stenosis is vital for effective treatment. By tackling these factors, healthcare providers can help manage symptoms and improve life quality for those with spinal stenosis.
Diagnosing Spinal Stenosis and Related Headaches
Diagnosing spinal stenosis is a detailed process. It includes physical exams, imaging tests, and neurological checks. This thorough approach helps spot spinal stenosis and its effects, like headaches.
Physical Examination
A physical exam is the first step in diagnosing spinal stenosis. Doctors check muscle strength, reflexes, and touch sensitivity. They also look at how spinal stenosis affects movement and balance, which can lead to headaches.
Key components of a physical examination include:
- Assessing muscle strength and reflexes
- Evaluating sensitivity to touch and pain
- Observing posture and gait
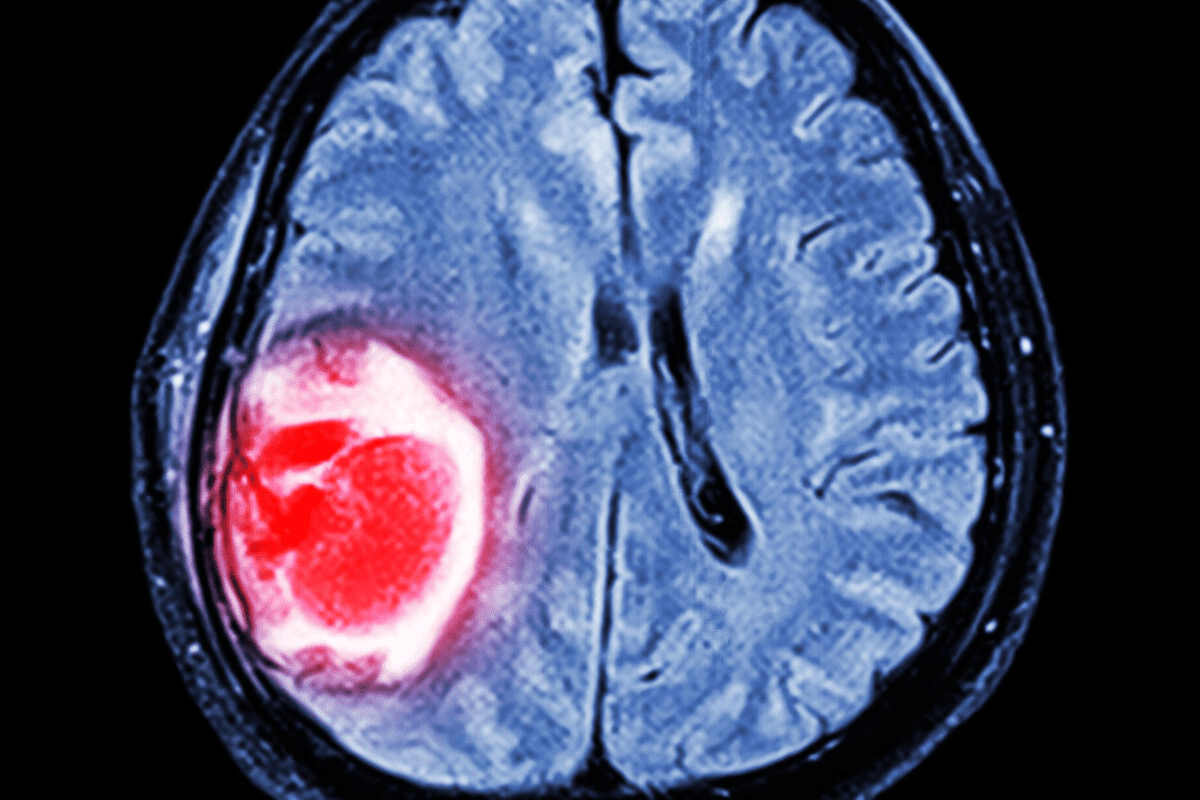
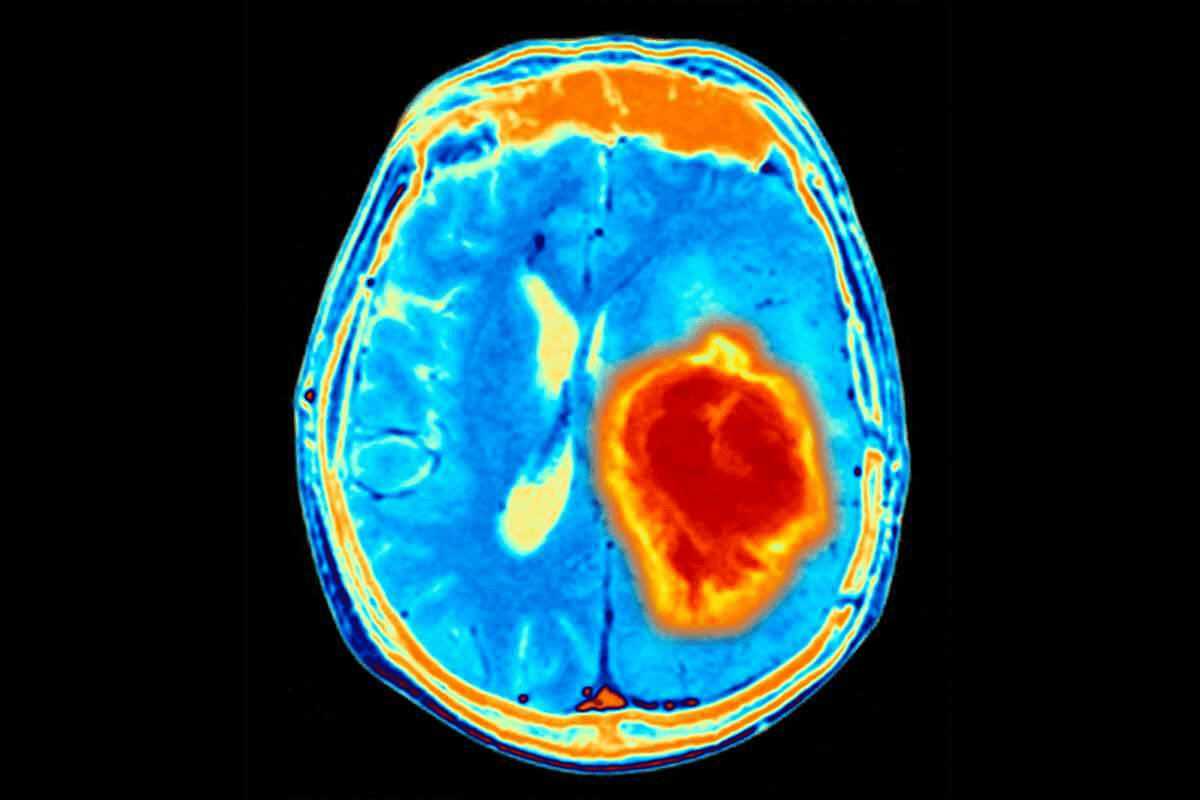
Imaging Tests
Imaging tests are key to confirming spinal stenosis. They show detailed images of the spine. This helps doctors spot narrowing and compression areas.
Common imaging tests used include:
- X-rays: Provide initial images of the spine’s structure
- MRI (Magnetic Resonance Imaging): Offers detailed images of soft tissues, nerves, and the spinal cord
- CT (Computed Tomography) scans: Provides detailed images of the spine’s bony structures
| Imaging Test | Primary Use | Benefits |
| X-rays | Initial assessment of spinal structure | Quick, widely available |
| MRI | Detailed imaging of soft tissues and nerves | High resolution, detailed nerve imaging |
| CT scans | Detailed imaging of bony structures | Excellent for bone detail, quick |
Neurological Assessments
Neurological tests are important for understanding spinal stenosis’s effects on the nervous system. They help find nerve damage or compression that might cause symptoms, like headaches.
Components of neurological assessments may include:
- Evaluating nerve function and response
- Assessing cognitive function and memory
- Testing for nerve root irritation
Severity Levels of Spinal Stenosis
It’s important to know how severe spinal stenosis is to choose the right treatment. Spinal stenosis is when the spinal canal gets narrower. This can affect people differently, based on how much it narrows and the symptoms it causes.
Mild Spinal Stenosis
Mild spinal stenosis means the spinal canal is only slightly narrowed. It doesn’t hurt the nerves much. People with mild stenosis might not feel many symptoms. They might not need strong treatments. Monitoring and conservative management are often suggested.
Moderate Spinal Stenosis
Moderate stenosis means the canal is more narrowed. This can cause numbness, tingling, and pain. These symptoms can make everyday tasks hard. Treatment might include physical therapy, pain meds, and epidural injections to reduce swelling.
Severe Spinal Stenosis
Severe stenosis means the canal is very narrowed, causing a lot of nerve pressure. This can lead to severe pain, muscle weakness, and trouble walking or standing. Surgical intervention is often needed to relieve nerve pressure and improve life quality.
Knowing the severity helps doctors create treatment plans that fit each patient. This approach can lead to better results and happier patients.
Non-Surgical Treatment Options for Spinal Stenosis
People with spinal stenosis can find relief through various non-surgical treatments. These help reduce pain and improve life quality. “
Medications for Pain Management
Medicines are key in managing spinal stenosis pain. Over-the-counter drugs like acetaminophen and ibuprofen help with mild to moderate pain. For more severe pain, doctors might prescribe stronger drugs like corticosteroids or muscle relaxants.
Key medications include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids for short-term use to reduce inflammation
- Muscle relaxants to alleviate muscle spasms
Physical Therapy Approaches
Physical therapy is vital in treating spinal stenosis without surgery. A physical therapist creates a custom exercise plan. This plan boosts flexibility, strength, and balance, helping to reduce pain and improve movement.
Lifestyle Modifications
Changing your lifestyle can greatly help manage spinal stenosis. Keeping a healthy weight, doing regular low-impact exercises, and maintaining good posture are key.
Beneficial lifestyle adjustments include:
- Maintaining a healthy weight to reduce pressure on the spine
- Engaging in low-impact activities like walking or swimming
- Improving posture to reduce strain on the spinal column
Alternative Therapies
Some people find relief in alternative therapies like chiropractic care, acupuncture, or massage therapy. These treatments can offer more pain relief and better function, even though the evidence varies.
It’s important for patients to talk to their healthcare provider before trying any new therapy. This ensures it’s right for their condition.
Surgical Interventions for Spinal Stenosis
When other treatments don’t work, surgery is an option for spinal stenosis. It aims to ease pressure on the spinal cord or nerves. This helps reduce pain and improve movement.
Decompression Procedures
Decompression surgery removes structures that press on nerves or the spinal cord. This can include laminectomy, where part or all of the vertebrae (lamina) is taken out. The goal is to give more space for nerves, easing symptoms.
Spinal Fusion
In some cases, spinal fusion is done with decompression. This joins two or more vertebrae together using bone grafts, rods, or screws. It stabilizes the spine and can reduce pain from abnormal motion.
Minimally Invasive Options
New surgical techniques have led to minimally invasive surgery for spinal stenosis. These use smaller cuts and cause less damage, leading to faster recovery. Methods include microdiscectomy and minimally invasive laminectomy.
Recovery and Rehabilitation
Recovery from spinal stenosis surgery varies. Patients usually need rest and physical therapy to build strength and mobility. A good rehabilitation plan is key for the best results.
It’s important for patients to talk to a healthcare provider. They can help decide the best surgery for their condition.
Managing Headaches Related to Spinal Stenosis
Managing headaches from spinal stenosis needs a mix of pain relief, posture correction, and stress management. Knowing and using these methods can help control headaches and enhance life quality.
Targeted Pain Relief Strategies
Effective pain relief is key for managing spinal stenosis headaches. Several strategies can be used:
- Medications: Over-the-counter pain relievers like acetaminophen or ibuprofen can ease headache symptoms. Sometimes, prescription meds are needed.
- Physical Therapy: Gentle exercises and stretches can lessen tension and improve spinal alignment. This can reduce headache frequency and severity.
- Nerve Blocks: For some, nerve blocks or steroid injections can offer significant relief. They reduce inflammation and pain.
Posture Correction
Good posture is vital for reducing spine strain and easing headache symptoms. Here are some tips for improving posture:
- Ergonomic Adjustments: Make sure workspaces support good posture. Monitors should be at eye level, and chairs should support the lower back.
- Regular Stretching: Adding stretching to daily routines helps keep muscles flexible and reduces tension.
- Strengthening Exercises: Doing exercises that strengthen the core and back muscles supports the spine and improves posture.
Stress Management Techniques
Stress can make headache symptoms worse, so managing stress is key. Techniques include:
- Mindfulness and Meditation: Mindfulness and meditation can lower stress and promote relaxation.
- Deep Breathing Exercises: Deep breathing calms the nervous system and reduces stress.
- Regular Exercise: Regular physical activity can lower stress levels and boost mood.
By using these strategies daily, people with spinal stenosis can manage their headaches better and improve their well-being.
Prevention and Long-Term Outlook
Spinal stenosis can be tough, but there are ways to improve your outlook. Knowing what causes it and taking steps early on can help. This way, you can lower your risk and handle the condition better.
Preventive Measures
To prevent spinal stenosis, make lifestyle changes and stay proactive. Regular exercise, a healthy weight, and good posture help your spine. Also, quitting smoking and managing diabetes are key for your spine’s health.
Prognosis With Treatment
The outlook for spinal stenosis depends on how severe it is and the treatment. Many see big improvements with the right care. Treatments range from physical therapy and pain management to surgery for serious cases.
| Treatment Approach | Benefits | Considerations |
| Physical Therapy | Improves mobility, reduces pain | Requires commitment to regular sessions |
| Pain Management | Reduces discomfort, improves quality of life | May involve medication side effects |
| Surgical Intervention | Can provide significant relief for severe cases | Involves surgical risks and recovery time |
Living With Chronic Spinal Stenosis
Managing chronic spinal stenosis means ongoing care and lifestyle changes. Stay informed and work with your healthcare team. This way, you can create a plan to manage symptoms and keep your quality of life high.
Conclusion
It’s important to know how spinal stenosis and headaches are linked. This article has covered spinal stenosis, its symptoms, and how it can cause headaches.
Spinal stenosis is when the spinal canal gets narrower. This can lead to neck and back pain, numbness, tingling, and muscle weakness. It can also cause headaches, mainly if the neck is affected.
To wrap up, recognizing the signs of spinal stenosis is key. Knowing the causes, risk factors, and treatment options helps manage the condition. This can also help reduce headaches.
FAQ
What is spinal stenosis?
Spinal stenosis is when the spinal canal gets narrower. This can put pressure on the spinal cord and nerves. It leads to various symptoms.
Can spinal stenosis cause headaches?
Yes, it can. Cervical spinal stenosis, in particular, can cause headaches. This is because of nerve compression and referred pain.
What are the common symptoms of spinal stenosis?
Symptoms include neck and back pain. You might also feel numbness and tingling. Muscle weakness, walking problems, and balance issues are common too.
How is spinal stenosis diagnosed?
Doctors use physical exams and imaging tests like MRI or CT scans. They also do neurological assessments. This helps them see how much the nerves are compressed and how narrow the spinal canal is.
What are the treatment options for spinal stenosis?
There are many treatments. Non-surgical options include medications, physical therapy, and lifestyle changes. Surgery, like decompression procedures and spinal fusion, is also an option.
Can spinal stenosis be prevented?
Some risk factors, like age and genetics, can’t be changed. But, a healthy lifestyle, regular exercise, and managing chronic conditions can help prevent it.
What is the prognosis for individuals with spinal stenosis?
With the right treatment and care, many people see big improvements. They can feel better and live a better life.
How does cervical stenosis affect the head?
Cervical stenosis can cause headaches. This is because nerves in the cervical spine get compressed. This can send pain to the head.
What are cervicogenic headaches?
Cervicogenic headaches start in the cervical spine. They are often linked to cervical spinal stenosis or other cervical spine problems.
Can spinal stenosis cause walking problems?
Yes, it can. Lumbar spinal stenosis can make walking hard. It can also affect balance because of nerve compression.
What is the difference between lumbar and cervical spinal stenosis?
Lumbar stenosis affects the lower back. It can cause leg pain and make walking hard. Cervical stenosis affects the neck. It can cause headaches, neck pain, and pain in the upper limbs.
Are there any alternative therapies for managing spinal stenosis symptoms?
Yes, there are. Chiropractic care, acupuncture, and massage therapy might help. But, how well they work can vary for each person.
How does age relate to the development of spinal stenosis?
Age is a big risk factor. Spinal stenosis is more common in older adults. This is because of degenerative changes in the spine.
Can injuries cause spinal stenosis?
Yes, they can. Injuries and trauma to the spine can lead to spinal stenosis. This is true if they cause structural changes or instability in the spine.
What lifestyle modifications can help manage spinal stenosis?
A healthy weight, regular exercise, good posture, and avoiding heavy lifting can help. These can manage symptoms and slow the condition’s progression.
Reference:
- Medical News Today. (2024). Spinal stenosis symptoms, progression, and treatments. Retrieved from https://www.medicalnewstoday.com/articles/spinal-stensosis-symptoms