Last Updated on November 4, 2025 by mcelik

This condition can lead to significant discomfort and weakness in the legs, which can impact daily life. Learn how spinal stenosis symptoms like leg weakness and numbness develop due to nerve compression.
Spinal stenosis is a narrowing of the spaces within the spine, which can put pressure on the nerves. This pressure can lead to various symptoms, including leg weakness, numbness, and pain. Understanding what spinal stenosis is and its impact on the body is key to managing its effects.
Key Takeaways
- Spinal stenosis is a condition that affects the spine.
- It can cause leg weakness and other symptoms.
- Understanding the causes is important for management.
- Proper diagnosis is key to treating the condition.
- There are various treatment options available.
What Is Spinal Stenosis?

Spinal stenosis is a condition where the spinal canal narrows. This can put pressure on nerves, leading to symptoms. It affects the quality of life.
Definition and Medical Meaning
Spinal stenosis means the spaces in the spine narrow. This can compress the spinal cord or nerves. The word “stenosis” means narrowing, applied to the spine.
This condition can range from mild to severe. It can greatly impact a person’s life, depending on how severe it is.
Prevalence and Demographics
Millions worldwide suffer from spinal stenosis. It’s more common with age, hitting those over 50 hard. It can be present at birth or develop later due to various reasons.
It’s a major cause of disability and pain, mainly in older adults. Knowing who it affects helps in managing it better.
Impact on Quality of Life
Spinal stenosis can significantly affect one’s life. Symptoms can vary from mild to severe, impacting mobility and daily activities. It can also lower overall well-being.
Effective management is key to improving life with spinal stenosis. This includes treatments like medication and surgery to relieve symptoms and enhance function.
Types of Spinal Stenosis

It’s important to know the different types of spinal stenosis to treat it well. This condition is divided by where in the spine it happens and where it narrows.
Cervical Spinal Stenosis
Cervical stenosis is in the neck. It can press on the spinal cord and nerves. This might cause neck pain, numbness in arms or legs, and trouble with balance.
Lumbar Spinal Stenosis
Lumbar stenosis is in the lower back. It’s the most common type. Symptoms include lower back pain, leg pain after standing or walking, and numbness or weakness in the legs.
Thoracic Spinal Stenosis
Thoracic stenosis is in the mid-back. It can cause chest or abdomen pain. In severe cases, it might affect bladder and bowel function.
Central Canal vs. Foraminal Stenosis
Spinal stenosis can be central or foraminal. Central stenosis narrows the central canal, where the spinal cord or cauda equina is. Foraminal stenosis narrows the foramina, where nerve roots exit.
A study says knowing the difference between central and foraminal stenosis is key. It affects symptoms and treatment.
| Type of Stenosis | Location | Common Symptoms |
| Cervical Stenosis | Neck Region | Neck pain, numbness or tingling in arms or legs |
| Lumbar Stenosis | Lower Back | Lower back pain, leg pain, weakness or numbness in legs |
| Thoracic Stenosis | Mid-back Region | Pain or numbness in chest or abdomen |
Each type of spinal stenosis has its own challenges. A specific treatment plan is needed. Accurate diagnosis is key to effective treatment.
The Connection Between Spinal Stenosis and Leg Weakness
Spinal stenosis and leg weakness are linked by nerve compression. When the spine narrows, it presses on nerves. This can stop nerves from working right, causing leg weakness.
How Nerve Compression Affects Muscle Function
Spinal stenosis can weaken leg muscles by compressing nerves. This makes it hard for nerves to send signals to muscles. The weakness’s severity depends on how much the nerves are compressed.
Nerve compression impacts muscle function in several ways:
- Reduced signal transmission: Compressed nerves can’t send signals well, causing muscle weakness.
- Muscle atrophy: Long-term nerve compression can cause muscles to waste away.
- Impaired reflexes: Nerve compression can also mess with reflexes, adding to muscle problems.
Patterns of Weakness in Different Types of Stenosis
The type of spinal stenosis affects where weakness shows up. For example:
Lumbar spinal stenosis usually weakens the lower legs. This is because the narrowing happens in the lower back, where leg nerves are.
Cervical spinal stenosis can weaken arms or legs, depending on the nerves. It can also cause myelopathy, a serious condition with significant weakness.
Distinguishing Stenosis-Related Weakness from Other Causes
It’s important to tell if leg weakness comes from spinal stenosis or something else. Other reasons for weakness include peripheral neuropathy, diabetes, and vascular diseases.
When diagnosing leg weakness, consider these factors:
- Other symptoms like pain, numbness, or tingling.
- Where the weakness is (one leg or both).
- How symptoms change over time.
- Medical history, including past conditions that could cause weakness.
Healthcare professionals use these details to figure out if weakness is from spinal stenosis or something else.
Spinal Stenosis Symptoms: From Mild to Severe
It’s important to know the different symptoms of spinal stenosis. This condition narrows the spinal canal and can cause various symptoms. These symptoms can really affect a person’s life, so it’s key to spot them early.
Early Warning Signs
The first signs of spinal stenosis are often mild. You might feel pain, numbness, or tingling in your back, legs, or arms. For those with lumbar spinal stenosis, pain or weakness in the legs or buttocks is common after standing or walking.
Progressive Symptoms
As spinal stenosis gets worse, symptoms get stronger. You might feel more pain, numbness, or weakness that makes daily tasks hard. Lumbar stenosis can cause pain in the legs when standing or walking, known as neurogenic claudication.
Advanced Symptoms and Complications
At its worst, spinal stenosis can cause serious problems. You might lose bladder or bowel control or even face paralysis. It’s vital to catch symptoms early to avoid these serious issues.
| Stage | Common Symptoms | Impact on Daily Life |
| Early | Mild pain, numbness, tingling | Minimal impact, manageable with conservative treatments |
| Progressive | Increased pain, weakness, neurogenic claudication | Moderate to significant impact, may require medical intervention |
| Advanced | Severe weakness, loss of bladder/bowel control, paralysis | Significant impact, often requires immediate medical attention |
It’s important to know the symptoms of spinal stenosis and how they progress. Being aware of early signs and the risk of worsening symptoms helps patients get the right care. This way, they can manage their condition better.
“Early diagnosis and treatment of spinal stenosis can significantly improve the quality of life for those affected.” –
A spine specialist
Common Causes and Risk Factors
Spinal stenosis can come from degenerative changes, congenital factors, and injuries. Knowing these causes helps doctors diagnose and treat the condition well.
Age-Related Degeneration
As we get older, our spinal discs shrink and lose their bounce. The facet joints also grow, making the spinal canal narrower.
Herniated Discs and Bone Spurs
Herniated discs and bone spurs are big contributors. Herniated discs push into the spinal canal, pressing nerves. Bone spurs, being extra bone growth, also narrow the canal and foramina.
Congenital Factors and Spinal Abnormalities
Being born with a narrow spinal canal increases the risk of spinal stenosis. People with this condition often start showing symptoms early.
Injuries and Trauma
Spinal injuries and trauma can also lead to spinal stenosis. Fractures, dislocations, or other injuries can make the spinal canal narrower.
| Cause/Risk Factor | Description | Impact on Spinal Stenosis |
| Age-Related Degeneration | Loss of disc height and elasticity, enlargement of facet joints | Narrowing of the spinal canal |
| Herniated Discs | Discs protruding into the spinal canal | Nerve compression |
| Bone Spurs | Abnormal bone growth | Narrowing of the spinal canal and foramina |
| Congenital Factors | Narrow spinal canal at birth | Early onset of symptoms |
| Injuries and Trauma | Fractures, dislocations | Narrowing of the spinal canal |
Understanding these causes helps doctors create better treatment plans. This improves how they manage spinal stenosis and helps patients get better.
The Anatomy Behind Spinal Stenosis
To understand spinal stenosis, we need to look at the spine’s structure and how it affects nerves. The spine is made up of vertebrae, discs, and nerves. These parts work together to support the body and help it move.
Normal Spine Structure
The spine has 33 vertebrae, divided into five areas: cervical, thoracic, lumbar, sacrum, and coccyx. Between these vertebrae are discs that cushion and help the spine move. The spine protects the spinal cord and nerves.
The spinal cord is key to our nervous system. It needs protection. The vertebrae and discs create a safe space for it and the nerves.
The Spinal Canal and Neural Foramina
The spinal canal is a tube made of vertebrae. It houses the spinal cord and nerves. The neural foramina are small openings where nerves leave the spinal canal. Both are vital for nerve function.
- The spinal canal protects the spinal cord.
- Neural foramina allow nerves to exit and supply various parts of the body.
How Narrowing Affects Nerve Function
When the spinal canal or neural foramina narrow, nerves can get compressed. This can cause pain, numbness, and weakness. These symptoms are common in spinal stenosis.
Narrowing can happen for many reasons, like aging, herniated discs, or bone spurs. Knowing these causes helps doctors diagnose and treat spinal stenosis.
We will look more into spinal stenosis and its treatments in the next sections.
Lower Extremity Symptoms Beyond Weakness
Spinal stenosis can cause many symptoms in the lower body. These symptoms can really affect how well you live your life. Weakness is common, but there are other symptoms too. These can make everyday tasks hard and affect your happiness.
Neurogenic Claudication
Neurogenic claudication is a key symptom of spinal stenosis. It causes pain or tiredness in the legs when you walk or stand. Resting, bending forward, or sitting can help make the pain go away.
Key characteristics of neurogenic claudication include:
- Pain or discomfort in the legs, thighs, or buttocks
- Symptoms triggered by standing or walking
- Relief obtained by bending forward, sitting, or resting
Numbness and Tingling Sensations
Many people with spinal stenosis feel numbness or tingling in their legs. These feelings can be uncomfortable and might get worse if not treated.
The numbness and tingling can spread in different ways. It depends on which nerves are affected by the stenosis.
Pain Patterns and Distribution
The pain from spinal stenosis can show up in different ways. Some people feel pain in one spot, like the lower back. Others might feel pain that spreads down their leg.
| Pain Characteristic | Description |
| Localized Pain | Pain confined to a specific area, such as the lower back or buttock |
| Radiating Pain | Pain that travels along the nerve pathway, often down the leg |
| Sharp or Shooting Pain | Sudden, severe pain that may be associated with nerve compression |
Balance and Coordination Problems
Spinal stenosis can also cause balance and coordination issues. This is because nerves that control the legs are compressed. This can make it easier to fall and increase the risk of accidents.
Patients experiencing balance problems may benefit from:
- Physical therapy to improve strength and coordination
- Assistive devices, such as canes or walkers, to enhance stability
Diagnosing Spinal Stenosis
To diagnose spinal stenosis, we take a detailed approach. We look at the patient’s medical history and perform physical exams. We also use advanced tests to get an accurate diagnosis.
Medical History and Physical Examination
Understanding the patient’s medical history is key. We ask about their symptoms and how long they’ve had them. We also check muscle strength, reflexes, and sensation in the affected areas.
During the physical exam, we might do the straight leg raise test. This test checks for nerve irritation. We also look at the patient’s gait and posture for any signs of spinal stenosis.
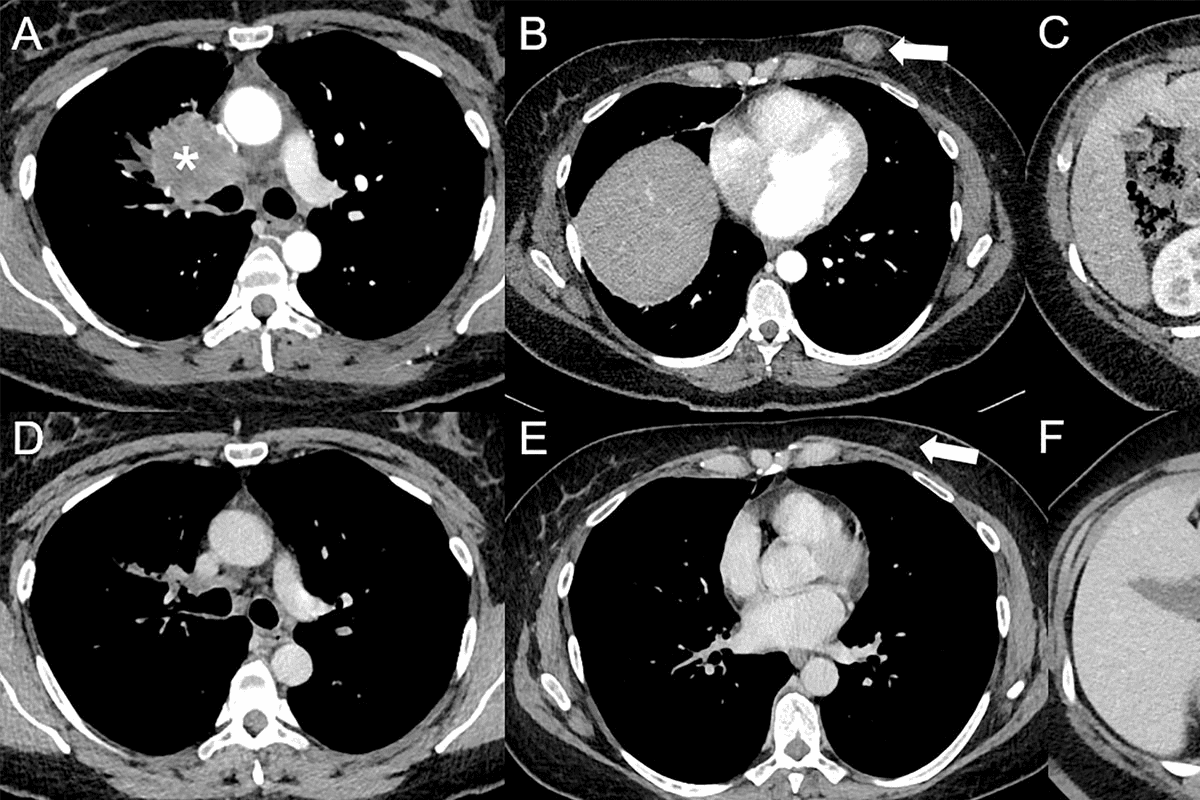
Imaging Technologies
Imaging studies are essential for confirming spinal stenosis. We use different imaging methods, including:
- Magnetic Resonance Imaging (MRI): MRI is the top choice for diagnosing spinal stenosis. It shows detailed images of the spinal canal and neural foramina.
- Computed Tomography (CT) scans: CT scans help us see bony structures. They can spot bone spurs or other bone issues that might cause stenosis.
- X-rays: X-rays can give us initial info on the spine’s alignment and any degenerative changes. They’re not as detailed as MRI or CT, though.
| Imaging Modality | Advantages | Limitations |
| MRI | Excellent soft tissue visualization, sensitive to nerve compression | Contraindicated in patients with certain metal implants, claustrophobia |
| CT scan | Good for visualizing bony structures, quick and widely available | Less sensitive to soft tissue changes, radiation exposure |
| X-ray | Quick, low cost, useful for initial assessment | Limited detail, not sensitive to soft tissue or nerve compression |
Nerve Conduction Studies and EMG
Nerve conduction studies (NCS) and electromyography (EMG) are tests that check nerve function. They help identify nerve damage or dysfunction. These tests are useful when the diagnosis is unclear or when planning surgery.
“The use of NCS and EMG can provide valuable information about the functional impact of spinal stenosis on the nervous system, helping to guide treatment decisions.”
NCS measures nerve signal speed and strength. EMG looks at muscle electrical activity. Together, they show the extent of nerve damage and muscle denervation, if any.
When to Seek Medical Attention
Getting medical help quickly is key to avoiding long-term damage from spinal stenosis. We’ll help you spot the warning signs. If spinal stenosis isn’t treated fast, it can cause serious problems.
Warning Signs That Require Immediate Care
Some symptoms mean you need to see a doctor right away. Look out for sudden severe pain, numbness, or weakness in the legs. If you notice these, get medical help fast to stop things from getting worse.
Cauda Equina Syndrome
Cauda equina syndrome is a serious issue from spinal stenosis. It happens when nerves in the lower back get squished, causing big problems. You might feel severe pain, weakness, and bladder or bowel issues. This is a medical emergency that needs surgery right away to avoid lasting harm.
Progressive Neurological Deficits
Seeing your symptoms get worse, like more weakness or numbness in your legs, is a bad sign. It means your condition is getting worse and needs quick medical help. This can help stop or slow down the problem.
Keep an eye on your symptoms and get medical help if you see any warning signs. Early treatment can make a big difference for people with spinal stenosis.
Non-Surgical Treatment Approaches
Spinal stenosis can be managed without surgery, improving life quality. These methods help reduce symptoms, boost mobility, and enhance well-being.
Physical Therapy and Exercise Programs
Physical therapy is key in managing spinal stenosis. A tailored exercise plan can improve flexibility and strengthen the spine’s muscles. It also helps with posture.
- Stretching exercises to improve flexibility
- Strengthening exercises for core and back muscles
- Aerobic exercises like walking or swimming to improve cardiovascular health
These exercises not only manage symptoms but also boost physical fitness.
Medications for Pain and Inflammation
Several medications can help with pain and inflammation from spinal stenosis. These include:
- Oral analgesics like acetaminophen for pain relief
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and pain
- Oral steroids for short-term use to reduce severe inflammation
It’s important to talk to a healthcare provider to find the right medication and dosage.
Epidural Steroid Injections
Epidural steroid injections are a common treatment for spinal stenosis. They are used when oral medications or physical therapy don’t work. These injections deliver steroids to the epidural space, reducing inflammation and pain.
The procedure is done under fluoroscopic guidance for accuracy.
Alternative and Complementary Therapies
Several alternative and complementary therapies can help with spinal stenosis symptoms. These include:
- Chiropractic care to improve spinal alignment and reduce pressure on the nerves
- Acupuncture to stimulate healing and reduce pain
- Massage therapy to relax tense muscles and improve circulation
While these therapies can be helpful, it’s important to talk to a healthcare provider. This ensures they fit with the overall treatment plan.
Surgical Interventions for Spinal Stenosis
Surgical treatments are a big help for those with severe spinal stenosis. If other treatments don’t work, surgery can greatly improve life quality.
Decompression Procedures
Decompression surgery helps by taking pressure off the spinal cord or nerves. It removes bone spurs, herniated discs, or other tissues that press on nerves. This makes more space and less irritation or damage to nerves.
Spinal Fusion Techniques
Spinal fusion might be needed to keep the spine stable after decompression. It joins vertebrae together with bone grafts, rods, or other devices. This helps keep the spine stable and stops further wear and tear.
Minimally Invasive Options
Minimally invasive surgery is getting more popular for spinal stenosis. It uses smaller cuts and less damage to tissues. This can lead to faster recovery and fewer problems. Examples include microdiscectomy or laminotomy.
Recovery and Rehabilitation
Recovery from spinal stenosis surgery varies. Patients usually need rest and physical therapy to get strong and mobile again. A good rehab plan is key for the best results and getting back to normal.
Choosing surgery is a big step. Our team is here to give full care and support. We aim for the best results for our patients.
Managing Daily Life with Spinal Stenosis
Spinal stenosis can make daily tasks hard, but there are ways to cope. It’s important to use medical treatments, make lifestyle changes, and use tools to stay independent. This helps keep your life quality high.
Adaptive Strategies for Activities
It’s key to adapt daily tasks for those with spinal stenosis. Taking breaks to rest can help manage symptoms. Breaking big tasks into smaller ones also helps avoid making the condition worse.
- Prioritize tasks based on importance and energy levels
- Use pacing techniques to avoid overexertion
- Modify activities to reduce strain on the spine
Ergonomic Considerations
Good ergonomics can lessen discomfort and boost function. It’s vital to set up work and living spaces for good posture and less spine strain.
Key ergonomic tips include:
- Maintaining a neutral spine position when sitting or standing
- Using supportive chairs and backrests
- Adjusting the height of work surfaces to avoid bending or reaching
Assistive Devices and Mobility Aids
Assistive devices and mobility aids can boost independence and safety. They include canes, walkers, and other tools to ease spine strain and improve movement.
Some common assistive devices include:
- Canes for additional support
- Walkers for stability
- Reachers or grabbers to avoid bending
Exercise Recommendations
Exercise is key in managing spinal stenosis. Gentle exercises that strengthen the spine muscles and improve flexibility can ease symptoms.
Recommended exercises may include:
- Gentle stretching to improve flexibility
- Low-impact aerobic exercises, such as swimming or cycling
- Strengthening exercises for core and back muscles
By using these strategies daily, people with spinal stenosis can better handle their symptoms. This helps keep their quality of life high.
Long-Term Prognosis and Outlook
Knowing how spinal stenosis will progress is key to managing it well. The disease’s impact on a patient’s life can change a lot.
Natural History
Spinal stenosis gets worse over time. Its progress depends on age, how severe it is, and other health issues. Studies show some people’s symptoms get worse slowly, while others stay the same for years.
Factors Affecting Progression
Several things can make spinal stenosis get worse, including:
- Age: Older people tend to see it get worse faster.
- Severity of Stenosis: If it’s more severe when first found, it might be harder to treat.
- Presence of Other Health Conditions: Diseases like diabetes or heart disease can make it worse.
Quality of Life Considerations
Spinal stenosis can really affect how well a person lives. Good treatment helps keep people moving and less in pain.
“The goal of treatment is not just to alleviate symptoms but to improve the patient’s overall quality of life.”
Monitoring and Follow-up Care
Keeping an eye on spinal stenosis and getting regular check-ups is important. This includes:
- Seeing healthcare providers often.
- Doing tests to see how the stenosis is changing.
- Changing the treatment plan if needed.
In summary, knowing about spinal stenosis’s long-term outlook means looking at its natural course, what makes it worse, and how it affects life. Good care and regular check-ups are key to better outcomes.
Conclusion
Spinal stenosis is a complex condition that affects millions worldwide. It causes a lot of discomfort and limits movement. Understanding its symptoms, causes, and treatments is key to managing it well. Recognizing signs like leg weakness, numbness, and pain is important. Knowing the different types of stenosis helps too. Early diagnosis and the right treatment, whether non-surgical or surgical, greatly improve life quality. This article on spinal stenosis shows how important it is to understand the condition. It’s vital for both patients and healthcare providers. A summary of spinal stenosis highlights the need for a team approach to care. This includes physical therapy, medications, and lifestyle changes. These help reduce symptoms and improve overall health. By providing a summary on stenosis, we stress the need for more research and awareness. This is to help those living with spinal stenosis have better outcomes.
FAQ
What is spinal stenosis?
Spinal stenosis is a condition where the spinal canal narrows. This can put pressure on the spinal cord and nerves. It leads to symptoms like leg weakness.
How does spinal stenosis affect leg strength?
It can weaken the legs by pressing on the nerves. This can cause anything from mild weakness to severe muscle loss.
What are the common symptoms of spinal stenosis?
Symptoms include leg weakness, numbness, tingling, pain, and balance issues. It also causes neurogenic claudication. This is pain, weakness, or fatigue in the legs when walking or standing.
What causes spinal stenosis?
It’s often caused by degenerative changes like herniated discs and bone spurs. Congenital factors, injuries, and trauma also play a role.
How is spinal stenosis diagnosed?
Doctors use a medical history, physical exam, and imaging like MRI or CT scans. They also do nerve conduction studies and EMG.
What are the treatment options for spinal stenosis?
Non-surgical treatments include physical therapy and medications. Epidural steroid injections and alternative therapies are also options. Surgery, like decompression and spinal fusion, is another choice.
Can spinal stenosis be cured?
While it’s a chronic condition, treatments can manage symptoms and slow its progression. This improves quality of life.
How can I manage daily life with spinal stenosis?
Use adaptive strategies and ergonomic considerations. Assistive devices and mobility aids help. Recommended exercises are also important.
What is the long-term prognosis for spinal stenosis?
The prognosis depends on the condition’s severity, treatment success, and individual health and lifestyle.
When should I seek medical attention for spinal stenosis?
Seek medical help for severe pain, progressive neurological deficits, or cauda equina syndrome. These are urgent.
Can spinal stenosis cause permanent nerve damage?
Untreated spinal stenosis can cause permanent nerve damage. Timely diagnosis and treatment are key.
Is surgery always necessary for spinal stenosis?
Surgery isn’t always needed. Many people find relief with non-surgical treatments. The decision to have surgery depends on symptoms and treatment success.
References
- Munakomi, S., et al. (2023). Spinal stenosis and neurogenic claudication. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK430872/