Chronic kidney disease (CKD) is a serious issue affecting millions globally. Stage 4 CKD is a critical point where kidneys work at only 15-29% of their normal capacity. This is shown by an estimated glomerular filtration rate (eGFR) between 15 and 29 ml/min/1.73m2.stage 4 kidney failureStage 1 Kidney Disease: Early Treatment Guide
At this stage, the risk of serious complications grows. About 1 in 7 adults in the United States has CKD. Elderly patients with advanced kidney disease are at even higher risk. Sadly, 45% of them die mainly from heart disease, not kidney failure.
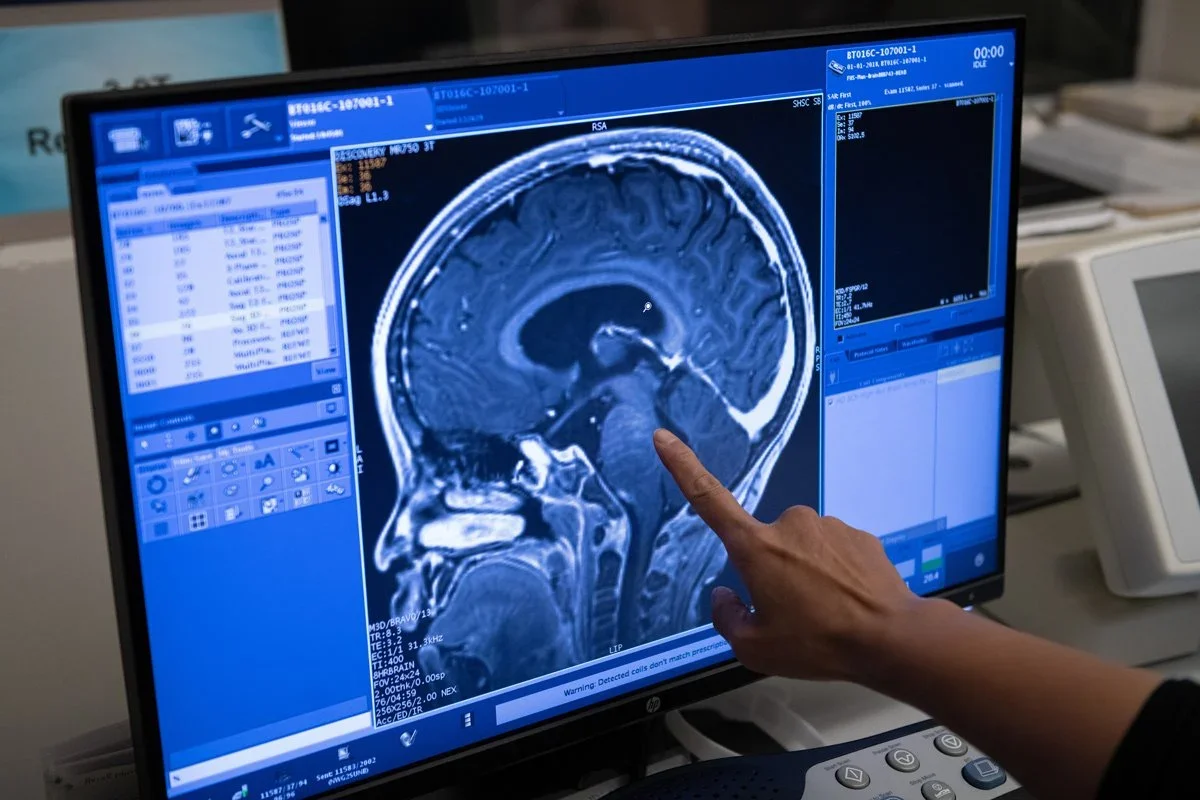
Though damage can’t be undone, treatments and lifestyle changes can slow the disease. At Liv Hospital, we focus on our patients, following international medical standards. We aim to give the best care for those with advanced CKD.
Key Takeaways
- Stage 4 CKD is a critical point in the disease’s progression, with kidneys functioning at 15-29% of normal capacity.
- Approximately 1 in 7 adults in the United States are affected by CKD.
- Elderly patients with advanced kidney disease face high risks of cardiovascular disease.
- Evidence-based treatment strategies and lifestyle modifications can slow disease progression.
- Liv Hospital provides extensive care for patients with advanced CKD, following international medical standards.
Understanding Stage 4 Kidney Disease
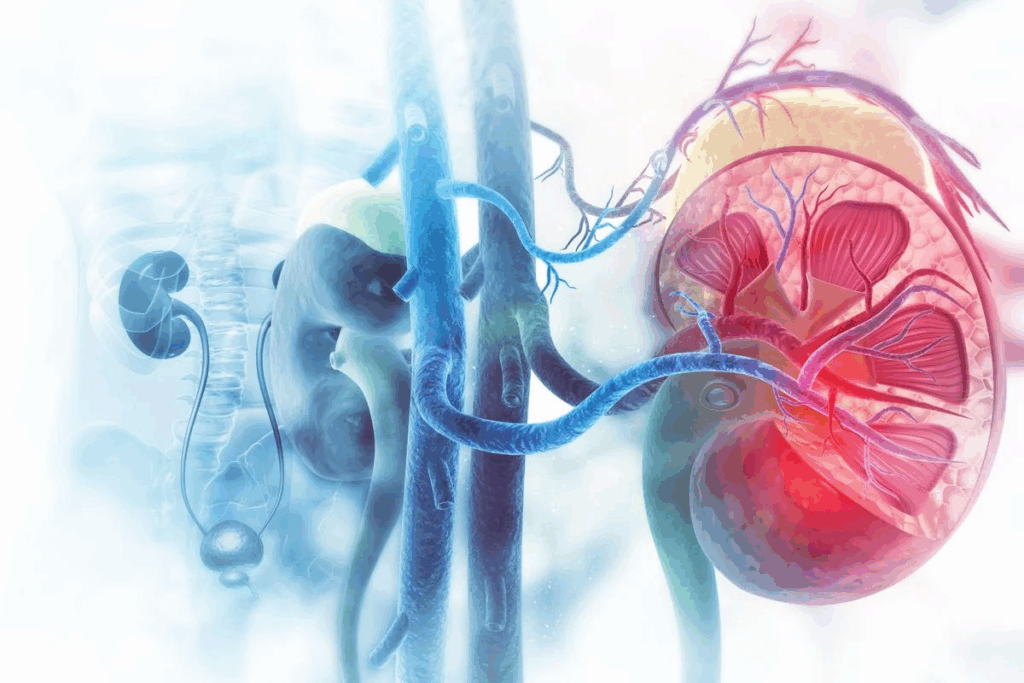
Understanding Stage 4 chronic kidney disease (CKD) is key for patients. It helps them choose the right treatment. Stage 4 CKD means the kidneys are badly damaged and don’t work right.
Definition and Diagnostic Criteria
Stage 4 CKD has a glomerular filtration rate (GFR) of 15 to 29 mL/min/1.73m. This shows the kidneys can’t filter waste well. Doctors use blood tests to check GFR and urine tests to see damage.
The criteria for Stage 4 CKD are:
- Significantly reduced GFR
- Presence of kidney damage markers in the blood or urine
- Symptoms associated with advanced kidney disease
GFR Levels and Kidney Function Percentage
GFR measures kidney function. At Stage 4, it’s between 15 and 29. This means kidney function is 25% or less of normal. It shows severe kidney damage.
CKD Stage | GFR Level (mL/min/1.73m2) | Kidney Function Percentage |
Stage 1 | 90+ | 90-100% |
Stage 2 | 60-89 | 60-89% |
Stage 3 | 30-59 | 30-59% |
Stage 4 | 15-29 | 15-29% |
Stage 5 | <15 | <15% |
Common Symptoms and Warning Signs
Stage 4 patients may feel tired, weak, and have swelling. They might also urinate more or less than usual. Other signs include nausea and loss of appetite.
- Fatigue and weakness
- Swelling in the legs, ankles, and feet
- Changes in urination frequency
- Nausea and loss of appetite
Risk Factors and Disease Progression
Several things can make CKD worse. These include diabetes, high blood pressure, family history, age, and obesity. Managing these risks is key to slowing CKD.
By understanding CKD, patients can work with doctors to manage it. This helps slow the disease’s progress.
The Reality of Stage 4 Kidney Failure: Can It Be Reversed?
Understanding Stage 4 kidney disease is key for patients and doctors. At this stage, the kidneys are badly damaged. The goal now is to manage the disease and its effects.
Medical Facts About Kidney Damage at Stage 4
Stage 4 kidney disease means the kidneys don’t work well. The glomerular filtration rate (GFR) is very low, showing kidney failure. Patients often face symptoms like anemia and heart problems.
The damage to the kidneys is irreversible. But, treatments can slow down the disease’s progress to Stage 5, or end-stage renal disease (ESRD).
The Difference Between Reversal and Slowing Progression
It’s important to know the difference between reversing and slowing kidney disease. Reversal means getting the kidneys back to normal. Slowing progression means stopping the disease from getting worse. Right now, we can slow the disease better than reverse it.
Treatments aim to fix the cause, manage symptoms, and prevent complications. This helps patients live better and may delay the need for kidney replacement.
Success Stories and Their Clinical Context
Some patients with Stage 4 kidney disease have improved a lot. Their success comes from good medical care, lifestyle changes, and diet.
For example, controlling blood pressure and diabetes can slow kidney disease. Also, following a special diet can help the kidneys less.
Setting Realistic Treatment Goals
It’s important to set realistic goals for Stage 4 kidney disease. This means knowing the kidney’s current state, spotting possible problems, and finding ways to handle them.
Patients and doctors need to work together. They should make a detailed care plan. This plan includes regular check-ups, medicine, diet, and lifestyle changes based on the patient’s needs.
Comprehensive Medical Management for Stage 4 CKD
Stage 4 CKD patients need a wide range of medical care. This care aims to manage symptoms and slow the disease’s progress. It includes using medicines, controlling blood pressure, managing diabetes, and regular lab tests.
Medication Protocols and Management
Medicines are key in treating Stage 4 CKD. We use them to control symptoms, slow the disease, and handle complications. These medicines include:
- ACE inhibitors or ARBs to protect kidney function
- Diuretics to manage fluid overload
- Phosphate binders to control phosphorus levels
- Vitamin D supplements to manage bone disease
It’s important to follow your medicine plan and tell your doctor about any side effects.
Blood Pressure Control Strategies
Keeping blood pressure in check is vital. We suggest:
- Lifestyle changes like diet and exercise
- Medicines like ACE inhibitors or ARBs
- Regular blood pressure checks
Keeping blood pressure in a target range can slow CKD’s progress.
Managing Diabetes and Other Underlying Conditions
For those with diabetes, controlling blood sugar is key. We recommend:
- Keeping blood sugar in check with diet, exercise, and medicine
- Checking HbA1c levels often
- Changing treatment plans as needed to keep blood sugar in range
It’s also important to manage other conditions like high blood pressure and heart disease.
Regular Monitoring and Laboratory Tests
Lab tests are vital for checking kidney function and adjusting treatment. These tests may include:
Laboratory Test | Purpose |
Serum Creatinine | Assess kidney function |
eGFR | Estimate kidney function |
Electrolyte Levels | Monitor for imbalances |
Urine Protein | Assess kidney damage |
Renal Nutrition: Dietary Approaches for Stage 4 Kidney Disease
Renal nutrition is a proactive way to manage Stage 4 kidney disease. It involves a diet plan tailored to the patient’s needs. This approach can slow disease progression, manage symptoms, and improve health.
Protein Restriction Guidelines and Implementation
Protein restriction is key for Stage 4 kidney disease patients. Limiting protein intake helps reduce kidney strain. The right amount of protein depends on age, weight, and health status.
Experts suggest eating 0.8 grams of protein per kilogram of body weight daily. It’s important to get this amount right. A healthcare provider or renal dietitian can help figure it out.
Sodium, Potassium, and Phosphorus Management
Managing sodium, potassium, and phosphorus is vital. Excessive intake can cause problems like high blood pressure, high potassium levels, and bone disease.
- Sodium: Keep sodium intake under 2,300 mg daily. Opt for low-sodium foods and avoid processed ones.
- Potassium: Avoid foods high in potassium like bananas, oranges, and potatoes. The right amount varies; check with a healthcare provider.
- Phosphorus: Limit foods rich in phosphorus, such as dairy, meats, and processed foods. Phosphorus binders might be needed to control levels.
Mineral | Recommended Intake | Foods to Limit |
Sodium | < 2,300 mg/day | Processed foods, table salt |
Potassium | Varies | Bananas, oranges, potatoes |
Phosphorus | Varies | Dairy products, meats, processed foods |
Fluid Intake Recommendations and Tracking
Fluid management is key for Stage 4 kidney disease patients. Monitoring fluid intake prevents dehydration and fluid overload.
The right amount of fluid varies based on individual needs, urine output, and health. Patients should track their fluid intake and output to stay balanced.
“Adequate hydration is essential, but excessive fluid intake can strain the kidneys. Patients should work closely with their healthcare team to determine the optimal fluid intake.”
Working Effectively with a Renal Dietitian
A renal dietitian is vital in creating a personalized diet plan. They help patients understand their dietary needs, manage mineral intake, and maintain nutritional health.
By working with a renal dietitian, patients can develop a diet plan that meets their specific needs, lifestyle, and preferences.
Lifestyle Modifications to Slow Stage 4 Kidney Failure Progression
Managing Stage 4 kidney disease needs a mix of changes. These adjustments can slow the disease and improve life quality.
Appropriate Exercise Programs for CKD Patients
Exercise is key for those with Chronic Kidney Disease (CKD). Tailored workouts help keep function, lower heart risks, and boost mood. Aerobic exercises like walking or swimming are good. Resistance training is also helpful with careful supervision.
Stress Management and Mental Health Support
Living with a chronic illness affects mental health. Stress-busting methods like meditation, yoga, or cognitive-behavioral therapy are helpful. Support groups offer a place to share and get advice.
Sleep Optimization Strategies
Good sleep is vital, more so for those with kidney disease. A regular sleep schedule and a calm sleep area are key. Avoiding caffeine and electronics before bed also helps. Sometimes, doctors suggest special treatments for sleep issues.
Avoiding Nephrotoxic Substances and Medications
Some substances and meds can harm kidneys. Knowing about nephrotoxins is important. People with Stage 4 kidney disease should talk to their doctor before trying new meds or supplements. Also, avoiding toxins and heavy metals helps keep kidneys working.
By making these lifestyle changes, people with Stage 4 kidney disease can manage their condition better. This can slow the disease’s progress.
Managing Complications in Stage 4 Kidney Disease
Stage 4 CKD brings many complications that need careful handling. Managing these issues well is key to keeping patients’ quality of life high and slowing disease growth.
Treating Anemia and Fatigue
Anemia is common in Stage 4 CKD, causing fatigue, weakness, and shortness of breath. We treat anemia with iron supplements, erythropoiesis-stimulating agents (ESAs), and fixing nutritional gaps.
Key Strategies for Managing Anemia:
- Regular monitoring of hemoglobin levels
- Iron therapy to maintain adequate iron stores
- Use of ESAs to stimulate red blood cell production
Bone Disease Prevention and Management
CKD-mineral and bone disorder (CKD-MBD) is a big problem, causing bone pain, fractures, and heart disease. We prevent and manage bone disease by watching mineral levels like calcium, phosphorus, and parathyroid hormone (PTH).
Mineral | Normal Level | CKD Stage 4 Target |
Calcium | 8.5-10.5 mg/dL | 8.4-9.5 mg/dL |
Phosphorus | 2.5-4.5 mg/dL | 3.5-5.5 mg/dL |
PTH | 15-65 pg/mL | 2-9 times upper normal limit |
Cardiovascular Risk Reduction Strategies
Heart disease is a big killer in CKD patients. We lower heart disease risk with diet, exercise, and managing high blood pressure, diabetes, and bad cholesterol.
“The management of cardiovascular risk in CKD patients requires a multifaceted approach, including lifestyle changes and pharmacological interventions.”
KDOQI Guidelines
Addressing Mineral and Electrolyte Imbalances
Imbalances in minerals and electrolytes can cause serious problems like heart rhythm issues and muscle weakness. We fix these imbalances with diet, medicine, and regular blood tests.
By tackling Stage 4 CKD complications fully, we can greatly improve patient outcomes and quality of life.
Special Considerations for Elderly Patients with Stage 4 Kidney Disease
As people get older, treating Stage 4 kidney disease gets more complex. Elderly patients with Stage 4 chronic kidney disease face special challenges. We need to tailor their treatment carefully.
Age-Related Challenges in Treatment
Elderly patients often see a drop in physical ability. They might also have other health issues. These factors make treating Stage 4 CKD harder.
- Cognitive impairment can affect adherence to medication and treatment regimens.
- Physical limitations may impact the ability to perform certain tasks, such as dialysis.
- Multiple comorbidities can complicate treatment and increase the risk of adverse events.
Medication Adjustments for Older Adults
Older adults with Stage 4 CKD often need changes in their medications. This is because of age-related changes in kidney function and other factors. We must manage their medications carefully to avoid bad side effects.
Key considerations include:
- Dose adjustments for reduced kidney function.
- Avoiding nephrotoxic medications when possible.
- Monitoring for possible drug interactions.
Quality of Life Considerations
Keeping quality of life high is key for elderly patients with Stage 4 CKD. We should focus on managing symptoms, reducing complications, and improving overall well-being.
Strategies to enhance quality of life include:
- Effective pain management.
- Addressing nutritional needs and deficiencies.
- Providing emotional and psychological support.
Coordinating Care with Multiple Health Conditions
Elderly patients with Stage 4 CKD often have many health conditions. We must work closely with different healthcare providers to manage them well.
By taking a team approach and considering the unique needs of elderly patients, we can improve outcomes and enhance quality of life.
Preparing for Renal Replacement Therapy
Preparing for renal replacement therapy is key for those with advanced kidney disease. As we move into the later stages of chronic kidney disease (CKD), knowing our options is vital. This includes dialysis, transplantation, and vascular access planning.
When to Consider Dialysis or Transplantation
Deciding on dialysis or transplantation comes when kidney function drops too low. Regular monitoring by a healthcare provider is essential. This decision depends on health, symptoms, and lab results.
- Monitoring kidney function through regular GFR tests
- Assessing symptoms and adjusting treatment
- Discussing options with a nephrologist
Types of Dialysis: Hemodialysis vs. Peritoneal Dialysis
Hemodialysis and peritoneal dialysis are the main dialysis types. Hemodialysis uses a machine to filter blood outside the body. Peritoneal dialysis uses the abdomen to filter waste, giving more freedom.
Characteristics | Hemodialysis | Peritoneal Dialysis |
Location | Dialysis center or home | Home |
Frequency | Several times a week | Daily exchanges |
Flexibility | Limited by center hours | More flexible scheduling |
Kidney Transplantation Evaluation and Process
Kidney transplantation is an option for those with end-stage renal disease. The process includes a thorough check to see if you’re a good candidate. Understanding the transplant process can help ease concerns.
- Initial evaluation and testing
- Listing on the transplant waiting list
- Matching with a donor kidney
- Transplant surgery and post-operative care
Vascular Access Planning and Preparation
For hemodialysis patients, vascular access is critical. This involves surgically connecting an artery and vein for dialysis. Early planning is key to ensure access is ready and to avoid complications.
Understanding and preparing for renal replacement therapy helps patients make informed decisions. This improves their quality of life and outcomes. We suggest discussing these options with a healthcare provider to find the best path forward.
Conclusion: Creating a Comprehensive Care Plan for Stage 4 Kidney Disease
Managing Stage 4 Chronic Kidney Disease (CKD) needs a team effort. It includes medical care, lifestyle changes, and getting ready for kidney replacement. We’ve talked about ways to slow the disease, handle problems, and boost life quality.
A detailed care plan is key for managing Stage 4 kidney disease. It means working with doctors, following medication, and changing your lifestyle. With help from a renal dietitian, you can create a diet that’s good for you and your kidneys.
Getting ready for kidney replacement is also important. Knowing about hemodialysis, peritoneal dialysis, and kidney transplant can help you choose the best option. A good care plan helps Stage 4 CKD patients stay healthy and feel better overall.
FAQ
What is Stage 4 Kidney Disease?
Stage 4 Kidney Disease is a serious kidney issue. It happens when the kidneys are badly damaged. They don’t work right, with a glomerular filtration rate (GFR) between 15-29 ml/min.
How bad is Stage 4 Kidney Disease?
Stage 4 Kidney Disease is very serious. It needs careful medical care to slow it down and manage symptoms. If not treated, it can lead to kidney failure, needing dialysis or a transplant.
Is Stage 4 Kidney Disease reversible?
Some kidney damage can be reversed. But Stage 4 Kidney Disease is usually not reversible. Yet, with the right treatment and lifestyle changes, you can slow it down and manage symptoms.
What are the symptoms of Stage 4 Kidney Disease?
Symptoms include fatigue, swelling, and changes in urination. Electrolyte imbalances are also common. As it gets worse, symptoms like nausea, vomiting, and shortness of breath may appear.
How is Stage 4 Kidney Disease diagnosed?
Doctors use lab tests, like serum creatinine and urea, and eGFR calculations. They also look at your medical history and do a physical exam.
What is the treatment for Stage 4 Kidney Disease?
Treatment includes medical care, lifestyle changes, and diet. This might include medicines, managing blood pressure, and controlling diabetes.
Can I slow the progression of Stage 4 Kidney Disease?
Yes, you can slow it down with the right treatment and lifestyle changes. This includes managing blood pressure, controlling blood sugar, and making dietary changes.
What dietary changes are recommended for Stage 4 Kidney Disease?
You should limit protein, manage sodium, potassium, and phosphorus, and watch your fluid intake. A renal dietitian can help with a personalized meal plan.
When should I consider dialysis or transplantation?
You should think about dialysis or transplant when symptoms are severe and quality of life is affected. The decision is made with your healthcare provider.
What are the special considerations for elderly patients with Stage 4 Kidney Disease?
Elderly patients need special care, including medication adjustments and quality of life considerations. Managing multiple health conditions is also key.
How can I manage complications associated with Stage 4 Kidney Disease?
Managing complications involves treating anemia and fatigue, preventing bone disease, reducing heart risks, and managing mineral and electrolyte imbalances.
What lifestyle modifications can help slow Stage 4 Kidney Disease progression?
Lifestyle changes include regular exercise, stress management, better sleep, and avoiding harmful substances.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7044433/