Last Updated on December 3, 2025 by Bilal Hasdemir

Stem Cell Injections Knee
Knee osteoarthritis is a big problem worldwide, causing a lot of pain and making it hard to move. Stem cell injections knee therapy is being looked at as a powerful new way to help slow cartilage damage, reduce inflammation, and improve joint function safely.
Studies suggest that stem cell injections knee pain might help and make joints work better. As this area of research grows, it’s important to keep up with the latest findings.
Key Takeaways
- Stem cell therapy is a promising treatment for knee osteoarthritis.
- Research has shown that stem cell injections knee can alleviate pain.
- Stem cell therapy can improve joint function in patients with osteoarthritis.
- The field of stem cell therapy is continuously evolving.
- More research is needed to fully understand the benefits of stem cell injections.
Understanding Knee Osteoarthritis and Joint Degeneration
It’s important to understand knee osteoarthritis to find good treatments. This condition involves many factors, like cartilage loss, meniscus degeneration, and synovium inflammation.
Common Causes of Knee Cartilage Damage
Knee cartilage damage comes from several sources. Aging, trauma, obesity, and genetics are key factors. As we get older, our cartilage wears down. Trauma, like fractures or ligament tears, can start the damage. Being overweight also adds stress to the knee, speeding up wear.
Genetics play a big role too. If your family has osteoarthritis, you might get it. Other factors, like gender and hormones, also affect the condition.
The Progressive Nature of Knee Osteoarthritis
Knee osteoarthritis gets worse over time if not treated. Cartilage loss causes pain and stiffness, affecting your life. As it worsens, the joint space shrinks, and bone spurs form, making symptoms worse.
| Stage | Characteristics | Symptoms |
| Early | Cartilage degeneration begins | Mild pain, stiffness |
| Moderate | Joint space narrowing, bone spurs | Moderate pain, reduced mobility |
| Advanced | Significant cartilage loss, bone-on-bone contact | Severe pain, significant mobility issues |
Limitations of Natural Healing in Cartilage Tissue
Cartilage can’t heal well because it lacks blood. This makes it hard for nutrients and cells to reach it. So, damaged cartilage often doesn’t heal, leading to osteoarthritis.
Using autologous stem cells and other regenerative therapies is promising. They help repair and grow cartilage, giving hope to those with knee osteoarthritis.
The Science Behind Stem Cell Injections Knees
MSC injections for knee regeneration
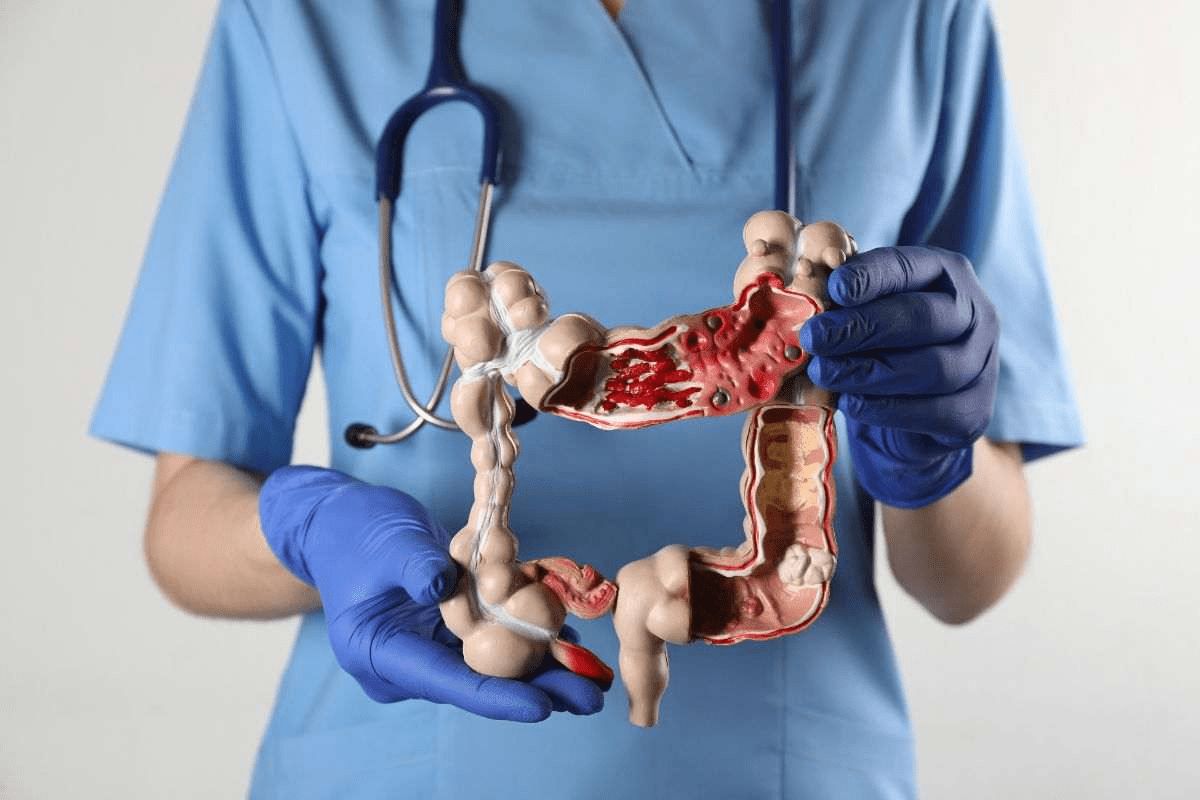
The science of stem cell injections knees uses mesenchymal stem cells (MSCs). These cells help the body fix itself, which can make joints work better and hurt less. This method is part of regenerative medicine, which helps the body heal itself.
Definition and Basic Mechanism of Action
Mesenchymal stem cells (MSCs) help fix and grow new tissue. They can turn into different types of cells, like bone and cartilage cells. When put in the knee, MSCs might fix damaged cartilage, lower swelling, and make the joint work better.
Types of Stem Cells Used in Knee Treatments
There are different stem cells for knee treatments. Autologous stem cells come from the patient themselves, and allogeneic MSCs come from donors. Autologous stem cells are often used in MSC injections. Allogeneic MSCs are easy to get and follow a set treatment plan.
How MSCs May Promote Tissue Repair
MSCs help fix tissue in several ways. They can turn into cells that fix damaged areas, like cartilage. They also release growth factors that help healing, reduce swelling, and make the joint better. This mix of actions helps in knee regeneration therapies.
Types of Stem Cell Therapies for Knee Conditions
Stem cell therapy has grown to offer many ways to treat knee problems. This growth comes from research into the best ways to use stem cells to fix or grow back damaged knee tissues.
Autologous Stem Cells: Sources and Processing
Autologous stem cells come from the patient’s own body, usually from bone marrow or fat. Using these cells means there’s no risk of the body rejecting them. They are taken, processed, and put back into the knee to help it heal.
Processing these cells means pulling them out of other cells and making them more concentrated. This step is key to making sure the cells work well and help fix tissues.
Allogeneic MSCs: Donor-Derived Options
Allogeneic MSCs come from donors, making them ready to use right away. These cells are from healthy donors and are checked and processed to be safe and effective.
Using donor MSCs has benefits like being ready to use right away and having consistent quality. But, there’s a small chance of a reaction from the immune system.
Bone Marrow Aspirate Concentrate (BMAC)
Bone Marrow Aspirate Concentrate (BMAC) is a way to use autologous stem cells. It involves taking bone marrow from the patient, usually from the hip, and then concentrating the stem cells.
BMAC has stem cells, growth factors, and other cells that help fix tissues. The concentrated solution is then injected into the knee to help it heal.
Adipose-Derived Stem Cells
Adipose-derived stem cells come from the patient’s fat, often taken through liposuction. These cells are popular because they’re easy to get and work well.
These stem cells can grow into different types of cells and help fix tissues. This makes them a good choice for treating knee problems.
| Therapy Type | Cell Source | Key Benefits |
| Autologous Stem Cells | Patient’s own tissues (bone marrow or adipose tissue) | Reduced risk of rejection, personalized treatment |
| Allogeneic MSCs | Donor tissues | Immediate availability, consistent cell quality |
| Bone Marrow Aspirate Concentrate (BMAC) | Patient’s bone marrow | Mixture of stem cells and growth factors, promotes tissue repair |
| Adipose-Derived Stem Cells | Patient’s fat tissue | Accessible, regenerative capabilities |
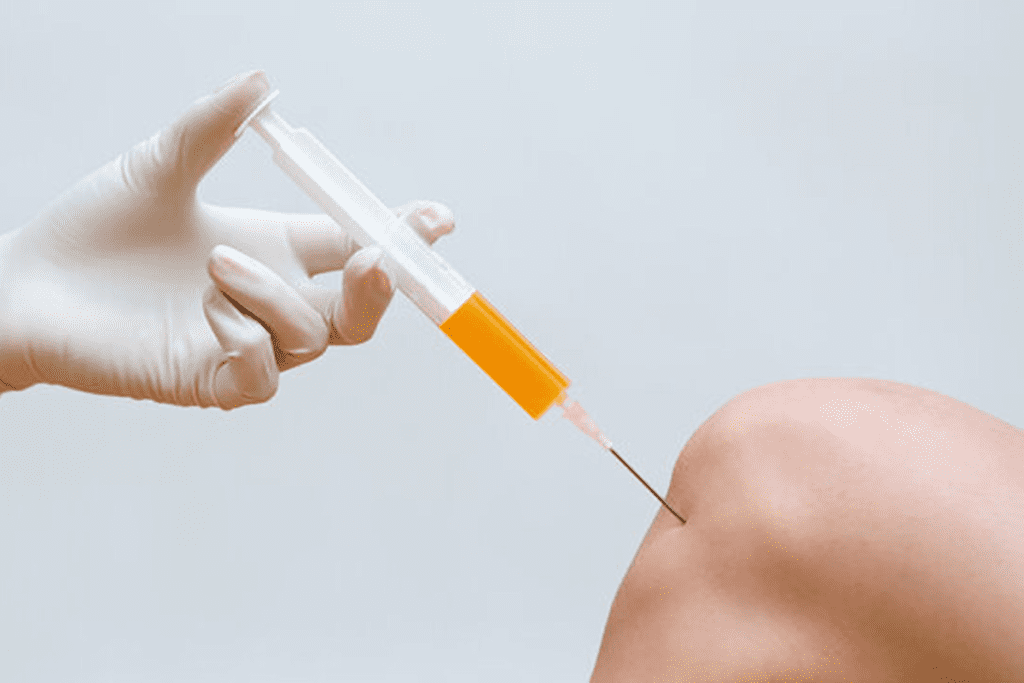
The Stem Cell Injection Procedure for Knees

Stem cell therapy for knee issues is a detailed process. It starts with preparation and ends with injecting stem cells. This method has shown to help with knee pain and repair cartilage.
Pre-Procedure Preparation
Before getting stem cell injections knee, patients go through a detailed check-up. They review their medical history and assess knee damage. They also do lab tests. Preparation is key to ensuring the best possible outcomes.
Harvesting and Processing Methods
The procedure starts by taking stem cells from the patient’s own body. This can be from bone marrow or fat tissue. The cells are then processed to make them more concentrated. Advanced processing techniques are used to ensure the quality and potency of the stem cells.
Injection Techniques and Guidance
The stem cells are injected into the knee joint under imaging guidance. This ensures they are placed correctly. Precise injection techniques are critical for the best results. Most patients find the procedure comfortable.
Post-Procedure Care and Recovery
After the injection, patients get advice on care to help with recovery. They might need to avoid hard activities and follow a rehabilitation plan. Proper post-procedure care can significantly influence the overall success of the treatment.
Experts say, “The success of stem cell therapy for knee osteoarthritis depends not only on the procedure itself but also on the care before, during, and after.”
“Stem cell therapy represents a promising approach for the treatment of knee osteoarthritis, with benefits in pain reduction and functional improvement.”
” Expert Opinion on Stem Cell Therapy
Clinical Evidence: Efficacy of MSC Injections for Knee Osteoarthritis
Knee osteoarthritis treatment is changing with MSC injections. The medical world is looking into new ways to treat this condition. Mesenchymal stem cells (MSCs) are being studied for their ability to repair cartilage and reduce inflammation.
Review of Major Clinical Trials
Many clinical trials have looked into MSC injections for knee osteoarthritis. They’ve used different types of MSCs and dosages. This helps us understand how well MSC injections work.
A study in the Journal of Orthopaedic Research showed MSC injections can help. Patients with knee osteoarthritis felt less pain and had better knee function after treatment.
Meta-Analysis Results for MSC Knee Treatments
Meta-analyses combine data from several trials. This gives us a clearer picture of MSC injections’ benefits. A study in Arthroscopy found MSC therapy improved pain and function in knee osteoarthritis patients.
| Study | MSC Source | Outcome Measures | Results |
| Study A | Autologous BM-MSCs | VAS, WOMAC | Significant improvement in pain and function |
| Study B | Allogeneic UC-MSCs | KOOS, MRI | Improved cartilage quality and reduced pain |
| Study C | Adipose-derived MSCs | IKDC, SF-36 | Enhanced functional outcomes and quality of life |
Outcomes for Different Knee Conditions
MSC injections work differently for each knee condition. Early-stage osteoarthritis patients might see more benefits than those with advanced disease.
Studies also look at combining MSC injections with other treatments like PRP therapy. This could improve results even more.
Limitations of Current Research
Even though the research looks promising, there are some issues. Different study methods and limited long-term data are concerns. Also, more diverse patient groups are needed.
Fixing these problems is key to fully understanding MSC injections’ role in treating knee osteoarthritis.
Potential Benefits of Stem Cell Therapy for Knee Regeneration
Stem cell therapy for knee regeneration offers many benefits. It gives hope to those with knee osteoarthritis and other knee problems.
Pain Reduction Capabilities
One key benefit is pain reduction. Studies show stem cell injections knee can lower pain in knee osteoarthritis patients.
Stem cells may work by reducing inflammation. This can significantly reduce knee pain.
Anti-Inflammatory Effects
Stem cell therapy also has anti-inflammatory effects. This can help with knee osteoarthritis inflammation.
By lowering inflammation, it creates a better healing environment in the knee.
Cartilage Repair Potencial
Another benefit is cartilage repair. Stem cells can turn into chondrocytes, helping repair damaged cartilage.
Functional Improvement Outcomes
Stem cell therapy also improves function. Patients with knee osteoarthritis often see better daily activity performance.
They can move better and perform tasks more easily. This improves their quality of life.
- Improved mobility
- Enhanced knee function
- Better overall quality of life
Safety Considerations of MSC Injections for Knee Pain Therapy
The safety of MSC injections for knee pain is a complex topic. As more people use them, knowing their safety is key for doctors and patients.
Common Side Effects
Most people find MSC injections safe, with few side effects. These can include:
- Temporary pain or discomfort at the injection site
- Mild swelling or bruising
- Headache or fatigue
Long-Term Safety Profile
Research on MSC injections’ long-term safety is ongoing. Early studies show they are well-tolerated. But, more research is needed to know all risks.
Regulatory Concerns and FDA Status
In the U.S., the FDA watches over MSC injections. Some are cleared for use, while others are not. It’s important for patients to know the product’s status.
Choosing Qualified Providers
Finding a skilled doctor is key for safe MSC injections. Look for doctors who:
- Know how to use MSC therapy for knee issues
- Use FDA-approved MSC products
- Follow strict clean injection methods
- Give clear instructions before and after treatment
Choosing the right doctor can lower risks and make treatment safer.
In summary, MSC injections are mostly safe for knee pain. But, it’s important to know about side effects, long-term safety, and rules. By picking the right doctor and staying informed, patients can make smart choices for their care.
Comparing Stem Cell Injections to Alternative Knee Treatments
When looking at treatments for knee osteoarthritis, it’s key to compare stem cell injections knee with other options. Knee osteoarthritis affects millions, causing pain and stiffness. Many treatments aim to ease symptoms and slow the disease.
Corticosteroid Injections
Corticosteroid injections are a common choice for knee osteoarthritis. They offer quick relief by reducing inflammation. But, long-term use can harm cartilage and cause side effects. Stem cell injections knee, on the other hand, aim to repair tissue and offer longer benefits.
Hyaluronic Acid (Viscosupplementation)
Hyaluronic acid injections help by adding to the knee’s natural lubrication. They can ease pain for some, but their success varies. Stem cell therapy, by contrast, aims to regenerate cartilage, tackling the disease’s root cause.
Platelet-Rich Plasma (PRP)
PRP therapy uses the patient’s own blood to create growth factor-rich plasma. Injected into the knee, it stimulates healing. While promising, its effectiveness compared to stem cell injections knee is under study. Both treatments aim to boost the body’s healing, but in different ways.
Surgical Options
Surgery, like knee replacement, is considered when other treatments fail. It can be effective but comes with risks and a long recovery. Stem cell injections knee offer a less invasive option, aiming to delay or avoid surgery.
In summary, many treatments exist for knee osteoarthritis, each with its own benefits and drawbacks. Stem cell injections knee are a promising option, focusing on repairing and regenerating tissue. By comparing these, patients and doctors can choose the best treatment plan.
Conclusion: Making an Informed Decision About Stem Cell Treatment for Knees
Patients thinking about stem cell injections knee osteoarthritis need to look at both sides. The treatment might help with pain and fix cartilage. But, how well it works can change based on the stem cells used and the patient’s health.
To make a smart choice, patients should look at the research and talk to a doctor. They should know about the different stem cell types and what they can do for knee problems.
Looking at the latest studies and trials helps patients understand stem cell injections better. This way, they can decide if this treatment is good for them.
FAQ
What is stem cell therapy for knee osteoarthritis?
Stem cell therapy for knee osteoarthritis is a treatment. It involves injecting stem cells into the knee. This helps repair cartilage and reduce inflammation.
How do MSC injections work for knee osteoarthritis?
MSC injections introduce mesenchymal stem cells into the knee. These cells can turn into cartilage cells. They help repair tissue.
What are the different types of stem cell therapies available for knee conditions?
There are several stem cell therapies for knee conditions. These include autologous stem cells and allogeneic MSCs. Bone marrow aspirate concentrate (BMAC) and adipose-derived stem cells are also options.
What is the stem cell injection procedure for knees?
The procedure starts with harvesting stem cells from bone marrow or fat tissue. The cells are then processed and injected into the knee. This is done under guidance.
Are stem cell injections knee osteoarthritis safe?
Yes, stem cell injections are generally safe. But, they can cause side effects like pain, swelling, or infection at the injection site.
How effective are MSC injections for knee osteoarthritis?
MSC injections show promise in treating knee osteoarthritis. They can reduce pain and improve function. But, results vary based on the individual and the condition’s severity.
What are the benefits of stem cell therapy for knee regeneration?
Stem cell therapy offers several benefits. It can reduce pain, have anti-inflammatory effects, and repair cartilage. It also improves knee function.
How do stem cell injections compare to alternative knee treatments?
Stem cell injections offer a regenerative approach. This is different from treatments like corticosteroid injections or hyaluronic acid. The best treatment depends on the patient’s needs.
What are the regulatory concerns surrounding MSC injections for knee pain therapy?
Regulatory concerns include FDA approval and ensuring stem cell quality and safety. It’s important to follow good manufacturing practices.
How can I choose a qualified provider for stem cell injections?
Look for a doctor with experience in stem cell therapy. Check their credentials and ensure they use high-quality stem cells. They should follow proper protocols.
What is the role of autologous stem cells in knee osteoarthritis treatment?
Autologous stem cells come from the patient’s own tissue. They can help repair cartilage and reduce inflammation in knee osteoarthritis.
Can stem cell injections regenerate cartilage in the knee?
Yes, stem cell injections can promote cartilage repair and regeneration. But, the extent of regeneration varies based on individual factors.
References
- Efficacy of a single intra-articular injection of mesenchymal stem cells for knee osteoarthritis: a dose-focused meta-analysis of randomized controlled trials. Journal of Orthopaedic Surgery and Research, 20, Article 190. (2025). https://doi.org/10.1186/s13018-025-06190-4
- Shoukrie, S. I., Venugopal, S., Dhanoa, R. K., Selvaraj, R., Selvamani, T. Y., Zahra, A., ¦ & et al. (2022). Safety and efficacy of injecting mesenchymal stem cells into a human knee joint to treat osteoarthritis: a systematic review. Journal of Research in Medical Sciences. https://pubmed.ncbi.nlm.nih.gov/35693367/
- Stem Cell Research & Therapy. (2025). Efficacy and safety of mesenchymal stem cells in knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials, 16, Article 122. https://doi.org/10.1186/s13287-025-04252-2
- Intra-articular mesenchymal stromal cell injections are no different from placebo in the treatment of knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy, 36(3), (2020). MD vs placebo. https://pubmed.ncbi.nlm.nih.gov/33098949/ PubMed
- Lee, W. C., et al. (2019). Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a Phase IIb, randomized, placebo-controlled clinical trial. STEM CELLS Translational Medicine, 8(7), 696-706. https://doi.org/10.1002/sctm.18-0122 Stem Cells Journal