Upper airway obstruction is a serious issue in pediatric patients. It happens when the airways get blocked or narrowed. This makes it hard for kids to breathe.

In pediatric patients, this problem can be very dangerous. It can cause a lot of harm and even death if not treated right. At LivHospital, we aim to give top-notch care to kids. We focus on managing airway problems, including stertor—a harsh, snoring-like sound due to airway obstruction—in a team effort to ensure the best outcomes.
Spotting this problem early and acting fast is key. It helps save kids from serious health issues.
It’s important to know how the pediatric airway is different from the adult airway. This knowledge helps in diagnosing and treating upper airway obstruction in kids. The main difference is that kids are more likely to have blockages.
The pediatric airway has unique features. Kids have larger heads and a larger occiput. This can cause the airway to bend when they lie down.
They also have a larger tongue and smaller mandibles than adults. These traits make their airway narrower, increasing the risk of blockage.
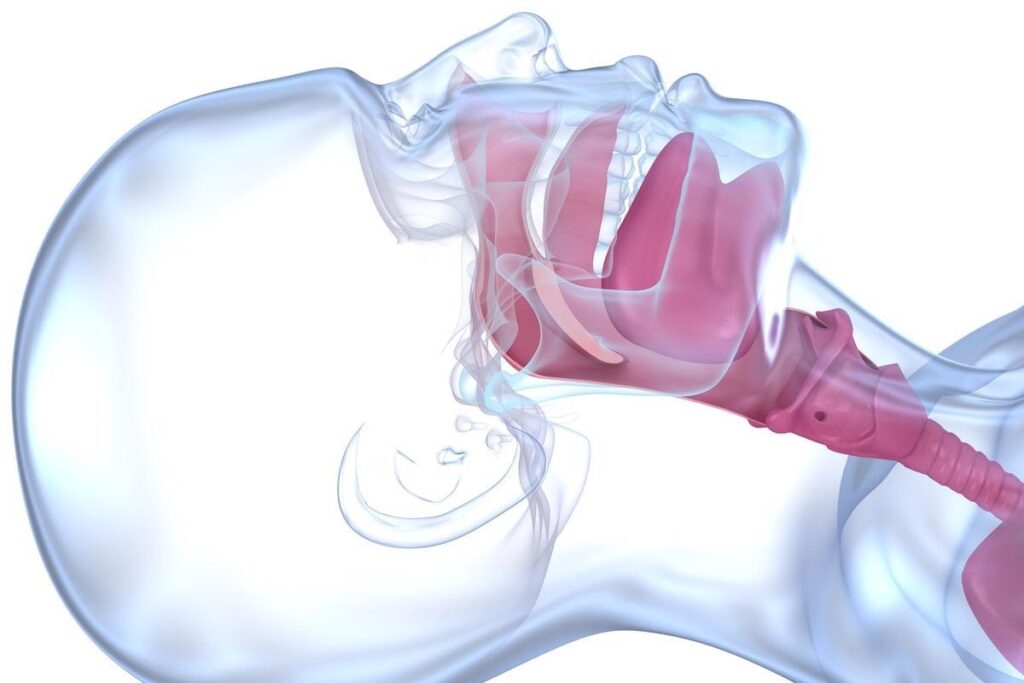
Children’s anatomy and other factors make them more at risk for airway blockage. For example, their larger tongue can block the airway, more so when they’re lying down. Also, their airway is smaller, so even a small blockage can cause big problems.
Healthcare providers need to understand these differences. This knowledge helps them give the right care to kids with airway blockages.
In kids, foreign body aspiration is a big problem. It’s most common in children aged 4-7. They love to explore by putting things in their mouths.

In 2000, the CDC reported 160 kids under 15 died from choking. There were also 17,537 emergency visits for nonfatal choking. These numbers show how serious foreign body aspiration is for young kids.
Food is a big choking hazard for kids. Nuts, seeds, and popcorn are very dangerous because they can get stuck in the airway. Foods like hot dogs and grapes are also risky because they can fit into the airway shape.
Toys and objects can also cause choking. Balloons are a big cause of choking deaths in kids. The latex in balloons can fit into the airway, leading to fatal blockages. Other toys with small parts or detachable parts are also dangerous.
Knowing these dangers helps us prevent choking in kids. We can do this by watching them during meals, avoiding dangerous foods, and making sure toys are safe and right for their age.
We see adenotonsillar hypertrophy as a main cause of upper airway blockage in kids. It’s when the tonsils and adenoids get too big. This can cause big problems with breathing.
It can also cause obstructive sleep apnea. This is when breathing stops or gets very shallow while sleeping. It messes up sleep and can lower oxygen levels. This affects a child’s health and growth.
Obstructive sleep apnea (OSA) from adenotonsillar hypertrophy is very serious. It messes up sleep quality and has bigger health issues. Kids with OSA might:
A study shows kids with adenotonsillar hypertrophy are more likely to get OSA. This can harm their heart and brain if not treated.
This condition shows why early diagnosis and treatment are key.
Adenotonsillectomy, or removing tonsils and adenoids, is a common fix. It helps kids with adenotonsillar hypertrophy and OSA a lot.
Studies show adenotonsillectomy is done in 19-118 kids per 10,000. Most kids see big improvements after the surgery. They sleep better and feel healthier.
By fixing adenotonsillar hypertrophy with adenotonsillectomy, we can make kids’ lives better. We help them with sleep apnea and other breathing problems.
It’s key for healthcare providers to spot airway obstruction signs early. If not treated quickly, it can lead to serious problems. We’ll look at stertor and stridor, and other signs of severe airway blockage.
Stertor is a noisy breathing sound above the larynx. It’s linked to upper airway blockage. Listen for a low-pitched snore or snort during breathing in. This sound is distinct from stridor, which is higher and linked to lower airway blockage.
Key characteristics of stertor include:
Knowing the difference between stertor and stridor is key for diagnosing airway issues. Both show respiratory distress, but at different levels. Stridor is a high-pitched sound from laryngeal or sub-laryngeal blockage. Stertor is from blockage above the larynx.
“The distinction between stertor and stridor is vital for accurate diagnosis and treatment of airway obstruction.” –
Medical Expert
Other signs of severe airway blockage include:
Spotting these signs early can help prevent serious issues. As healthcare providers, we must be alert and act fast to manage airway blockage.
Other than well-known causes, infections, allergic reactions, and congenital issues can also block the upper airway. It’s important to understand these causes for proper diagnosis and treatment.
Infections are a big reason for upper airway blockage in kids. Viral laryngotracheobronchitis (croup) is a common cause. We also see less common but serious infections like epiglottitis and bacterial tracheitis that need quick medical help.
Allergic reactions, like anaphylaxis, can cause sudden and severe blockage of the upper airway. Anaphylaxis is a serious condition that needs immediate treatment with epinephrine. Common allergens include peanuts, tree nuts, fish, shellfish, milk, eggs, wheat, and soy.
Congenital issues can also cause upper airway blockage. Conditions like laryngomalacia and subglottic stenosis are examples. These often need careful management and sometimes surgery to fix the blockage.
When dealing with upper airway blockage in kids, we must consider these causes for the right care.
Airway obstruction in children needs quick diagnosis and emergency management. We will look at how to diagnose airway blockage and the emergency steps to manage it.
Diagnosing airway obstruction starts with a detailed history and physical exam. We use tools like flexible laryngoscopy to see the airway and check the blockage. X-rays and CT scans help find the cause and where it is.
Flexible laryngoscopy is key because it lets us see the larynx directly. It can be done in a clinic without general anesthesia. This helps find problems like big tonsils or foreign bodies.
For acute airway obstruction, first aid is vital. For choking kids, back slaps or the Heimlich maneuver can save lives. If they can, they should cough to try and get the object out.
For severe blockage or when first aid doesn’t work, medical help is needed fast. This might include endotracheal intubation or surgery. Doctors must act quickly to open the airway and make sure the child gets enough oxygen.
Good emergency management of airway obstruction needs teamwork from healthcare teams. Knowing how to diagnose and treat helps save children’s lives.
It’s key to know why upper airway obstruction happens in kids to stop it early. We need to teach parents and caregivers about choking dangers and airway block signs.
Preventing upper airway blockage means knowing the risks. This includes choking on objects, big tonsils, and other causes. Spotting severe blockage signs like stertor and stridor is critical for quick doctor visits.
At LivHospital, we urge parents to act fast if their child’s airway is blocked badly. We aim to give top-notch care and support to international patients. Being alert and informed helps prevent blockages and ensures kids get help when they need it.
Upper airway obstruction in kids is a serious issue. It happens when the airway gets blocked. This can be very dangerous if not treated right away.
Main causes include swallowing something they shouldn’t, big tonsils or adenoids, infections like croup, allergies, and some birth defects.
Stertor sounds like a low rumble and happens when something blocks the airway near the nose or mouth. Stridor is a high-pitched sound that means something is blocking the larynx or trachea.
Signs include trouble breathing, sounds like stertor or stridor, not being able to speak or cough. In very bad cases, a child might lose consciousness or turn blue.
To manage big tonsils and adenoids, doctors might remove them. This surgery can help with sleep problems and other symptoms.
First aid for a blockage includes back slaps or the Heimlich maneuver for kids over one. For babies under one, use back slaps and chest thrusts. If the child stops breathing, start CPR.
To prevent blockages, keep small things away from kids. Avoid giving them nuts or popcorn. Make sure toys are safe and don’t have small parts.
Doctors use clinical checks, X-rays, or CT scans to find blockages. Sometimes, they do a laryngoscopy or a bronchoscopy to see the airway directly.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us