
Sleep apnea is a serious condition that affects millions worldwide. It causes interruptions in breathing during sleep. This significantly impacts health and quality of life. Effective treatment is key to managing this condition.
The Sleep Foundation says sleep apnea affects 2% to 9% of adults in the U.S. We will look at different treatment options. This includes CPAP therapy and Inspire Upper Airway Stimulation. These can help you understand how to fix sleep apnea and improve your well-being.
The term “surgical cpap” often refers to the Inspire implant. Learn how it and other methods can fix sleep apnea.

Sleep apnea is a condition where breathing stops during sleep. It has many types and serious health effects if not treated. Knowing the different types, causes, and health risks is key to managing it well.
Sleep apnea is a sleep disorder that causes breathing pauses during sleep. These pauses, or apneas, can happen many times a night. They lead to poor sleep and low blood oxygen levels. Sleep apnea can greatly affect a person’s life and health.
There are three main types of sleep apnea: Obstructive Sleep Apnea (OSA), Central Sleep Apnea, and Complex Sleep Apnea.
Many factors can raise the risk of sleep apnea. These include obesity, age, neck size, and certain health conditions. Knowing these risk factors is key for prevention and early diagnosis.
Some common risk factors are:
Untreated sleep apnea can lead to serious health problems. These include heart disease, diabetes, and brain function issues. Getting a diagnosis and treatment early is very important.
The health risks include:
Healthcare professionals use several tools to diagnose sleep apnea. This is key to finding the right treatment.
Polysomnography (PSG) is a main tool for diagnosing sleep apnea. It tracks heart rate, lung activity, and brain waves while you sleep. PSG can be done in a lab or at home.
Home sleep apnea testing (HSAT) is a simpler option for some. It uses portable devices to record breathing and oxygen levels. Though not as detailed as PSG, it’s good for diagnosing OSA in certain cases.
The Apnea-Hypopnea Index (AHI) and Respiratory Disturbance Index (RDI) show how severe sleep apnea is. AHI counts apneas and hypopneas per hour. RDI includes more disturbances. These help doctors decide on treatment.
If you snore loudly, stop breathing during sleep, or feel very tired during the day, see a doctor. Early treatment can greatly improve your life and prevent health problems.
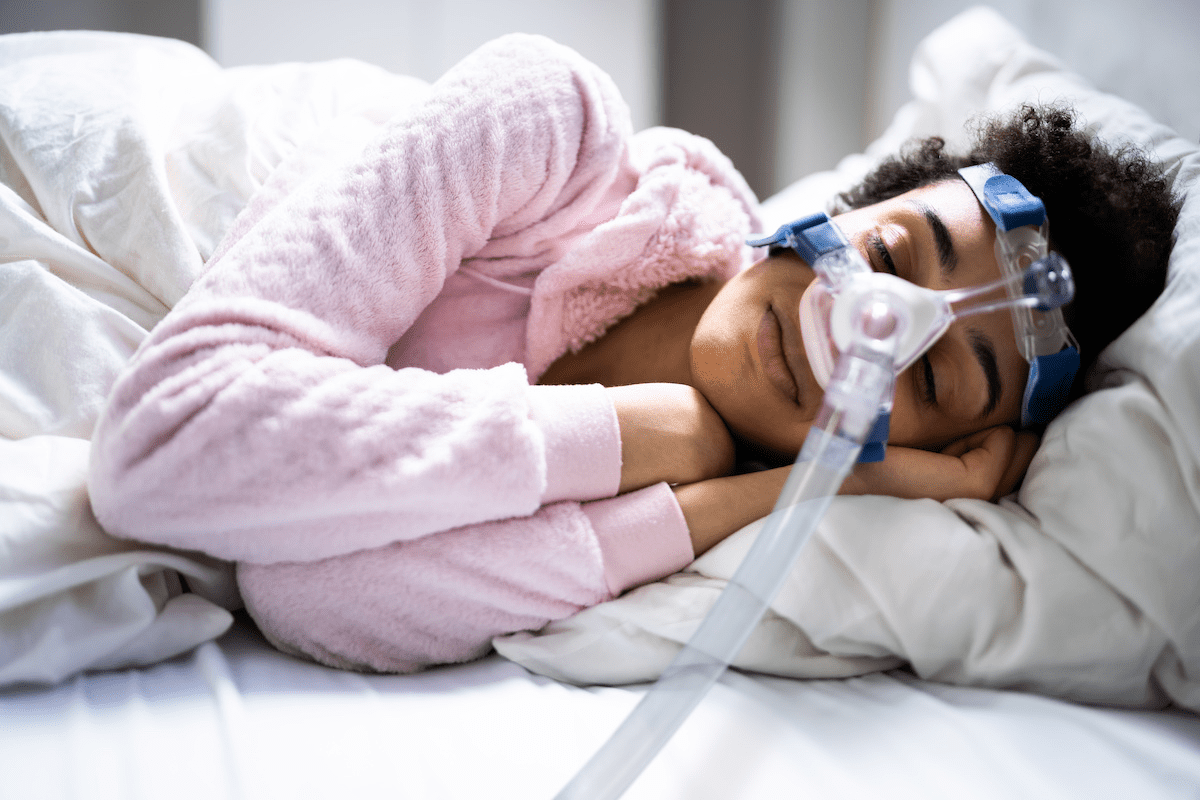
Millions of people with sleep apnea find relief in CPAP therapy. It’s a treatment where you wear a mask over your nose and/or mouth while sleeping. This mask connects to a machine that sends air, keeping your airway open and reducing apneic events.
CPAP machines send a steady flow of air through the mask. This keeps your airway open during sleep. The air pressure is set based on a sleep study, making sure it’s right for you.
Key Components of CPAP Therapy:
There are many CPAP devices and masks for different needs. Here are some common ones:
Device/Mask Type | Description | Benefit |
Nasal CPAP Mask | Covers the nose | Ideal for patients who breathe through their nose |
Full-Face CPAP Mask | Covers both the nose and mouth | Suitable for patients who breathe through their mouth during sleep |
Nasal Pillow CPAP Mask | Small prongs that fit into the nostrils | Less intrusive, ideal for patients with claustrophobia |
Auto-Adjusting CPAP (APAP) | Automatically adjusts pressure throughout the night | Provides the minimum pressure required to keep the airway open, improving comfort |
Setting up a CPAP machine takes a few steps. You need to fit the mask, adjust the pressure, and calibrate the machine. It’s important to work with your healthcare provider to get it right.
“The key to successful CPAP therapy lies in proper fitting and adjustment. Patients should work closely with their healthcare provider to ensure the best possible outcome.” – Medical Expert, Sleep Specialist
CPAP therapy can greatly reduce apnea events and improve sleep quality. Studies show it can also improve daytime functioning and reduce sleep apnea symptoms. It lowers the risk of health problems too.
CPAP therapy works well for most people. Knowing how it works and the different options can help you get the most out of it.
CPAP therapy is very effective but can be tough for some due to discomfort. Up to 50% of users face skin issues, and others get ear or sinus discomfort. It’s key to tackle these problems to boost compliance and treatment success.
Many users find CPAP uncomfortable because of mask fit, dryness, or machine noise. Trying different masks or sizes can help with fit. A humidifier can reduce dryness, and quieter machines can lessen disturbance.
“I’ve seen many patients struggle with CPAP due to mask discomfort,” says Medical Expert, a sleep specialist. “By working with a healthcare provider to adjust the mask and settings, users can significantly improve their comfort and compliance.”
Finding the right mask is key for comfort. Consider mask type, size, and material. A good fit should not leak or cause sores. Users can get help from healthcare providers or CPAP suppliers to find the best mask.
Adjusting humidity and pressure can greatly improve comfort. Start by tweaking humidity to avoid dryness. Adjust pressure to ensure it’s right for keeping the airway open without too much pressure.
Keeping CPAP equipment clean and well-maintained is vital. Wash masks and tubing with mild soap and water, then dry them well. Clean the machine with a damp cloth, and replace filters as recommended.
By following these tips and working with healthcare providers, CPAP users can beat common challenges and sleep better.
The Inspire Upper Airway Stimulation system is changing how we treat sleep apnea. It gives hope to those who can’t use CPAP therapy. Many find CPAP machines uncomfortable or hard to stick with.
The Inspire Sleep Device is a small, implanted device for sleep apnea treatment. It sends gentle electrical pulses to the tongue. This keeps the airway open while you sleep.
Inspire Sleep Therapy uses a small device to stimulate the tongue’s movement. This helps keep the airway open. It reduces sleep apnea events.
To get the Inspire implant, you need to meet certain criteria. You must have moderate to severe sleep apnea. You should also not be significantly overweight and have the right airway anatomy.
Candidacy Criteria | Description |
Severity of Sleep Apnea | Moderate to severe |
Body Mass Index (BMI) | Less than 32 (varies by criteria) |
Airway Anatomy | Suitable for Inspire therapy |
The procedure to implant the Inspire device is done under general anesthesia. It takes a few hours. Recovery time is short, and most can get back to normal in a week.
Key Benefits of Inspire Upper Airway Stimulation:
The Inspire Upper Airway Stimulation system is a game-changer for sleep apnea. It greatly improves sleep quality and overall health for those with moderate to severe obstructive sleep apnea (OSA).
Learning to use the Inspire remote control is key. It lets patients control the device, adjust settings, and check battery life. Using the remote correctly is vital for getting the most from Inspire therapy.
Research shows Inspire therapy cuts Apnea-Hypopnea Index (AHI) scores and boosts quality of life for those with OSA. Clinical trials show high success rates, with many patients seeing a big drop in sleep apnea symptoms. A study in the New England Journal of Medicine found AHI scores fell by 68% on average.
“The Inspire device has changed my life. I no longer wake up multiple times a night, and I feel more energized throughout the day.” – Patient testimonial
The Inspire device is built to last, with a battery life of 8 to 11 years. Regular check-ups with a healthcare provider are key to keeping the device working well and planning for battery replacement.
Patients with the Inspire implant need ongoing care for the best results. This includes regular appointments to adjust settings, monitor progress, and address any issues. Good follow-up care is essential for the best outcomes with Inspire therapy.
For those who can’t handle CPAP therapy, surgery might be a good option. Sleep apnea is different for everyone. If CPAP doesn’t work, surgery could help a lot.
UPPP is a surgery that removes extra tissue in the throat. It makes the airway wider. This helps with sleep apnea by reducing blockages.
MMA is a more serious surgery. It moves the upper and lower jaws to make the airway bigger. It’s good for those with severe sleep apnea and certain jaw shapes.
This method implants a device that keeps the tongue from blocking the airway. It’s great for those who can’t use CPAP or other treatments.
Choosing between surgery and CPAP depends on the benefits and risks of each. Here’s a table comparing the surgeries with CPAP.
Treatment | Effectiveness | Invasiveness | Recovery Time |
CPAP | High | Non-invasive | Immediate |
UPPP | Moderate to High | Invasive | 2-4 weeks |
MMA | High | Highly Invasive | 6-8 weeks |
Hypoglossal Nerve Stimulation | Moderate to High | Invasive | 2-4 weeks |
Each surgery has its own good points and things to think about. Talking to a doctor is key to finding the right treatment for sleep apnea.
Oral appliances, like mandibular advancement devices, are a good treatment for sleep apnea. They move the lower jaw to keep the airway open. This helps reduce sleep apnea symptoms.
There are many types of oral appliances for sleep apnea. The most common are:
Oral appliances can be custom-made or bought over-the-counter. Custom-made devices fit better and work better. They are made by a dentist or healthcare provider.
Custom-made oral appliances have many benefits:
Oral appliances work best for mild to moderate sleep apnea. Their success depends on the severity and the device type. For severe cases, treatments like CPAP or Inspire Upper Airway Stimulation might be needed.
Oral appliances are usually well-tolerated. But, some people might feel jaw pain, tooth movement, or changes in bite. It’s important to see a healthcare provider regularly to adjust the device and avoid side effects.
Common side effects include:
Making simple changes to your daily habits can greatly improve sleep apnea. By making lifestyle changes, you can lessen sleep apnea episodes. We’ll look at key strategies for better sleep and health.
Keeping a healthy weight is key for managing sleep apnea. Extra weight, mainly around the neck, can block the airway during sleep. Weight loss can help many people with sleep apnea. A mix of diet changes and exercise is recommended for a healthy weight.
Eating a balanced diet with fruits, veggies, and whole grains helps with weight loss. It’s also wise to get advice from a healthcare provider or nutritionist for personal guidance.
Sleeping on your side can reduce sleep apnea episodes. Sleep position training helps you sleep on your side. Using pillows or special devices to stop rolling onto your back can work well.
There are many products and methods to help you sleep on your side. These include wedge pillows and wearable devices that vibrate when you roll onto your back.
Drinking alcohol and sedatives before bed can relax your throat muscles, raising the risk of airway blockage. Avoiding these substances before bed can lessen sleep apnea episodes.
Talking to your healthcare provider about medications is also important. They can help adjust your medication to reduce its impact on sleep.
Regular exercise can improve sleep quality and reduce sleep apnea. Exercise helps with weight management, heart health, and overall well-being.
Try moderate-intensity exercises like brisk walking, cycling, or swimming for at least 30 minutes a day. But avoid intense exercise before bed, as it can disrupt sleep.
The world of sleep apnea treatment is changing fast. New technologies and therapies are coming to meet the needs of patients. As we learn more about sleep disorders, we’re finding new ways to help people sleep better.
Scientists are looking into medicines to help with sleep apnea. They’re working on drugs that might fix the root causes of the problem. These include things like hypoglossal nerve stimulation helpers and drugs that control breathing better. These ideas are early, but they could be big steps forward.
Nasal EPAP devices are another new way to treat sleep apnea. They push air out during breathing, keeping the airway open. Some studies show they work well for people with mild to moderate sleep apnea. But, we need more research to know how good they really are.
Hypoglossal nerve stimulation is already helping people with sleep apnea. The newest versions are even better, with personalized therapy and longer battery life. These updates make the treatment more comfortable and effective for more people.
The future might bring treatments that use different methods together. For example, CPAP with hypoglossal nerve stimulation or oral appliances with EPAP devices. Early studies look promising, showing these combinations could work even better.
Looking ahead, sleep apnea treatment will keep getting better. With new research and ideas, patients will have more options that fit their needs. “The future of sleep apnea treatment is not just about managing the condition, but about finding a cure,” says Medical Expert, a leading researcher. New treatments bring hope to those with sleep apnea, and we’re excited to be part of this progress.
Central sleep apnea and complex sleep apnea are tough to diagnose and treat. They are different from obstructive sleep apnea. We’ll look at the special needs and treatment choices for these sleep disorders.
Inspire Upper Airway Stimulation (UAS) is mainly for obstructive sleep apnea (OSA). But, its use for central sleep apnea is being studied. Right now, Inspire is not usually suggested for central sleep apnea. This is because it works by opening the airway, which might not fix the brain’s breathing issues.
Adaptive Servo-Ventilation (ASV) is made for central and complex sleep apnea. It gives pressure support that changes with each breath. ASV is great for central sleep apnea because it can handle breathing changes well.
Bilevel Positive Airway Pressure (BiPAP) is another choice for central sleep apnea. It has two pressures: one for inhaling and a lower one for exhaling. BiPAP is good for complex sleep apnea because it can adjust to different pressure needs.
Complex sleep apnea mixes obstructive and central sleep apnea. Treatment might include CPAP, BiPAP, or ASV, along with lifestyle changes and medicine. It’s all about finding the right treatment for each person, which might mean trying different things.
Dealing with central and complex sleep apnea can be hard. But, with the right help and treatment options, people can manage their condition and live better.
Effective treatment of sleep apnea needs a plan made just for you. We team up with healthcare experts to craft a treatment plan that fits your needs and likes.
In this article, we’ve looked at many ways to treat sleep apnea. These include CPAP therapy, Inspire Upper Airway Stimulation, surgery, oral appliances, and changing your lifestyle. Each method has its own good points and things to think about.
When picking a treatment, we look at how bad your sleep apnea is, your overall health, and what you’re comfortable with. Knowing about all the options helps you make a smart choice about your care.
Creating a sleep apnea treatment plan is more than just picking a treatment. It also means getting ongoing support and making changes as needed. We urge patients to stay in touch with their healthcare team to keep an eye on their condition and adjust their plan if needed.
By taking a detailed and personalized approach to treating sleep apnea, we can greatly improve the lives of those with this condition. So, how to fix sleep apnea? It’s about finding the right mix of treatments and support.
The latest treatments for sleep apnea include Inspire Upper Airway Stimulation. It’s a device that keeps the airway open while you sleep. Other new options are advanced hypoglossal nerve stimulation systems, nasal EPAP, and new medicines.
Inspire therapy uses the hypoglossal nerve to control tongue and airway muscles. This keeps the airway open, reducing sleep apnea.
Inspire is mainly for obstructive sleep apnea (OSA). It might help with central sleep apnea in some cases. But, for central sleep apnea, treatments like ASV are often better.
To fight sleep apnea, try losing weight, change your sleep position, and avoid alcohol and sedatives. Exercise regularly too. There are also treatments like CPAP, Inspire, oral appliances, and surgery.
To use CPAP well, pick the right mask and adjust the pressure. Keep the device clean. If the mask is uncomfortable, try different types and adjust the fit.
There are many CPAP devices, like standard CPAP and APAP. Masks vary too, from nasal to full-face. Choose what fits you best.
There’s no single cure for sleep apnea. But, many treatments can help manage it. The best treatment depends on your specific case.
To stick with CPAP, focus on mask comfort and adjust the pressure. Keep the device clean. Use a humidifier, try different masks, and get help from doctors.
National Center for Biotechnology Information. (2025). How to Fix Sleep Apnea CPAP Inspire and. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2743098/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us