Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we know an irregular heartbeat can worry you. Tachycardia and bradycardia are when your heart beats too fast or too slow. This usually happens because of electrical problems in your heart.
Tachycardia means your heart beats too quickly, over 100 times a minute. Bradycardia is when it beats too slowly, under 60 times a minute. Both can be caused by electrical issues in the heart.
It’s important to know the difference between these heart rhythm problems. In this article, we’ll look at the symptoms, causes, and how to manage sinus bradycardia and tachycardia.
Key Takeaways
- Abnormal heart rates can be a sign of underlying conditions.
- Tachycardia and bradycardia are related to electrical abnormalities in heart rhythm.
- Understanding the symptoms and causes is key to effective management.
- Liv Hospital is dedicated to top-notch care and patient focus.
- Managing heart rhythm problems needs a full approach.
The Basics of Heart Rhythm and Rate
The heartbeat is controlled by an electrical system. Knowing this system helps us understand heart rhythm disorders. It makes sure the heart pumps blood well across the body.
How the Heart’s Electrical System Works
The heart’s electrical system starts with the sinoatrial (SA) node, the heart’s natural pacemaker. It sends signals to the atrioventricular (AV) node, and then to the bundle of His. This makes the heart muscle contract and pump blood. This pathway is key for a normal heart rhythm.
What Constitutes Normal Heart Rate
A normal heart rate is between 60 to 100 beats per minute (BPM). Things like age, fitness, and mood can change heart rate. For example, athletes often have a lower heart rate because they are more fit.
When Heart Rate Becomes Abnormal
When the heart rate is too fast (tachycardia) or too slow (bradycardia), it can cause symptoms. These include dizziness, fatigue, and shortness of breath. Conditions like bradycardia and tachycardia syndrome, or bradytachycardia or brady-tachy syndrome, happen when both occur. They make heart function harder to manage.
Knowing these basics is key to spotting when heart rhythm and rate are off. This lets us get medical help quickly.
Tachycardia and Bradycardia: Definition and Differences
Knowing about tachycardia and bradycardia is key to keeping your heart healthy. These heart rhythm issues can really affect your life.
What is Tachycardia? (Heart Rate Above 100 BPM)
Tachycardia means your heart beats too fast, over 100 BPM. You might feel palpitations, dizzy, or have trouble breathing. Doctors say it could mean you have a health problem that needs attention.
What is Bradycardia? (Heart Rate Below 60 BPM)
Bradycardia is when your heart beats too slow, under 60 BPM. It can make you feel dizzy, tired, or short of breath. Doctors say it’s normal in athletes but serious in others.
How These Conditions Affect Heart Function
Tachycardia and bradycardia both hurt your heart’s ability to pump blood. Tachycardia makes the heart less efficient. Bradycardia means your heart doesn’t circulate blood well enough.
Managing these conditions needs a full plan, including lifestyle changes and sometimes medicine. Knowing about tachycardia and bradycardia helps you take care of your heart.
Key Fact #1: Types of Tachycardia and Their Mechanisms
Tachycardia is a heart rate over 100 beats per minute (BPM). It has many forms, each with its own causes and effects. Knowing these differences is key to treating tachycardia.
Sinus Tachycardia: Normal Response vs. Pathological
Sinus tachycardia happens when the heart’s natural pacemaker fires too fast. This can be due to exercise, stress, or fever. But, it can also be caused by health issues like anemia or hyperthyroidism. It’s important to know the cause to treat it right.
Supraventricular Tachycardias
Supraventricular tachycardias (SVTs) start above the ventricles. They have abnormal electrical pathways. SVTs can start and stop suddenly. Treatment might include the Valsalva maneuver or catheter ablation.
Ventricular Tachycardia and Its Dangers
Ventricular tachycardia (VT) is dangerous and can lead to cardiac arrest. It happens when the ventricles have abnormal electrical activity. VT is often linked to heart disease. Quick medical help is needed, usually with cardioversion or medications.
| Type of Tachycardia | Characteristics | Common Causes |
|---|---|---|
| Sinus Tachycardia | Increased SA node firing rate | Exercise, stress, fever, anemia, hyperthyroidism |
| Supraventricular Tachycardia (SVT) | Abnormal electrical pathways above ventricles | AVNRT, AVRT, other reentrant circuits |
| Ventricular Tachycardia (VT) | Abnormal electrical activity in ventricles | Coronary artery disease, cardiomyopathy, electrolyte imbalances |
It’s vital for doctors to know about the different types of tachycardia. Each type needs a specific treatment plan. This helps in managing tachycardia effectively.
Key Fact #2: Types of Bradycardia and Their Mechanisms
It’s important to know the different types of bradycardia and what causes them. Bradycardia is when your heart beats too slow. Each type affects your heart and health in different ways.
Sinus Bradycardia: When It’s Normal vs. Concerning
Sinus bradycardia happens when the heart’s natural pacemaker, the SA node, beats slower than usual. It’s common in athletes or very fit people. But, in others, it might mean there’s a problem, like hypothyroidism or side effects from medication.
Heart Blocks: First, Second, and Third Degree
Heart blocks occur when electrical signals from the atria to the ventricles are delayed or blocked. They are divided into three degrees based on how severe the blockage is.
| Degree of Heart Block | Description | Symptoms and Implications |
|---|---|---|
| First Degree | Delayed electrical conduction | Often asymptomatic, may progress to higher degrees |
| Second Degree | Intermittent blocking of electrical impulses | May cause dizziness, fainting; can progress to third degree |
| Third Degree | Complete blockage of electrical impulses | Severe symptoms, including fainting, heart failure; requires pacemaker |
Sick Sinus Syndrome
Sick sinus syndrome is when the SA node doesn’t work right, causing irregular heartbeats. It can lead to bradycardia, tachycardia, or both (bradycardia-tachycardia syndrome).
Knowing about these bradycardia types is key for the right diagnosis and treatment. Each type has its own signs and what it means for your health.
Key Fact #3: Bradycardia-Tachycardia Syndrome Explained
Bradycardia-tachycardia syndrome is a complex heart condition. It causes the heart to switch between slow and fast rhythms. This makes it hard to diagnose and treat.
Understanding Brady-Tachyarrhythmia
Brady-tachyarrhythmia means the heart beats too slow and too fast. This back-and-forth can cause many symptoms. It’s not just about the heart rate; it’s about the heart’s electrical system not working right.
Prevalence and Demographics
This condition is more common in older adults. It gets more common with age, and heart disease is a big factor. It affects both men and women, but women might get it a bit more often.
| Age Group | Prevalence of Brady-Tachyarrhythmia |
|---|---|
| 60-69 years | 2.5% |
| 70-79 years | 5.1% |
| 80 years and above | 8.3% |
The Unique Challenges of Alternating Heart Rhythms
Managing this condition is tough because it’s so unpredictable. We need to tailor treatments carefully. This is because what works for one rhythm might not work for the other.
“The management of bradycardia-tachycardia syndrome requires a nuanced understanding of the condition’s complexities and a flexible treatment strategy.” – Cardiologist
In conclusion, bradycardia-tachycardia syndrome is a complex condition. It needs careful diagnosis and management. By understanding it better, we can help those living with it more effectively.
Key Fact #4: Recognizing Symptoms of Abnormal Heart Rates
It’s key to know the signs of abnormal heart rates early. Tachycardia and bradycardia show different symptoms, some mild, others serious.
Common Symptoms of Tachycardia
Tachycardia, when your heart beats over 100 times a minute, has many symptoms. You might feel:
- Palpitations or a rapid heartbeat feeling
- Dizziness or feeling lightheaded
- Shortness of breath
- Chest pain or discomfort
- Fainting or near-fainting spells
Common Symptoms of Bradycardia
Bradycardia, with a heart rate under 60 beats per minute, has its own symptoms. You might notice:
- Fatigue or feeling weak
- Dizziness or fainting
- Shortness of breath
- Chest pain
- Confusion or trouble concentrating
Warning Signs That Require Immediate Medical Attention
Some symptoms need you to see a doctor right away. These include:
Syncope and Pre-syncope
Fainting or near-fainting are serious signs. They mean you might have a heart problem.
Chest Pain and Shortness of Breath
Chest pain and hard breathing are urgent signs. They could mean a heart issue or something worse.
Seek medical help if you have these severe symptoms. Quick action can help a lot.
Pay attention to your body’s signs. Don’t wait to see a doctor if you’re worried.
Key Fact #5: Causes and Risk Factors of Heart Rate Abnormalities
Heart rate issues like tachycardia and bradycardia have many causes. Knowing these is key to diagnosing and treating them well.
Physiological vs. Pathological Causes
Physiological causes are normal responses, like a fast heart rate when exercising. Pathological causes, on the other hand, are linked to health problems. For example, veterno or Roemheld syndrome can cause heart rate problems due to stomach issues.
Genetic and Age-Related Factors
Genetics can make some people more likely to have heart issues. Age also plays a big role, as heart rate problems get more common with age. We need to think about these when we’re checking patients.
Medication-Induced Arrhythmias
Some medicines can cause heart rhythm problems, like tachycardia and bradycardia. It’s important to watch patients on these medicines, like beta-blockers.
Underlying Health Conditions
Many health issues can lead to abnormal heart rates. For example, thyroid problems, imbalances in electrolytes, and heart disease can all affect heart rhythm.
| Cause | Condition | Effect on Heart Rate |
|---|---|---|
| Genetic predisposition | Family history of heart conditions | Increased risk of tachycardia or bradycardia |
| Age | Aging | Increased risk of heart rate abnormalities |
| Medications | Beta-blockers, anti-arrhythmics | Can induce bradycardia or tachycardia |
| Underlying health conditions | Thyroid disorders, heart disease | Can cause tachycardia or bradycardia |
A medical expert said, “Finding and treating the root causes is key to fixing tachycardia and bradycardia.”
“Understanding the causes and risk factors is the first step to managing heart rate problems.”
Key Fact #6: Diagnosis and Treatment Approaches
Diagnosing and treating heart rhythm disorders needs a detailed plan. We use many tools and strategies to handle tachycardia and bradycardia well.
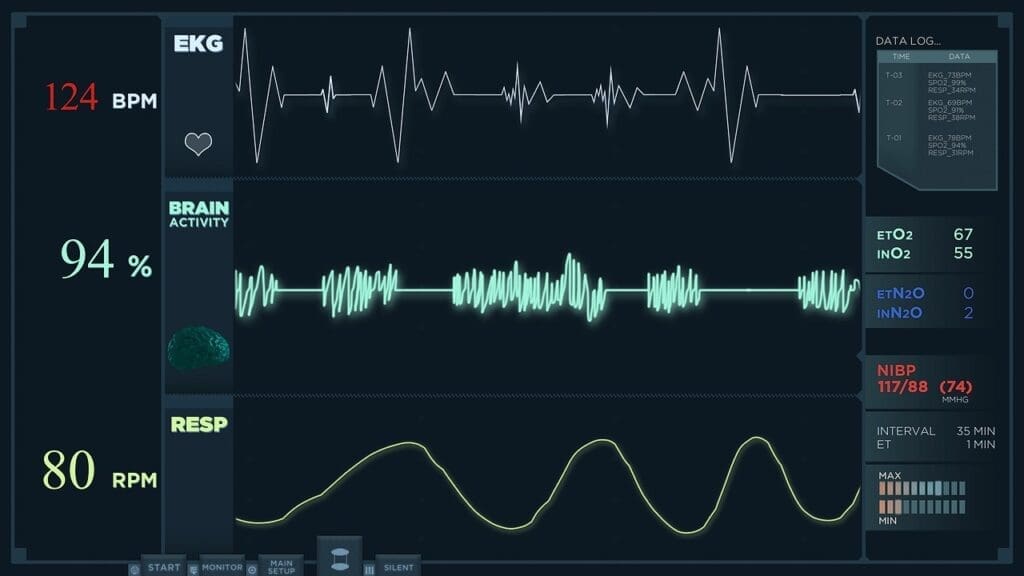
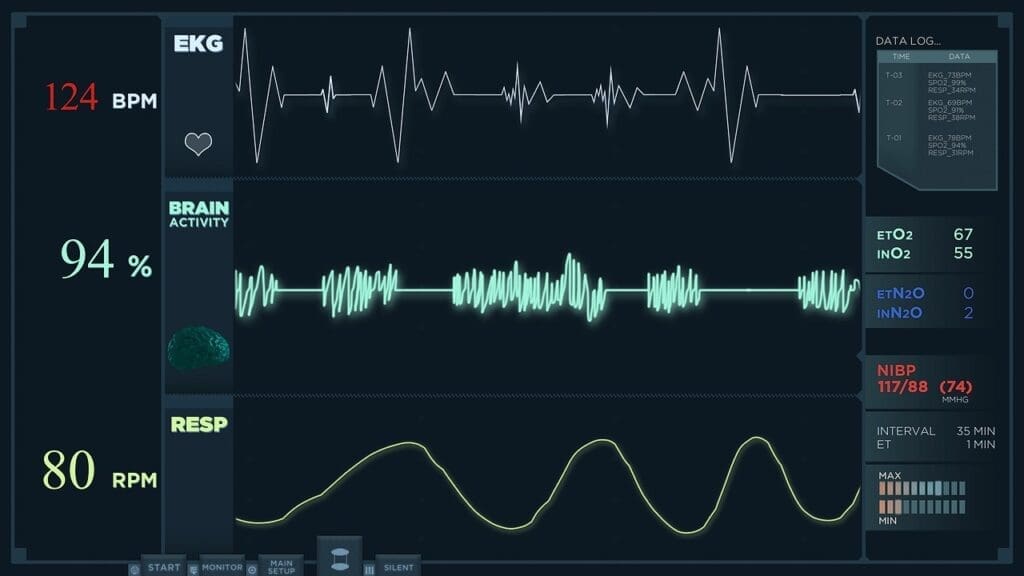
Diagnostic Methods: ECG, Holter Monitoring, and Beyond
Diagnosis starts with an electrocardiogram (ECG) to check the heart’s electrical activity. For symptoms that come and go, Holter monitoring over 24 to 48 hours gives more insight. Other tools include event monitors and electrophysiology studies.
Medical Treatments for Tachycardia
Treatment for tachycardia aims to control the heart rate and stop future episodes. Doctors often use beta-blockers and anti-arrhythmic drugs. Sometimes, catheter ablation is needed to destroy the bad electrical pathway.
Medical Treatments for Bradycardia
Bradycardia treatment varies based on the cause and how severe it is. For bradycardia that causes symptoms, a pacemaker is usually the best choice. Medications can help manage symptoms, but they’re not a lasting fix.
Interventional Procedures and Devices
Interventional procedures include catheter ablation for tachycardia and device implantation for both tachycardia and bradycardia.
Catheter Ablation
Catheter ablation uses energy to destroy the bad electrical pathway causing arrhythmia. It’s very effective for some types of tachycardia.
Pacemakers and Implantable Cardioverter-Defibrillators
Pacemakers help manage bradycardia by keeping the heart rate up. Implantable cardioverter-defibrillators (ICDs) can detect and fix dangerous tachycardia by giving an electric shock.
| Diagnostic/Treatment Method | Description | Condition Treated |
|---|---|---|
| ECG | Assesses heart’s electrical activity | Tachycardia, Bradycardia |
| Holter Monitoring | 24-48 hour heart monitoring | Intermittent arrhythmias |
| Catheter Ablation | Destroys abnormal electrical pathways | Tachycardia |
| Pacemaker | Ensures minimum heart rate | Bradycardia |
| ICD | Corrects life-threatening tachycardia | Tachycardia |
Key Fact #7: Living With and Managing Heart Rate Disorders
Living with tachycardia and bradycardia can be tough, but it’s doable. The right strategies help people stay active. It’s all about medical care, lifestyle changes, and keeping an eye on your heart.
Lifestyle Modifications
Healthy choices are key for managing heart issues. Eat well, exercise often, and handle stress. Stress-reducing activities like meditation or yoga can help avoid tachy and brady episodes.
- Eat a heart-healthy diet rich in fruits, vegetables, and whole grains.
- Engage in regular physical activity, such as walking or swimming, after consulting with your healthcare provider.
- Practice stress-reducing techniques like deep breathing or meditation.
Monitoring Your Heart Health at Home
Keeping an eye on your heart rate at home is important. Use a heart rate monitor or a smartwatch. This helps track your heart and spot any problems. For more info on cardiac rehab, check out cardiac rehabilitation resources.
When to Contact Your Healthcare Provider
Knowing when to get medical help is vital. If you feel dizzy, have chest pain, or can’t breathe, call your doctor right away. Regular visits are also important for managing brady and tachy conditions.
Long-term Prognosis and Quality of Life
The future looks different for everyone with heart rate disorders. It depends on the cause and how well you manage it. With the right treatment and lifestyle, many people with bradycardia and tachycardia live full lives. Staying in touch with your doctor is essential for a good quality of life.
Conclusion: Taking Control of Your Heart Health
Knowing about tachycardia and bradycardia is key to a healthy heart. We’ve covered the basics of these heart issues. This includes what they are, their symptoms, causes, and how to manage them.
Handling heart rate problems can make life better. Spotting the signs of tachycardia and bradycardia helps you get help when you need it. It’s important to watch over conditions like sinus bradycardia and tachycardia closely.
We urge you to play a big part in your heart health. Make lifestyle changes, keep an eye on your heart, and get medical help when it’s needed. This way, you can feel better and lower heart disease risks.
By understanding and managing tachycardia and bradycardia, you can control your heart health. It’s all about a mix of medical care and making healthy lifestyle choices.
FAQ
What is the difference between tachycardia and bradycardia?
Tachycardia is when your heart beats too fast, over 100 beats per minute. Bradycardia is when it beats too slow, under 60 beats per minute.
What are the symptoms of tachycardia?
Symptoms of tachycardia include a rapid pulse, dizziness, and shortness of breath. You might also feel palpitations.
What are the symptoms of bradycardia?
Symptoms of bradycardia include dizziness, fainting, and fatigue. You might also experience shortness of breath.
What is bradycardia-tachycardia syndrome?
Bradycardia-tachycardia syndrome, or brady-tachyarrhythmia, is when your heart switches between slow and fast rhythms. It’s challenging to diagnose and manage.
How are tachycardia and bradycardia diagnosed?
Doctors use electrocardiograms (ECG) and Holter monitoring to diagnose tachycardia and bradycardia. They also use other advanced tools.
What are the treatment options for tachycardia?
Treatments for tachycardia include medications and procedures like catheter ablation. Devices like implantable cardioverter-defibrillators are also used.
What are the treatment options for bradycardia?
For bradycardia, treatments include pacemakers and other devices to regulate the heart rate.
Can lifestyle modifications help manage heart rate disorders?
Yes, a healthy diet, regular exercise, and stress management can help manage heart rate disorders.
When should I contact my healthcare provider about my heart rate?
Contact your healthcare provider if you experience fainting, near-fainting, chest pain, or severe shortness of breath.
What is the long-term prognosis for individuals with tachycardia or bradycardia?
The long-term prognosis depends on the cause and management. With proper care, many can lead active lives.
What is sinus tachycardia?
Sinus tachycardia is when the heart rate is too fast due to stress or exercise. It’s a normal response.
What is sick sinus syndrome?
Sick sinus syndrome is when the sinoatrial node doesn’t work right. It leads to irregular heart rhythms.
Can certain medications cause heart rate abnormalities?
Yes, some medications can affect heart rate and cause tachycardia or bradycardia.
At Liv Hospital, we know an irregular heartbeat can worry you. Tachycardia and bradycardia are when your heart beats too fast or too slow. This usually happens because of electrical problems in your heart.
Tachycardia means your heart beats too quickly, over 100 times a minute. Bradycardia is when it beats too slowly, under 60 times a minute. Both can be caused by electrical issues in the heart.
It’s important to know the difference between these heart rhythm problems. In this article, we’ll look at the symptoms, causes, and how to manage sinus bradycardia and tachycardia.
Key Takeaways
- Abnormal heart rates can be a sign of underlying conditions.
- Tachycardia and bradycardia are related to electrical abnormalities in heart rhythm.
- Understanding the symptoms and causes is key to effective management.
- Liv Hospital is dedicated to top-notch care and patient focus.
- Managing heart rhythm problems needs a full approach.
The Basics of Heart Rhythm and Rate
The heartbeat is controlled by an electrical system. Knowing this system helps us understand heart rhythm disorders. It makes sure the heart pumps blood well across the body.
How the Heart’s Electrical System Works
The heart’s electrical system starts with the sinoatrial (SA) node, the heart’s natural pacemaker. It sends signals to the atrioventricular (AV) node, and then to the bundle of His. This makes the heart muscle contract and pump blood. This pathway is key for a normal heart rhythm.
What Constitutes Normal Heart Rate
A normal heart rate is between 60 to 100 beats per minute (BPM). Things like age, fitness, and mood can change heart rate. For example, athletes often have a lower heart rate because they are more fit.
When Heart Rate Becomes Abnormal
When the heart rate is too fast (tachycardia) or too slow (bradycardia), it can cause symptoms. These include dizziness, fatigue, and shortness of breath. Conditions like bradycardia and tachycardia syndrome, or bradytachycardia or brady-tachy syndrome, happen when both occur. They make heart function harder to manage.
Knowing these basics is key to spotting when heart rhythm and rate are off. This lets us get medical help quickly.
Tachycardia and Bradycardia: Definition and Differences
Knowing about tachycardia and bradycardia is key to keeping your heart healthy. These heart rhythm issues can really affect your life.
What is Tachycardia? (Heart Rate Above 100 BPM)
Tachycardia means your heart beats too fast, over 100 BPM. You might feel palpitations, dizzy, or have trouble breathing. Doctors say it could mean you have a health problem that needs attention.
What is Bradycardia? (Heart Rate Below 60 BPM)
Bradycardia is when your heart beats too slow, under 60 BPM. It can make you feel dizzy, tired, or short of breath. Doctors say it’s normal in athletes but serious in others.
How These Conditions Affect Heart Function
Tachycardia and bradycardia both hurt your heart’s ability to pump blood. Tachycardia makes the heart less efficient. Bradycardia means your heart doesn’t circulate blood well enough.
Managing these conditions needs a full plan, including lifestyle changes and sometimes medicine. Knowing about tachycardia and bradycardia helps you take care of your heart.
Key Fact #1: Types of Tachycardia and Their Mechanisms
Tachycardia is a heart rate over 100 beats per minute (BPM). It has many forms, each with its own causes and effects. Knowing these differences is key to treating tachycardia.
Sinus Tachycardia: Normal Response vs. Pathological
Sinus tachycardia happens when the heart’s natural pacemaker fires too fast. This can be due to exercise, stress, or fever. But, it can also be caused by health issues like anemia or hyperthyroidism. It’s important to know the cause to treat it right.
Supraventricular Tachycardias
Supraventricular tachycardias (SVTs) start above the ventricles. They have abnormal electrical pathways. SVTs can start and stop suddenly. Treatment might include the Valsalva maneuver or catheter ablation.
Ventricular Tachycardia and Its Dangers
Ventricular tachycardia (VT) is dangerous and can lead to cardiac arrest. It happens when the ventricles have abnormal electrical activity. VT is often linked to heart disease. Quick medical help is needed, usually with cardioversion or medications.
| Type of Tachycardia | Characteristics | Common Causes |
|---|---|---|
| Sinus Tachycardia | Increased SA node firing rate | Exercise, stress, fever, anemia, hyperthyroidism |
| Supraventricular Tachycardia (SVT) | Abnormal electrical pathways above ventricles | AVNRT, AVRT, other reentrant circuits |
| Ventricular Tachycardia (VT) | Abnormal electrical activity in ventricles | Coronary artery disease, cardiomyopathy, electrolyte imbalances |
It’s vital for doctors to know about the different types of tachycardia. Each type needs a specific treatment plan. This helps in managing tachycardia effectively.
Key Fact #2: Types of Bradycardia and Their Mechanisms
It’s important to know the different types of bradycardia and what causes them. Bradycardia is when your heart beats too slow. Each type affects your heart and health in different ways.
Sinus Bradycardia: When It’s Normal vs. Concerning
Sinus bradycardia happens when the heart’s natural pacemaker, the SA node, beats slower than usual. It’s common in athletes or very fit people. But, in others, it might mean there’s a problem, like hypothyroidism or side effects from medication.
Heart Blocks: First, Second, and Third Degree
Heart blocks occur when electrical signals from the atria to the ventricles are delayed or blocked. They are divided into three degrees based on how severe the blockage is.
| Degree of Heart Block | Description | Symptoms and Implications |
|---|---|---|
| First Degree | Delayed electrical conduction | Often asymptomatic, may progress to higher degrees |
| Second Degree | Intermittent blocking of electrical impulses | May cause dizziness, fainting; can progress to third degree |
| Third Degree | Complete blockage of electrical impulses | Severe symptoms, including fainting, heart failure; requires pacemaker |
Sick Sinus Syndrome
Sick sinus syndrome is when the SA node doesn’t work right, causing irregular heartbeats. It can lead to bradycardia, tachycardia, or both (bradycardia-tachycardia syndrome).
Knowing about these bradycardia types is key for the right diagnosis and treatment. Each type has its own signs and what it means for your health.
Key Fact #3: Bradycardia-Tachycardia Syndrome Explained
Bradycardia-tachycardia syndrome is a complex heart condition. It causes the heart to switch between slow and fast rhythms. This makes it hard to diagnose and treat.
Understanding Brady-Tachyarrhythmia
Brady-tachyarrhythmia means the heart beats too slow and too fast. This back-and-forth can cause many symptoms. It’s not just about the heart rate; it’s about the heart’s electrical system not working right.
Prevalence and Demographics
This condition is more common in older adults. It gets more common with age, and heart disease is a big factor. It affects both men and women, but women might get it a bit more often.
| Age Group | Prevalence of Brady-Tachyarrhythmia |
|---|---|
| 60-69 years | 2.5% |
| 70-79 years | 5.1% |
| 80 years and above | 8.3% |
The Unique Challenges of Alternating Heart Rhythms
Managing this condition is tough because it’s so unpredictable. We need to tailor treatments carefully. This is because what works for one rhythm might not work for the other.
“The management of bradycardia-tachycardia syndrome requires a nuanced understanding of the condition’s complexities and a flexible treatment strategy.” – Cardiologist
In conclusion, bradycardia-tachycardia syndrome is a complex condition. It needs careful diagnosis and management. By understanding it better, we can help those living with it more effectively.
Key Fact #4: Recognizing Symptoms of Abnormal Heart Rates
It’s key to know the signs of abnormal heart rates early. Tachycardia and bradycardia show different symptoms, some mild, others serious.
Common Symptoms of Tachycardia
Tachycardia, when your heart beats over 100 times a minute, has many symptoms. You might feel:
- Palpitations or a rapid heartbeat feeling
- Dizziness or feeling lightheaded
- Shortness of breath
- Chest pain or discomfort
- Fainting or near-fainting spells
Common Symptoms of Bradycardia
Bradycardia, with a heart rate under 60 beats per minute, has its own symptoms. You might notice:
- Fatigue or feeling weak
- Dizziness or fainting
- Shortness of breath
- Chest pain
- Confusion or trouble concentrating
Warning Signs That Require Immediate Medical Attention
Some symptoms need you to see a doctor right away. These include:
Syncope and Pre-syncope
Fainting or near-fainting are serious signs. They mean you might have a heart problem.
Chest Pain and Shortness of Breath
Chest pain and hard breathing are urgent signs. They could mean a heart issue or something worse.
Seek medical help if you have these severe symptoms. Quick action can help a lot.
Pay attention to your body’s signs. Don’t wait to see a doctor if you’re worried.
Key Fact #5: Causes and Risk Factors of Heart Rate Abnormalities
Heart rate issues like tachycardia and bradycardia have many causes. Knowing these is key to diagnosing and treating them well.
Physiological vs. Pathological Causes
Physiological causes are normal responses, like a fast heart rate when exercising. Pathological causes, on the other hand, are linked to health problems. For example, veterno or Roemheld syndrome can cause heart rate problems due to stomach issues.
Genetic and Age-Related Factors
Genetics can make some people more likely to have heart issues. Age also plays a big role, as heart rate problems get more common with age. We need to think about these when we’re checking patients.
Medication-Induced Arrhythmias
Some medicines can cause heart rhythm problems, like tachycardia and bradycardia. It’s important to watch patients on these medicines, like beta-blockers.
Underlying Health Conditions
Many health issues can lead to abnormal heart rates. For example, thyroid problems, imbalances in electrolytes, and heart disease can all affect heart rhythm.
| Cause | Condition | Effect on Heart Rate |
|---|---|---|
| Genetic predisposition | Family history of heart conditions | Increased risk of tachycardia or bradycardia |
| Age | Aging | Increased risk of heart rate abnormalities |
| Medications | Beta-blockers, anti-arrhythmics | Can induce bradycardia or tachycardia |
| Underlying health conditions | Thyroid disorders, heart disease | Can cause tachycardia or bradycardia |
A medical expert said, “Finding and treating the root causes is key to fixing tachycardia and bradycardia.”
“Understanding the causes and risk factors is the first step to managing heart rate problems.”
Key Fact #6: Diagnosis and Treatment Approaches
Diagnosing and treating heart rhythm disorders needs a detailed plan. We use many tools and strategies to handle tachycardia and bradycardia well.
Diagnostic Methods: ECG, Holter Monitoring, and Beyond
Diagnosis starts with an electrocardiogram (ECG) to check the heart’s electrical activity. For symptoms that come and go, Holter monitoring over 24 to 48 hours gives more insight. Other tools include event monitors and electrophysiology studies.
Medical Treatments for Tachycardia
Treatment for tachycardia aims to control the heart rate and stop future episodes. Doctors often use beta-blockers and anti-arrhythmic drugs. Sometimes, catheter ablation is needed to destroy the bad electrical pathway.
Medical Treatments for Bradycardia
Bradycardia treatment varies based on the cause and how severe it is. For bradycardia that causes symptoms, a pacemaker is usually the best choice. Medications can help manage symptoms, but they’re not a lasting fix.
Interventional Procedures and Devices
Interventional procedures include catheter ablation for tachycardia and device implantation for both tachycardia and bradycardia.
Catheter Ablation
Catheter ablation uses energy to destroy the bad electrical pathway causing arrhythmia. It’s very effective for some types of tachycardia.
Pacemakers and Implantable Cardioverter-Defibrillators
Pacemakers help manage bradycardia by keeping the heart rate up. Implantable cardioverter-defibrillators (ICDs) can detect and fix dangerous tachycardia by giving an electric shock.
| Diagnostic/Treatment Method | Description | Condition Treated |
|---|---|---|
| ECG | Assesses heart’s electrical activity | Tachycardia, Bradycardia |
| Holter Monitoring | 24-48 hour heart monitoring | Intermittent arrhythmias |
| Catheter Ablation | Destroys abnormal electrical pathways | Tachycardia |
| Pacemaker | Ensures minimum heart rate | Bradycardia |
| ICD | Corrects life-threatening tachycardia | Tachycardia |
Key Fact #7: Living With and Managing Heart Rate Disorders
Living with tachycardia and bradycardia can be tough, but it’s doable. The right strategies help people stay active. It’s all about medical care, lifestyle changes, and keeping an eye on your heart.
Lifestyle Modifications
Healthy choices are key for managing heart issues. Eat well, exercise often, and handle stress. Stress-reducing activities like meditation or yoga can help avoid tachy and brady episodes.
- Eat a heart-healthy diet rich in fruits, vegetables, and whole grains.
- Engage in regular physical activity, such as walking or swimming, after consulting with your healthcare provider.
- Practice stress-reducing techniques like deep breathing or meditation.
Monitoring Your Heart Health at Home
Keeping an eye on your heart rate at home is important. Use a heart rate monitor or a smartwatch. This helps track your heart and spot any problems. For more info on cardiac rehab, check out cardiac rehabilitation resources.
When to Contact Your Healthcare Provider
Knowing when to get medical help is vital. If you feel dizzy, have chest pain, or can’t breathe, call your doctor right away. Regular visits are also important for managing brady and tachy conditions.
Long-term Prognosis and Quality of Life
The future looks different for everyone with heart rate disorders. It depends on the cause and how well you manage it. With the right treatment and lifestyle, many people with bradycardia and tachycardia live full lives. Staying in touch with your doctor is essential for a good quality of life.
Conclusion: Taking Control of Your Heart Health
Knowing about tachycardia and bradycardia is key to a healthy heart. We’ve covered the basics of these heart issues. This includes what they are, their symptoms, causes, and how to manage them.
Handling heart rate problems can make life better. Spotting the signs of tachycardia and bradycardia helps you get help when you need it. It’s important to watch over conditions like sinus bradycardia and tachycardia closely.
We urge you to play a big part in your heart health. Make lifestyle changes, keep an eye on your heart, and get medical help when it’s needed. This way, you can feel better and lower heart disease risks.
By understanding and managing tachycardia and bradycardia, you can control your heart health. It’s all about a mix of medical care and making healthy lifestyle choices.
FAQ
-
- Medical News Today (Tachycardia vs. Bradycardia) : https://www.medicalnewstoday.com/articles/tachycardia-vs-bradycardia
-
- PMC – PubMed Central : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5360359
- Cardiac Specialists (Tachycardia and Bradycardia) : https://cardiacspecialists.com/service-or-procedure/tachycardia-and-bradycardia