Did you know that nearly 1.5 million people in the United States are living with lupus? It’s a chronic autoimmune disease that can affect many parts of the body. Finding out if someone has lupus can be hard, but a Complete Blood Count (CBC) is often the first step.
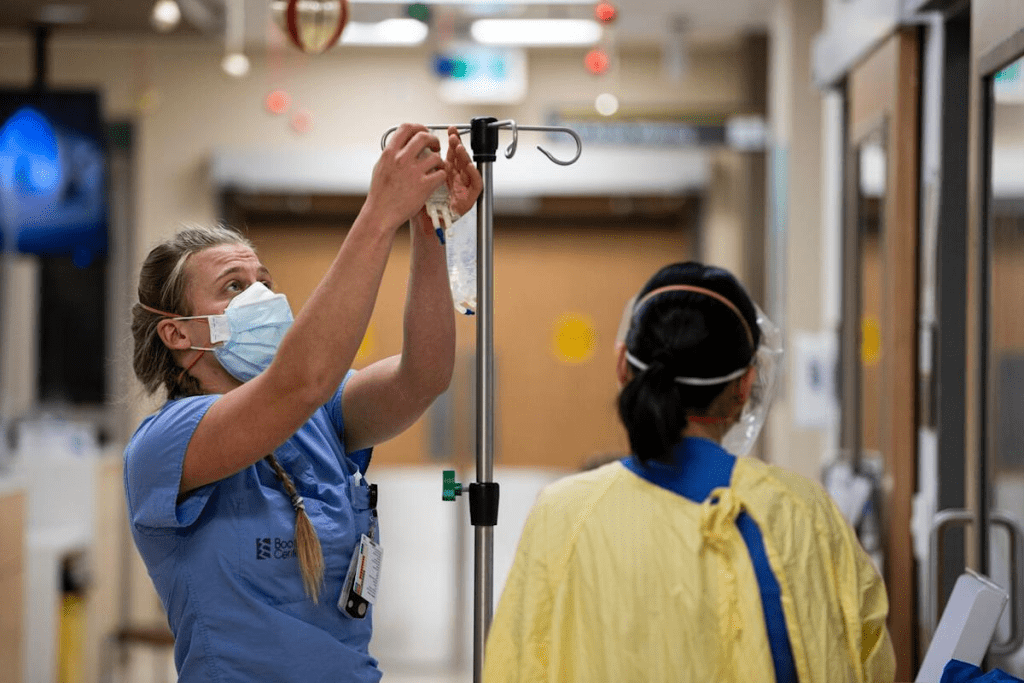
A CBC is a common blood test. It checks the blood for red and white blood cells and platelets. When it comes to lupus diagnosis, a CBC can show signs of the disease.
We use a CBC as a first lupus blood test to spot possible problems. Doctors interpret the results to gain deeper insights into the patient’s overall health.
Key Takeaways
- A CBC is a key blood test for diagnosing and tracking lupus.
- Any odd results in a CBC might mean someone has lupus.
- A CBC looks at different parts of the blood, like red and white blood cells and platelets.
- Diagnosing lupus takes both doctor’s checks and lab tests.
- A CBC is often the first test to find possible issues.
Understanding Systemic Lupus Erythematosus (SLE)
It’s important to know about Systemic Lupus Erythematosus (SLE) if you have it. SLE, or lupus, can harm many parts of your body. This leads to different symptoms.
What is Lupus?
Lupus is a long-lasting disease where your immune system attacks healthy tissues. This causes inflammation and damage in places like your skin, joints, and organs.
“Lupus is a complex and unpredictable disease”, doctors say. This shows why it needs careful care and understanding.
Types of Lupus
There are four main types of lupus. The most common is Systemic Lupus Erythematosus (SLE). It can be mild or very serious.
- SLE: Affects multiple organs and systems.
- Cutaneous Lupus: Primarily affects the skin.
- Drug-Induced Lupus: Triggered by certain medications.
- Neonatal Lupus: A rare condition affecting newborns.
Common Symptoms and Manifestations
Lupus symptoms can differ a lot from person to person. This makes it hard to diagnose. Common signs include:
- Joint pain and swelling
- Skin rashes, like the butterfly-shaped rash on the face
- Fever
- Fatigue
- Hair loss
As a doctor said,
“Lupus is known for its unpredictability and the wide range of its symptoms, making each patient’s experience unique.”
Knowing all about lupus is key to managing it well. By understanding its types and symptoms, you can handle your diagnosis better.
The Role of Blood Tests in Lupus Diagnosis

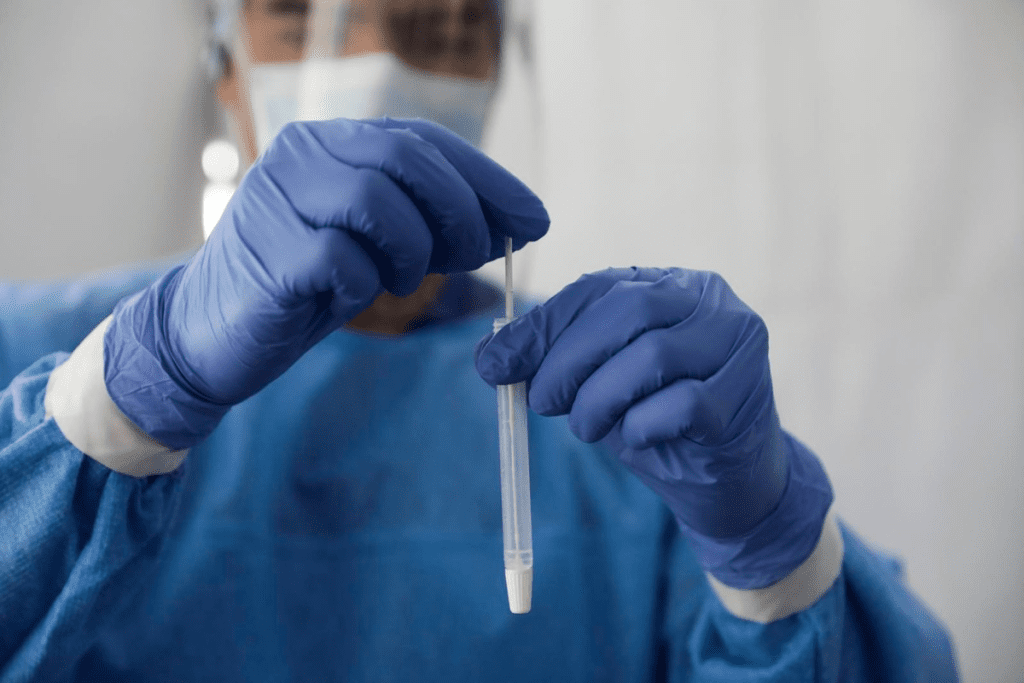
Blood tests are key in diagnosing lupus, a chronic autoimmune disease. They help find specific antibodies and markers linked to lupus. This makes it easier to get an accurate diagnosis.
Why Blood Tests are Essential
Blood tests are vital for diagnosing lupus. They show if certain antibodies and inflammation markers are present. Lupus diagnosis often looks for antinuclear antibodies (ANA) and other autoantibodies.
Some antibodies, like anti-dsDNA and anti-Sm, point strongly to lupus. Tests also check inflammation and organ damage levels. This helps doctors decide on treatment.
Limitations of Laboratory Testing
Even though blood tests are important, they have their limits. Not everyone with lupus will have all the characteristic antibodies. Some people without lupus might have them too. So, diagnostic criteria for lupus use both clinical findings and lab results.
Lab results must be seen in the light of the patient’s symptoms and medical history. A full diagnostic check is needed to exclude other conditions that might look like lupus.
The Diagnostic Criteria for Lupus
The diagnostic criteria for lupus include both clinical and lab findings. The Systemic Lupus International Collaborating Clinics (SLICC) criteria are often used. They combine clinical signs and immunologic markers.
- Clinical signs might include skin rashes, joint pain, kidney disease, and neurological symptoms.
- Immunologic markers include ANA, anti-dsDNA, and anti-Sm antibodies, among others.
Meeting certain criteria helps doctors accurately diagnose lupus. It’s a detailed process that looks at both clinical and lab evidence.
Complete Blood Count (CBC) in Lupus Patients
A CBC test gives important insights into lupus patients’ health. It helps doctors diagnose and track the disease.
Components of a CBC Test
A CBC test checks several blood parts. These include:
- Red Blood Cell (RBC) count and hemoglobin levels
- White Blood Cell (WBC) count and differential
- Platelet count
Each part tells doctors something important. For example, RBC and hemoglobin levels show if a patient has anemia, a common lupus issue.
Common CBC Abnormalities in Lupus
Lupus patients often have abnormal CBC results. These include:
- Anemia: Low RBC count or hemoglobin levels
- Leukopenia: Low WBC count, which can increase the risk of infections
- Thrombocytopenia: Low platelet count, which can lead to bleeding complications
These signs can show how active the disease is or if treatments are causing side effects. Regular CBC tests are key.
How to Interpret CBC Results
Understanding CBC results needs a deep look at the patient’s situation. Doctors consider:
- The patient’s symptoms and medical history
- Current medications and treatments
- Previous CBC results for comparison
Anemia and Lupus: What CBC Results Show
Anemia and lupus are closely linked, with several types of anemia affecting lupus patients. Anemia can greatly impact their health and daily life. A Complete Blood Count (CBC) test is key in diagnosing anemia in these patients.
Types of Anemia in Lupus Patients
Lupus patients face different anemia types, such as anemia of chronic disease, iron deficiency anemia, and hemolytic anemia. Anemia of chronic disease is common in those with ongoing inflammation. Iron deficiency anemia can stem from low iron intake or chronic blood loss. Hemolytic anemia happens when red blood cells are destroyed too quickly.
Hemolytic Anemia Markers
Hemolytic anemia is a major concern for lupus patients. Signs include elevated reticulocyte count, increased lactate dehydrogenase (LDH), and decreased haptoglobin levels. These markers show red blood cells are being destroyed, leading to anemia. A CBC test can hint at hemolytic anemia, leading to further tests.
Other Red Blood Cell Abnormalities
CBC tests also reveal other red blood cell issues. These include red blood cell distribution width (RDW) and mean corpuscular volume (MCV) abnormalities. These help classify anemia types. Knowing these details is vital for managing lupus.
White Blood Cell Changes in Lupus
White blood cell changes are key in lupus, showing how active the disease is and how well treatments work. Lupus, a chronic autoimmune disease, can affect white blood cell counts. This can lead to various complications.
Leukopenia in Lupus Patients
Leukopenia, or low white blood cell count, is common in lupus patients. It raises the risk of infections and may need changes in treatment plans. We will look at the causes and effects of leukopenia in lupus.
Causes of Leukopenia: Leukopenia in lupus comes from the disease itself and immunosuppressive drugs.
- Autoimmune destruction of white blood cells
- Immunosuppressive therapy
- Bone marrow suppression
Lymphocyte Abnormalities
Lymphocytes, a type of white blood cell, are vital for the immune system. In lupus, lymphocyte counts and function can change. This affects the disease’s pathology.
| Lymphocyte Abnormality | Implication in Lupus |
| Lymphopenia | Reduced lymphocyte count, potentially increasing infection risk |
| Lymphocyte Activation | Hyperactive lymphocytes contribute to autoimmune responses |
Neutrophil Count Changes
Neutrophils, another important white blood cell, can also be affected in lupus. Changes in neutrophil counts show disease activity or infections.
Neutropenia in Lupus: A low neutrophil count raises the risk of bacterial infections. It’s vital to monitor neutrophil counts in lupus patients.
Understanding white blood cell count changes helps healthcare providers manage lupus better. They can tailor treatments to meet each patient’s needs.
Platelet Abnormalities in Lupus Blood Work
Thrombocytopenia, or low platelet count, is common in systemic lupus erythematosus (SLE) patients. It affects how we manage lupus. Knowing about these abnormalities is key.
Thrombocytopenia in Lupus
Thrombocytopenia means having fewer than 150,000 platelets per microliter. In lupus, it can happen due to immune attacks or bone marrow issues. Immune thrombocytopenia is a big problem, where the body attacks platelets.
Thrombocytopenia can cause anything from small bruises to serious bleeding. We must keep an eye on platelet counts to adjust treatments.
Platelet Function Tests
Platelet function tests help us understand how well platelets work in lupus patients. These tests check if platelets can form clots properly. Platelet aggregometry is a test that shows how platelets react to different substances.
Problems with platelet function can lead to bleeding or clotting issues. It’s important to know this to plan the right treatment.
Implications for Treatment
Thrombocytopenia and platelet issues in lupus affect treatment choices. We must balance the risk of bleeding against the chance of blood clots. Treatment strategies might include drugs to fight autoantibodies or boost platelet production.
In some cases, rituximab, a drug that targets B cells, is used for severe thrombocytopenia. The right treatment depends on the cause of low platelets and the patient’s situation.
Antinuclear Antibody (ANA) Test for Lupus
The Antinuclear Antibody (ANA) test is key in finding lupus. It’s a chronic disease that can harm many organs.
Understanding ANA Testing
The ANA test looks for antinuclear antibodies in the blood. These antibodies attack the cell nucleus and can cause inflammation and damage. The test uses a special dye to see if these antibodies are present.
Interpreting ANA Patterns and Titers
When looking at ANA test results, two things matter: the pattern and the titer level. The pattern can be homogeneous, speckled, nucleolar, or peripheral. Each pattern is linked to different diseases. The titer level shows how much of the antibody is present. Higher levels often mean a person might have lupus.
Here are the common ANA patterns and what they mean:
- Homogeneous pattern: Often linked to lupus and shows antibodies against DNA or histones.
- Speckled pattern: Seen in many autoimmune diseases, including lupus, Sjögren’s syndrome, and scleroderma.
- Nucleolar pattern: Usually linked to scleroderma.
- Peripheral pattern: Less common, often seen in lupus.
False Positives and Limitations
Even though the ANA test is good for finding lupus, it’s not perfect. It can show false positives in healthy people, at low titers, and in those with other autoimmune diseases. So, test results must be looked at with other symptoms and tests in mind.
Anti-dsDNA Antibodies in Lupus Diagnosis
Diagnosing lupus is complex, and anti-dsDNA antibodies play a key role. These antibodies are a specific type of anti-nuclear antibody (ANA). They are closely linked to systemic lupus erythematosus (SLE).
Significance of Anti-dsDNA Antibodies
Anti-dsDNA antibodies are important because they are very specific to SLE. The presence of these antibodies is a key diagnostic criterion for lupus. It helps doctors tell lupus apart from other autoimmune diseases.
Here are some key points about anti-dsDNA antibodies:
- They are found in about 70% of SLE patients.
- High levels are linked to more active disease.
- They play a role in lupus nephritis, a common SLE complication.
What is Considered a High Level
Doctors measure anti-dsDNA antibodies through blood tests, like ELISA or CLIFT. The normal range can differ between labs. But generally, a high level is above 30 IU/mL, though this can change.
Correlation with Disease Activity
There’s a strong link between anti-dsDNA antibody levels and lupus activity. High levels often mean active disease, like kidney problems. Watching these levels helps doctors see how well treatment is working.
Here are some important points about this link:
- High anti-dsDNA levels often mean a flare is coming.
- Lower levels mean treatment is working and disease is less active.
- Regular checks are key to managing lupus well.
Complement Proteins C3 and C4 in Lupus
The immune system’s complement proteins, like C3 and C4, show how active lupus is. They help the body fight off infections. These proteins are important for keeping the immune system working right.
The Role of Complement in Immune Function
Complement proteins are vital for the immune system. They help fight off infections by killing pathogens or marking them for destruction. C3 and C4 are key players in this process, helping to clear out harmful substances and control inflammation.
Low Complement Levels in Active Lupus
In people with lupus, low C3 and C4 levels often mean the disease is active. This happens because lupus forms immune complexes that use up these proteins. Low complement levels can signal that the disease is getting worse and might flare up.
Monitoring Disease Activity with Complement Tests
Checking C3 and C4 levels is important for managing lupus. Doctors use these tests to see how active the disease is and adjust treatments. Regular tests help catch flare-ups early, so they can be treated quickly.
Complement tests, along with other tools, give a full picture of lupus. This helps doctors create treatment plans that work best for each patient. This approach is key to managing lupus well and improving patient care.
The Most Common Test for Lupus: Comprehensive Panels
Testing for lupus is key to diagnosing and managing the disease. Lupus is a complex autoimmune disorder. It needs a detailed approach to diagnosis. A lupus panel is a set of tests that check different parts of the disease.
Components of a Complete Lupus Panel
A complete lupus panel includes several important tests. These are:
- Complete Blood Count (CBC): Checks for anemia, leukopenia, or thrombocytopenia.
- Antinuclear Antibody (ANA) Test: Looks for ANA, often positive in lupus patients.
- Anti-dsDNA Antibodies: Measures the level of these specific antibodies linked to lupus.
- Complement Levels (C3 and C4): Shows the activity of the disease.
- Erythrocyte Sedimentation Rate (ESR) or C-Reactive Protein (CRP): Checks for inflammation.
When Additional Testing is Needed
Even with a lupus panel, more tests might be needed. This is true if the diagnosis is unclear or if symptoms are unusual. Tests like anti-Smith antibodies or anti-RNP antibodies might be ordered.
Interpreting Multiple Test Results
Understanding lupus test results is complex. For example, a positive ANA test and high anti-dsDNA antibodies suggest lupus. But, diagnosis comes from a mix of clinical findings and lab results.
We use these panels to diagnose lupus and track its activity. This helps us adjust treatment plans. Knowing about lupus panels and how to read the results helps healthcare providers give better care.
Other Specific Antibody Tests for Lupus
Several specific antibody tests are key in diagnosing and managing lupus. These tests help understand the disease’s complexity. They also help tailor treatment plans to each patient’s needs.
Anti-Smith Antibodies
Anti-Smith (anti-Sm) antibodies are very specific for Systemic Lupus Erythematosus (SLE). They are one of the criteria for diagnosing lupus. Though found in only about 30% of patients, their presence is a strong indicator of the disease.
Key points about anti-Sm antibodies:
- High specificity for SLE
- Found in approximately 30% of lupus patients
- Considered a diagnostic criterion
Anti-RNP Antibodies
Anti-RNP (anti-ribonucleoprotein) antibodies are linked to mixed connective tissue disease. They can also be present in lupus patients. High levels may indicate a condition that overlaps with other autoimmune diseases.
Significance of anti-RNP antibodies:
- Associated with mixed connective tissue disease
- Can be present in lupus patients
- May indicate overlapping autoimmune conditions
Anti-Ro/SSA and Anti-La/SSB Antibodies
Anti-Ro/SSA and anti-La/SSB antibodies are often found together. They are associated with Sjögren’s syndrome, subacute cutaneous lupus, and neonatal lupus. These antibodies are significant in assessing the risk of congenital heart block in newborns of mothers with lupus.
Key aspects of anti-Ro/SSA and anti-La/SSB:
- Frequently occur together
- Linked to Sjögren’s syndrome and subacute cutaneous lupus
- Important in assessing risk for neonatal lupus
Antihistone Antibodies
Antihistone antibodies are commonly found in drug-induced lupus. This condition mimics SLE but is triggered by certain medications. These antibodies can help differentiate between drug-induced lupus and idiopathic SLE.
Relevance of antihistone antibodies:
- Common in drug-induced lupus
- Help differentiate between drug-induced and idiopathic SLE
Understanding these specific antibody tests is key for diagnosing and managing lupus effectively. Each test provides unique insights into the disease’s characteristics. They help in developing a personalized treatment plan.
Inflammatory Markers in Lupus Blood Work
Inflammatory markers are key in checking lupus activity. They help doctors see how much inflammation is in the body. This is vital for diagnosing and managing lupus.
Erythrocyte Sedimentation Rate (ESR)
The ESR test measures how fast red blood cells settle in a test tube. It shows how much inflammation is in the body. A higher ESR means more inflammation.
Key aspects of ESR in lupus:
- ESR levels can be high when lupus is active
- It’s not specific, meaning it can rise in many inflammatory conditions
- Doctors use ESR with other tests to check lupus activity
C-Reactive Protein (CRP)
CRP is a liver-made protein released into the blood when there’s inflammation. It’s a key marker for inflammation in lupus patients.
Significance of CRP in lupus:
- CRP levels show if there’s inflammation
- High CRP levels might mean active lupus or an infection
- CRP helps tell if symptoms are from a lupus flare or something else
Other Inflammatory Indicators
Other than ESR and CRP, there are more markers for lupus activity. These include various cytokines and proteins involved in inflammation.
Knowing these markers helps doctors keep a closer eye on lupus activity. They can then adjust treatment plans as needed.
Monitoring Lupus Through Regular Blood Testing
Blood tests are key in managing lupus. They help track the disease and guide treatment. Regular tests let doctors see how the disease is doing and make needed changes.
Frequency of Testing
How often lupus patients need blood tests varies. It depends on how active the disease is and the treatment plan. Patients with active lupus might need tests every few weeks. Those with stable lupus might only need tests every few months.
It’s best for patients to talk with their doctors about how often they should get tested.
Tracking Disease Activity
Blood tests are important for tracking lupus. They check for:
- Complete Blood Count (CBC) to look for anemia, low white blood cells, or low platelets
- Inflammatory markers like ESR or CRP to see inflammation levels
- Complement levels (C3 and C4) to check the immune system
- Anti-dsDNA antibody levels, which can show disease activity in some
These tests give doctors a full picture of the disease. They can then make the best decisions.
Adjusting Treatment Based on Results
Treatment changes are often needed based on blood test results. For example, if tests show a flare is coming, doctors might adjust medications. If the disease is well-controlled, treatment might be changed to reduce side effects.
Here’s how blood test results can lead to treatment changes:
| Blood Test Result | Possible Interpretation | Treatment Adjustment |
| Low C3 and C4 levels | Active lupus, possible flare | Increase immunosuppressive medication |
| High anti-dsDNA levels | Increased disease activity | Adjust or intensify treatment |
| Normal CBC and inflammatory markers | Disease is well-controlled | Maintain current treatment, monitor closely |
Regular blood testing is key in managing lupus. It helps in precise and responsive care. By understanding the importance of these tests, lupus patients can better control their disease and improve their quality of life.
Conclusion: Understanding Your Lupus Test Results
It’s key to understand lupus test results for good care. We’ve looked at blood tests like the Complete Blood Count (CBC) and the Antinuclear Antibody (ANA) test. These help doctors spot and track lupus.
These tests give clues about lupus, helping doctors plan treatments. They check for signs like anemia and low blood cells, common in lupus patients.
Handling lupus needs a full plan, including tests and patient input. Blood tests are key to keeping an eye on the disease and tweaking treatments. Knowing your test results helps you work with your doctor for the best results.
Good lupus care means knowing how symptoms, tests, and treatments work together. By staying informed, patients can manage their lupus better and live a fuller life.
FAQ
What is a CBC, and how is it used in diagnosing lupus?
A CBC is a blood test that checks the blood’s components. It looks at red and white blood cells and platelets. It’s a first step to see if lupus might be present by finding any unusual signs.
What are the common symptoms and manifestations of lupus?
Lupus is a chronic disease that can affect many parts of the body. Symptoms include fatigue, joint pain, skin rashes, and kidney issues.
Why are blood tests essential in diagnosing lupus?
Blood tests are key in diagnosing lupus. They help find specific antibodies and markers that show the disease. These tests are used with symptoms and other criteria to confirm lupus.
What does a CBC test measure, and what abnormalities are common in lupus patients?
A CBC test looks at the blood’s components, like red and white blood cells and platelets. In lupus patients, common issues are anemia, low white blood cell count, low lymphocyte count, and low platelet count.
What is the significance of anti-dsDNA antibodies in lupus diagnosis?
Anti-dsDNA antibodies are specific to lupus. Their presence helps diagnose and track the disease. High levels often mean the disease is active.
How are complement proteins C3 and C4 used in lupus diagnosis and monitoring?
Complement proteins C3 and C4 are important in the immune system. Low levels are linked to active lupus. These tests help monitor the disease and check if treatment is working.
What is the Antinuclear Antibody (ANA) test, and how is it used in lupus diagnosis?
The ANA test is a key tool in diagnosing lupus. It detects antibodies against cell nuclei. A positive test suggests lupus, and further tests confirm the diagnosis.
How often should lupus patients undergo blood testing?
The blood test frequency for lupus patients varies. It depends on the disease’s severity, treatment success, and any complications. Regular tests are important to track the disease and adjust treatment.
What other specific antibody tests are used in lupus diagnosis and monitoring?
Other tests used in lupus diagnosis and monitoring include anti-Smith, anti-RNP, anti-Ro/SSA, anti-La/SSB, and antihistone antibodies. Each test provides important information about the disease.
How are inflammatory markers used in lupus management?
Inflammatory markers like ESR and CRP help assess lupus activity. They show inflammation levels and guide treatment. High levels often mean the disease is active.
References
Lupus Blood Test Results: What to Know. (2022). HSS.edu.
https://www.hss.edu/health-library/conditions-and-treatments/lupus-blood-test-results-explained


































