Last Updated on October 21, 2025 by mcelik
Going through a stem cell transplant can change a patient’s life. It’s a complex process, but with the right care, patients can feel confident. This journey is made easier with top-notch medical care.
A stem cell transplant has five key stages. These are tests, harvesting, conditioning, transplanting, and recovery. Each step is vital for a successful transplant.
Patients get many treatments and checks during these stages. This includes bone marrow transplant and hematopoietic stem cell transplantation. These help prepare the body for the transplant.
Key Takeaways
- Stem cell transplant is a complex, multi-stage procedure.
- The five main stages are: tests and examinations, harvesting, conditioning, transplanting the stem cells, and recovery.
- Comprehensive care is key to transplant success.
- Patients get many treatments and checks during the stages.
- Top medical care improves patient results.
Understanding Stem Cell Transplants
Stem cell transplants replace damaged cells with healthy ones. This can cure many diseases. They are a key treatment for serious illnesses.
Definition and Purpose of Stem Cell Transplants
A stem cell transplant, or bone marrow transplant, replaces damaged cells with healthy ones. The main goal is to help the body make healthy blood cells again. These transplants help treat cancer, blood disorders, and immune system diseases.
Stem cell transplants offer many benefits. They can cure some diseases and improve life quality for those with chronic conditions. They give hope to patients who thought they had no treatment options.
Types of Stem Cell Transplants: Autologous vs. Allogeneic
There are two main types of stem cell transplants: autologous and allogeneic. Autologous transplants use the patient’s own stem cells, collected, stored, and then reinfused. This reduces the risk of GVHD.
Allogeneic transplants use stem cells from a donor, who can be a family member or someone else. Allogeneic transplants have a higher GVHD risk but are good for genetic disorders or blood cancers.
- Autologous transplants are often used for patients with multiple myeloma or certain types of lymphoma.
- Allogeneic transplants are typically used for patients with leukemia or other blood disorders.
- The choice between autologous and allogeneic transplants depends on the patient’s specific medical condition and overall health.
It’s important to understand the differences between autologous and allogeneic stem cell transplants. Knowing the benefits and risks helps patients make informed decisions about their treatment.
The Evolution of Stem Cell Therapy
Medical research is always moving forward, and stem cell therapy is a big part of it. We’re seeing a big change in how stem cells are used to treat different health issues.
What Are Stem Cells?
Stem cells are young cells that can grow into many types of cells in our bodies. They help fix and repair tissues naturally. Stem cells are special because they can fix or replace damaged tissues.
Sources of Therapeutic Stem Cells
Therapeutic stem cells come from different places in our bodies. The main sources are:
- Bone marrow: full of stem cells that can turn into many cell types.
- Peripheral blood: stem cells can move into the blood and be collected.
- Umbilical cord blood: a great source of stem cells for treatment, showing that stem cells can come from the afterbirth.
These sources are key for stem cell therapy, opening up new treatments for many health problems. Knowing where stem cells come from is important for improving their use in medicine.
The flexibility of stem cells and their many sources show the promise of stem cell therapy in today’s medicine. As research goes on, we’ll see more and more uses of therapeutic stem cells.
Who Needs a Stem Cell Transplant?
Stem cell transplants are a cure for some medical conditions. We’ll look at the conditions treated and who can get this procedure.
Medical Conditions Treated with Stem Cell Transplants
Stem cell transplants mainly help with blood cancers and disorders. They treat leukemia, lymphoma, and multiple myeloma. They also help with aplastic anemia and sickle cell disease.
Stem cell transplants are a key treatment for many serious health problems. They replace damaged stem cells with healthy ones. This can cure the disease.
Determining Patient Eligibility
To see if a patient can get a stem cell transplant, we look at several things. We check the patient’s overall health, the specific condition, and the stage of the disease. We also consider the patient’s age and previous treatments.
- The type and stage of the disease
- The patient’s overall health and fitness for the procedure
- Previous treatments and their outcomes
- The availability of a suitable donor (for allogeneic transplants)
We carefully check these factors to see if a stem cell transplant is right for a patient.
Stage 1: Pre-Transplant Testing and Evaluation
Before a stem cell transplant, patients must go through a detailed testing and evaluation phase. This stage is key to checking the patient’s health and if they’re ready for the transplant.
Comprehensive Medical Assessment
A thorough medical check-up is done to see the patient’s current health. We carefully look at their medical history, including past treatments and any health issues that might impact the transplant. This helps us spot risks and plan how to avoid them.
Laboratory Tests and Imaging
Laboratory tests and imaging studies are vital in the pre-transplant evaluation. We run a variety of tests, like blood work, to check blood cell counts, organ function, and overall health. We might also use X-rays, CT scans, or MRI scans to look at internal organs and find any problems.
Psychological Evaluation and Preparation
A psychological evaluation is also a key part of the pre-transplant process. We check the patient’s mental health and offer support to make sure they’re emotionally ready for the transplant and recovery. This helps us find any mental health concerns and plan how to deal with them.
By carefully checking the patient’s physical and mental health, we make sure they’re ready for the stem cell transplant. This detailed approach helps reduce risks and improve outcomes.
Stage 2: Stem Cell Collection and Harvesting
Stem cell collection and harvesting are key steps in the stem cell transplant journey. They need careful planning and execution. This stage is vital because it affects the quality and amount of stem cells for the transplant.
Donor Selection Process
The journey starts with donor selection. We look for a donor who matches the patient in terms of genetics, health, and stem cell donation ability. For allogeneic transplants, donors can be family or unrelated. We use advanced genetic testing to find the best match.
Growth Factor Administration
To boost stem cell production, growth factors are given to the donor. This step is key to getting more stem cells in the blood. Growth factors are given through injections, and we watch closely to keep the donor safe and the treatment effective.
Collection Methods
There are two main ways to collect stem cells: apheresis and bone marrow harvesting. Apheresis takes stem cells from the blood, while bone marrow harvesting takes them directly from the bone. The choice depends on the transplant type, donor health, and patient needs.
Stem cell collection can be complex and may worry donors and patients. Our team offers full support and care during this stage. We aim to make the process as smooth and safe as we can.
Stage 3: Conditioning Regimen
Conditioning regimens are key to the success of stem cell transplants. They get rid of diseased cells and prepare the body for the transplant.
Purpose of Conditioning
The main goal of conditioning is to suppress the immune system. This prevents the body from rejecting the new stem cells. It also helps get rid of any diseased cells in the body. This step is vital for the new stem cells to work well.
High-Intensity vs. Reduced-Intensity Conditioning
Conditioning regimens can be more or less intense. This depends on the patient’s health, age, and the transplant type. High-intensity conditioning uses strong doses of chemotherapy and/or radiation. It’s often for patients with certain cancers.
Reduced-intensity conditioning uses lower doses. It’s less harsh and better for older patients or those with health issues. This makes it safer for them.
Common Conditioning Protocols
Protocols include chemotherapy like cyclophosphamide and fludarabine, and total body irradiation (TBI). The choice depends on the disease, transplant type, and patient health.
- Chemotherapy-based regimens are common for blood cancers.
- Total body irradiation kills cancer cells and weakens the immune system.
- Each protocol is customized for the patient’s specific needs.
Stage 4: The Transplantation Procedure
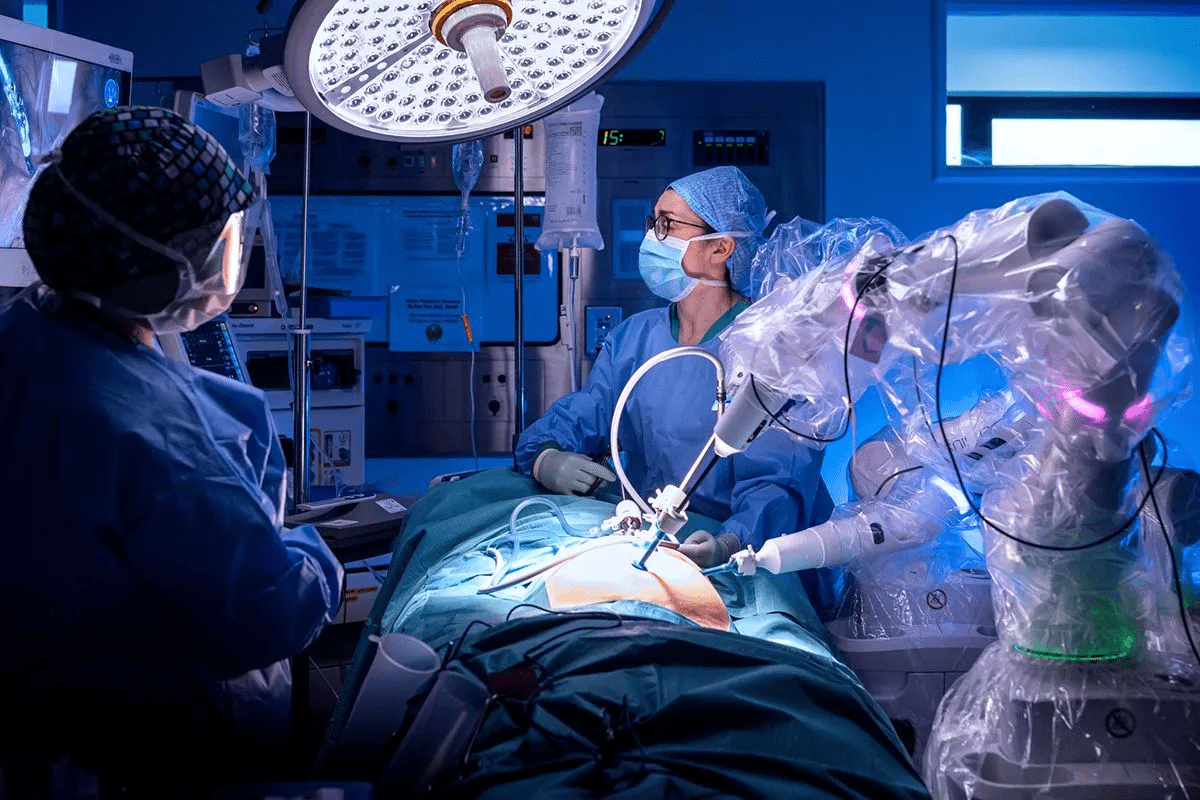
Infusing stem cells into the patient’s body is the fourth stage of the transplant process. This stage is key because it introduces stem cells to rebuild the bone marrow and restore the immune system.
Stem Cell Infusion Process
The stem cell infusion process is simple and is like a blood transfusion. The collected stem cells are given to the patient through a central venous catheter. We watch the patient closely to catch any bad reactions.
The infusion takes about 30 minutes to an hour. Our medical team is there to handle any issues that come up.
What Happens During the Procedure
During the infusion, we keep a close eye on the patient’s vital signs and watch for bad reactions. The infusion is done slowly to lower the risk of problems.
- The patient’s heart rate, blood pressure, and oxygen levels are checked all the time.
- We are ready to deal with any quick reactions, like allergies or infusion issues.
- The stem cells are given slowly to avoid overwhelming the patient’s system.
Immediate Post-Infusion Care
After the infusion, we keep a close eye on the patient for a while to make sure there are no problems. We watch for any reactions and check their vital signs often.
Our care after the infusion includes:
- Watching for any bad reactions or issues.
- Handling side effects, like nausea or tiredness.
- Providing support to keep the patient comfortable and safe.
By managing the infusion carefully and giving good care afterward, we can reduce risks and help the transplant succeed.
Stage 5: Post-Transplant Recovery and Monitoring
Post-transplant recovery is a key stage that needs constant medical watch. After the stem cell transplant, patients are closely watched. This is to see how the new stem cells settle in the bone marrow.
Engraftment Process and Success Rates
The engraftment process usually takes 2-4 weeks after the transplant. During this time, patients face risks of infections and other issues. We keep a close eye on their blood counts and health to ensure the new cells take hold.
Hospital Recovery Phase
In the hospital recovery phase, we watch for immediate problems like infections, bleeding, or GVHD. We offer support care, like transfusions and antibiotics, to handle these issues.
Long-term Follow-up Care
After leaving the hospital, patients need ongoing care to check their health and manage long-term issues. This includes regular visits with the transplant team and watching for GVHD signs.
Long-term care is vital for the best outcomes after a stem cell transplant. We work with patients and their families to offer full care and support during recovery.
Potential Complications and Management
The journey doesn’t end with a stem cell transplant. Patients must face complications that can affect their recovery and long-term health.
Graft-Versus-Host Disease
Graft-versus-host disease (GVHD) is a big risk after an allogeneic stem cell transplant. Here, the donated stem cells attack the recipient’s body. GVHD can be acute or chronic, with symptoms ranging from mild to severe. Management strategies include using immunosuppressive medications to reduce the immune response and prevent damage to vital organs.
Infections and Immune System Recovery
Patients undergoing stem cell transplants face a higher risk of infections. This is because their immune system is suppressed during the conditioning regimen and while the new immune system matures. We stress the need for infection prevention measures, like prophylactic antibiotics and antifungal medications, to lower this risk.
- Regular monitoring for signs of infection
- Use of antimicrobial prophylaxis
- Isolation techniques to minimize exposure to pathogens
Organ Damage and Other Side Effects
Organ damage is another risk after a stem cell transplant. The conditioning regimen can harm various organs, like the liver, lungs, and heart. We watch patients closely for early signs of organ dysfunction and work to prevent long-term damage.
Research shows many patients face complications after a stem cell transplant. GVHD happens in about 30-50% of patients getting allogeneic transplants. Knowing these stats helps us tailor our care to meet each patient’s needs.
- GVHD incidence rates vary based on donor type and conditioning regimen
- Infection rates are highest in the first few months post-transplant
- Long-term follow-up care is key for managing late effects
By understanding the possible complications and using effective management strategies, we can better outcomes for patients getting stem cell transplants.
Success Rates and Outcomes of Stem Cell Transplants
Stem cell transplants have varied success rates. Many factors play a role in these outcomes. We’ll look at these factors and their effects, helping patients understand what to expect.
Factors Affecting Transplant Success
Several key factors influence the success of stem cell transplants. These include the disease being treated, the patient’s health, and the transplant type. Autologous transplants use the patient’s own stem cells, while allogeneic transplants use donor cells.
The patient’s age and health are also important. Younger, healthier patients usually do better. The match between donor and recipient in allogeneic transplants also matters a lot.
Disease-Specific Survival Rates
Survival rates after stem cell transplants vary by disease. For example, some leukemia or lymphoma patients may have better survival rates than others.
Research shows that patients with multiple myeloma or lymphoma can see significant improvement with transplants. But, the disease’s stage at transplant time can affect success.
Quality of Life After Transplantation
Proper care can greatly improve life after stem cell transplants. Many patients regain their health, allowing them to live normally again. Some can even go back to work.
But some patients face long-term side effects, like graft-versus-host disease (GVHD) in allogeneic transplants. This can lower their quality of life. It’s vital to have ongoing care to manage these issues and improve outcomes.
Understanding what affects transplant success and survival rates helps us manage patients hopes better. The quality of life after transplant is key to the procedure’s success.
Conclusion
Exploring the five stages of stem cell transplants shows us how complex this process is. It needs thorough care for the best results. Each stage, from testing before the transplant to recovery after, requires careful attention and a team effort.
Stem cell therapy has changed how we treat many diseases. Its success depends on the quality of care given during the transplant. Patients and doctors can better face the challenges and benefits of stem cell transplants by understanding this process.
Good care is key to better patient outcomes and a better life. As we move forward in stem cell therapy, focusing on the patient is vital. We must offer support and care that meets each person’s specific needs during a stem cell transplant.
FAQ’s:
What is a stem cell transplant?
A stem cell transplant replaces damaged or diseased stem cells with healthy ones. This can be done using the patient’s own stem cells or those from a donor.
What are stem cells, and what is their role in the body?
Stem cells can develop into different types of cells in the body. They are key in the development, growth, and repair of tissues and organs.
What medical conditions are treated with stem cell transplants?
Stem cell transplants treat blood cancers like leukemia and lymphoma. They also treat certain blood disorders and immune system disorders.
What is the difference between autologous and allogeneic stem cell transplants?
Autologous transplants use the patient’s own stem cells. Allogeneic transplants use stem cells from a donor. Autologous transplants are often for cancer patients. Allogeneic transplants are for blood disorders or certain leukemias.
What is involved in the pre-transplant testing and evaluation stage?
The pre-transplant stage includes a medical assessment and lab tests. It also involves psychological evaluations to check if the patient is a good candidate for the transplant.
How are stem cells collected and harvested?
Stem cells are collected from bone marrow, peripheral blood, or umbilical cord blood. First, growth factors are given to stimulate stem cell production. Then, a procedure is done to collect the cells.
What is the purpose of the conditioning regimen before a stem cell transplant?
The conditioning regimen prepares the body for the transplant. It destroys diseased cells and suppresses the immune system. This reduces complications and improves transplant success.
What are the possible complications of a stem cell transplant?
Complications include graft-versus-host disease, infections, and organ damage. These can be managed with proper medical care and monitoring.
What is graft-versus-host disease?
Graft-versus-host disease is a complication of allogeneic transplants. It occurs when the donor’s immune cells attack the patient’s tissues and organs.
What is the success rate of stem cell transplants?
The success rate varies based on the condition, transplant type, and other factors. Stem cell transplants are effective for many patients with certain conditions.
What is the quality of life like after a stem cell transplant?
Life after a transplant varies by patient and condition. Many patients return to normal activities and enjoy better health and well-being after a successful transplant.
Where do stem cells come from?
Stem cells come from bone marrow, peripheral blood, and umbilical cord blood. The source depends on the transplant type and the patient’s condition.
What is hematopoietic stem cell transplantation?
Hematopoietic stem cell transplantation uses stem cells to replace blood-forming cells. It’s often used for blood cancers and disorders.
References
- Warner, M. J., & Armitage, A. E. (2023). Iron Deficiency Anemia. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448065/
- American Cancer Society. (2022). Getting a Stem Cell or Bone Marrow Transplant. https://www.cancer.org/cancer/managing-cancer/treatment-types/stem-cell-transplant/process.html