Last Updated on December 4, 2025 by Ugurkan Demir
Third-degree AV heart block, also known as complete heart block, is a serious heart condition. It stops electrical signals from the atria from reaching the ventricles.
At Liv Hospital, we know how dangerous this condition is. We also understand the importance of its unique ECG signs. Our team helps patients find the best ways to diagnose and treat it.
Understanding third-degree AV heart block is key for diagnosis and treatment. This condition makes the atria and ventricles beat on their own. Symptoms include severe slow heart rate, tiredness, and fainting.
Key Takeaways
- Third-degree AV heart block is a life-threatening cardiac condition.
- It is characterized by the complete blockage of electrical impulses from the atria to the ventricles.
- Distinctive ECG features are critical for diagnosis.
- Understanding key aspects is vital for effective treatment.
- Liv Hospital provides expert care and guidance for patients with this condition.
What Is Third Degree AV Heart Block?
Third degree AV heart block, also known as complete heart block, is a serious heart condition. It happens when electrical signals from the atria can’t reach the ventricles. This makes the atria and ventricles beat on their own, leading to severe bradycardia, fatigue, syncope, and even sudden cardiac death.
Definition and Terminology
Heart block is when the heart’s electrical signals don’t follow the usual path. Third degree AV heart block is the most severe form. It means there’s a complete block of electrical signals from the atria to the ventricles.
This condition is marked by complete AV dissociation. This means the atria and ventricles beat independently without any coordination. Understanding these terms is key to understanding the condition.
Prevalence and Epidemiology
Third degree AV heart block becomes more common with age. It’s often linked to heart disease, certain medications, or other heart-related conditions. Studies show it’s more common in older people, mainly those with heart problems.
| Age Group | Prevalence of Third Degree AV Block |
| Less than 40 | Rare |
| 40-60 | Moderate |
| Greater than 60 | High |
The table shows the risk increases with age. This highlights the need to watch and manage heart conditions in older adults. Symptoms include severe bradycardia, fatigue, syncope, and risk of sudden cardiac death. This makes early diagnosis and treatment critical.
“The diagnosis of third degree AV block is mainly based on electrocardiographic (ECG) findings. These show complete dissociation between atrial and ventricular activity.”
— ECG Interpretation Guide
Knowing about third degree AV heart block is key to spotting at-risk groups. It helps us take the right steps in diagnosis and treatment. We must consider these factors when checking patients with suspected heart conduction problems.
Pathophysiology of Complete Heart Block
To understand complete heart block, we must first look at how the heart normally works. The heart’s electrical system starts in the SA node. It then goes through the AV node to the ventricles. This ensures the heart beats in sync, pumping blood well.
Normal Cardiac Conduction System
The heart’s electrical system is complex. It starts in the SA node in the right atrium. Then, it moves to the AV node. From there, it goes down the Bundle of His, to the bundle branches, and to the Purkinje fibers. This system makes sure the heart pumps blood efficiently.
Mechanism of AV Node Disruption
In complete heart block, the AV node is disrupted. This can happen for many reasons, like heart disease or certain medicines. Because of this, the heart’s electrical signals can’t reach the ventricles. This leads to the atria and ventricles beating out of sync.
Consequences of Complete AV Dissociation
When the atria and ventricles don’t beat together, the ventricles start their own rhythm. This might be enough to keep some blood flowing. But, it’s often not enough. Patients might feel tired, have a slow heart rate, and not enough blood flow.
Because of this, doctors often need to act fast. They might use a pacemaker to help the heart beat right again. This can help the patient feel better and avoid more serious problems.
Essential Fact #1: Third Degree AV Heart Block Creates Complete AV Dissociation
Third-degree AV heart block causes the atria and ventricles to beat on their own. This happens because of a block in the electrical pathway. As a result, there’s no coordination between the atrial and ventricular rhythms.
Electrical Independence of Atria and Ventricles
In third-degree AV heart block, the atria and ventricles beat at different rates. The atria are controlled by the sinoatrial node, while the ventricles are controlled by an escape pacemaker. This means the atria and ventricles don’t beat in sync.
The P waves on an electrocardiogram (ECG) show when the atria depolarize. The QRS complexes show when the ventricles depolarize. In third-degree AV block, P waves and QRS complexes are not linked, showing they beat independently.
Escape Pacemaker Activation
The ventricles use an escape pacemaker to keep a rhythm when the normal pathway is blocked. This pacemaker can be in the AV junction or in the ventricles. The rate at which it fires determines the ventricular rate.
A junctional escape pacemaker usually fires at 40-60 beats per minute. A ventricular escape pacemaker fires slower, at 20-40 beats per minute. The activation of an escape pacemaker is key to keeping the heart pumping when normal conduction is lost.
Hemodynamic Consequences
Third-degree AV heart block has big effects on the heart’s function. The lack of coordination between atrial and ventricular contractions can lower cardiac output. This can cause symptoms like dizziness, fatigue, and shortness of breath.
To show the impact on the heart, let’s look at a table:
| Hemodynamic Parameter | Normal Condition | Third-Degree AV Block |
| Cardiac Output | Optimal due to coordinated AV contractions | Reduced due to loss of AV synchrony |
| Ventricular Rate | Normal (60-100 bpm) | Abnormally slow (dependent on escape pacemaker) |
| Atrial Contribution to Ventricular Filling | Significant | Lost due to AV dissociation |
Understanding these effects is key to managing third-degree AV heart block. It helps decide if a pacemaker is needed.
Essential Fact #2: Clinical Presentations and Warning Signs
Third-degree AV heart block shows itself in many ways. But, there are some common warning signs. These signs happen because the heart can’t meet the body’s needs well.
Bradycardia and Its Symptoms
Bradycardia, or a slow heart rate, is a key sign of third-degree AV heart block. It can cause dizziness and lightheadedness because of poor blood flow. Severe bradycardia can really lower a person’s quality of life.
Fatigue and Exercise Intolerance
Fatigue is another common symptom. The heart can’t speed up when needed, leading to reduced exercise tolerance. This makes it hard for patients to do everyday tasks without getting very tired.
Syncope and Stokes-Adams Attacks
Syncope, or fainting, happens when the heart can’t keep a good rate. This leads to less blood to the brain. Stokes-Adams attacks, a type of syncope, are very scary and might mean someone needs to see a doctor right away.
Risk of Sudden Cardiac Death
People with third-degree AV heart block are at higher risk of sudden cardiac death. This risk shows why quick diagnosis and treatment are so important to avoid serious problems.
| Clinical Presentation | Symptoms | Potential Complications |
| Bradycardia | Dizziness, lightheadedness | Reduced cerebral blood flow |
| Fatigue | Exercise intolerance | Impact on daily activities |
| Syncope | Fainting, Stokes-Adams attacks | Increased risk of injury |
| Sudden Cardiac Death | Life-threatening complications | Mortality |
Essential Fact #3: Major Causes of Third Degree Heart Block
Third-degree AV heart block can come from many conditions. These conditions affect how the heart conducts electrical signals. Knowing these causes helps in managing and treating the condition.
Ischemic Heart Disease and Myocardial Infarction
Ischemic heart disease and myocardial infarction are big reasons for third-degree AV heart block. When blood flow to the heart is cut off, it can harm the heart’s electrical system. Myocardial infarction can scar the heart’s electrical paths, leading to lasting conduction problems.
Degenerative Conduction System Disease
Degenerative conduction system disease is another common cause. It happens when the heart’s electrical system gets scarred and hardened with age. As the system gets worse, the chance of complete heart block goes up.
Medication-Induced AV Block
Some medicines can cause third-degree AV heart block by messing with the AV node. Drugs that slow the heart rate or make the AV node take longer to recover can lead to complete heart block. It’s key to watch patients on these drugs for signs of heart conduction issues.
Congenital and Infiltrative Causes
Congenital heart defects and diseases that spread through the body can also cause third-degree AV heart block. Congenital issues can affect the heart’s structure and its electrical system. Infiltrative diseases, like sarcoidosis or amyloidosis, can invade the heart’s electrical paths, causing problems. Spotting and treating these early is key to avoiding lasting heart damage.
In summary, third-degree AV heart block can stem from many causes. Figuring out and tackling these causes is vital for finding the right treatment and bettering patient results.
Essential Fact #4: Characteristic ECG of 3rd Degree Heart Block
The electrocardiogram (ECG) is key for spotting third-degree AV heart block. It shows clear signs that set it apart from other heart block types. Knowing these ECG signs is vital for correct diagnosis and treatment.
P Waves and QRS Complex Relationship
In third-degree AV heart block, the ECG shows no link between P waves and QRS complexes. This is a key sign of complete heart block. P waves, which show atrial activity, and QRS complexes, which show ventricular activity, happen at different times.
Identifying Complete AV Dissociation
Complete AV dissociation is seen on ECG when P waves and QRS complexes don’t match up. The atrial and ventricular rates are not in sync. Atrial rate is usually faster, while ventricular rate is slower. This is a main sign of third-degree AV heart block.
Rate Differentials Between Atria and Ventricles
The rate difference between atria and ventricles is another important ECG feature. Atrial rate is often normal (60-100 bpm), while ventricular rate is slower (40-60 bpm). This shows the lack of coordination between atrial and ventricular contractions.
Spotting these ECG signs is key to diagnosing third-degree AV heart block. It helps doctors choose the right treatment and care.
Essential Fact #5: Types of Escape Rhythms in Complete Heart Block
In third-degree AV heart block, escape rhythms are key. They help when the normal heart pathway is blocked. The ventricles start an escape rhythm to keep the heart beating.
Junctional Escape Rhythms and Their ECG Features
Junctional escape rhythms start from the AV junction. They beat between 40-60 times per minute. On an ECG, they look almost normal.
This shows the block is likely above the AV node.
Ventricular Escape Rhythms and Their ECG Features
Ventricular escape rhythms start in the ventricles. They beat slower, at 20-40 times per minute. On an ECG, they show a wide QRS complex.
This means the block is further down in the ventricles.
Clinical Implications of Different Escape Rhythms
The type of escape rhythm matters a lot. Junctional rhythms are faster and more stable. They might keep the heart working better than ventricular rhythms.
But, both types might keep blood flowing. Often, we need to pace the heart quickly to help it work better and avoid problems.
Even though escape rhythms save lives, they’re not a permanent fix. The treatment choice depends on the heart block cause and the patient’s health.
Essential Fact #6: Sinus Rhythm with 3rd Degree AV Block Patterns
In third-degree AV block, the heart’s top chamber, the atria, beats regularly. But, the ventricles don’t follow this rhythm. This makes the heart’s rhythm unpredictable, which is a big worry for patients.
Regular P Waves with Independent QRS Complexes
The heart’s electrical activity, shown on an ECG, looks normal at first. The P waves, which show the atria’s rhythm, are regular. But, the QRS complexes, which show the ventricles’ rhythm, don’t match the P waves. This shows a complete break in communication between the atria and ventricles.
The P waves are regular, showing the atria’s rhythm is steady. But, the QRS complexes, which show the ventricles’ rhythm, are different. They don’t follow the P waves. This is a key sign of third-degree AV block.
Differentiating from Other AV Blocks
It’s important to tell third-degree AV block apart from other types. This is because third-degree AV block needs more serious treatment, like a pacemaker. It’s different because there’s no connection between the atria and ventricles.
To spot third-degree AV block, look for no connection between P waves and QRS complexes on the ECG. This is different from other AV blocks where some connection is kept.
Clinical Significance of Preserved Sinus Function
Even with third-degree AV block, the heart’s top chamber keeps beating normally. This helps keep the heart working well, even if the ventricles don’t beat right. Knowing this helps doctors treat patients better.
While the ventricles’ rate is a big worry, the heart’s top chamber helps. This helps doctors treat the heart as a whole, not just the ventricles.
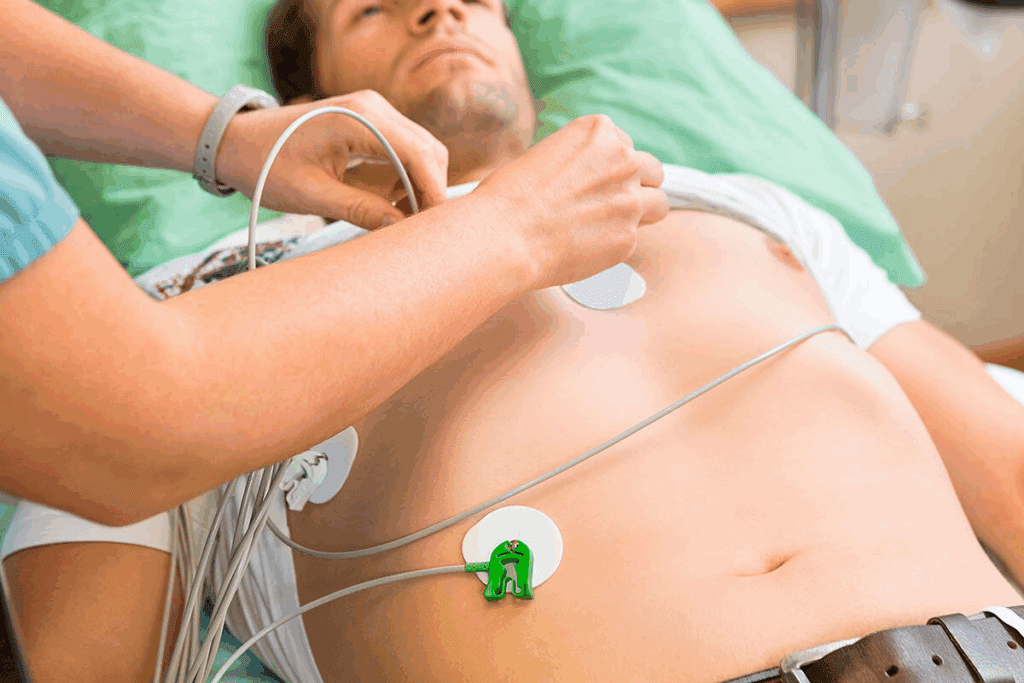
Essential Fact #7: RV Paced ECG Patterns After Pacemaker Placement
After a pacemaker is implanted for third-degree AV heart block, the ECG shows special patterns. These patterns are key to checking if the pacemaker works right. They include pacing spikes, which show the pacemaker’s activity.
Identifying Pacing Spikes on ECG
Pacing spikes are sharp lines on the ECG that show the pacemaker’s signal to the heart. It’s important to spot these spikes to know the pacemaker’s function. The spikes’ size and shape tell us about the pacemaker’s work and how it affects the heart’s electrical activity.
To find pacing spikes, doctors look for sharp, narrow lines on the ECG. These spikes can be positive or negative, based on the lead’s position and the chamber being paced. Spotting these spikes well is key to understanding paced ECGs and making good patient care decisions.
Ventricular vs. Dual Chamber Pacing Patterns
The shape of the paced QRS complexes on ECG changes with ventricular or dual-chamber pacing. Ventricular pacing makes a wide QRS complex because it goes straight to the ventricles. Dual-chamber pacing paces both the atria and ventricles, making the QRS complex look more natural.
Knowing the differences between ventricular and dual-chamber pacing is important for ECG interpretation. Each pacing type has its own use and benefits. The choice depends on the patient’s heart condition and the desired outcome.
Troubleshooting Abnormal Paced Rhythms
Fixing abnormal paced rhythms on ECG is a big part of caring for pacemaker patients. Issues like failure to capture, oversensing, or undersensing can happen. Failure to capture means the pacemaker’s signal doesn’t make the heart depolarize. Oversensing makes the pacemaker think it’s sensing when it’s not, and undersensing means it misses the heart’s natural signals.
To fix these problems, doctors must carefully look at the ECG. They check the pacing spikes, the pacemaker’s capture and sensing, and the heart’s rhythm. They might need to adjust the pacemaker’s settings or check the lead placement to solve the issue.
Understanding RV paced ECG patterns and fixing problems helps healthcare providers improve pacemaker therapy. Good management of pacemaker patients needs a deep understanding of pacing, ECG reading, and solving any issues that come up.
Diagnostic Approach to Third Degree Atrioventricular Block
To diagnose third-degree atrioventricular block, a detailed plan is needed. This includes a clinical check-up and reading ECGs. We’ll cover the main steps and what to think about when diagnosing this condition.
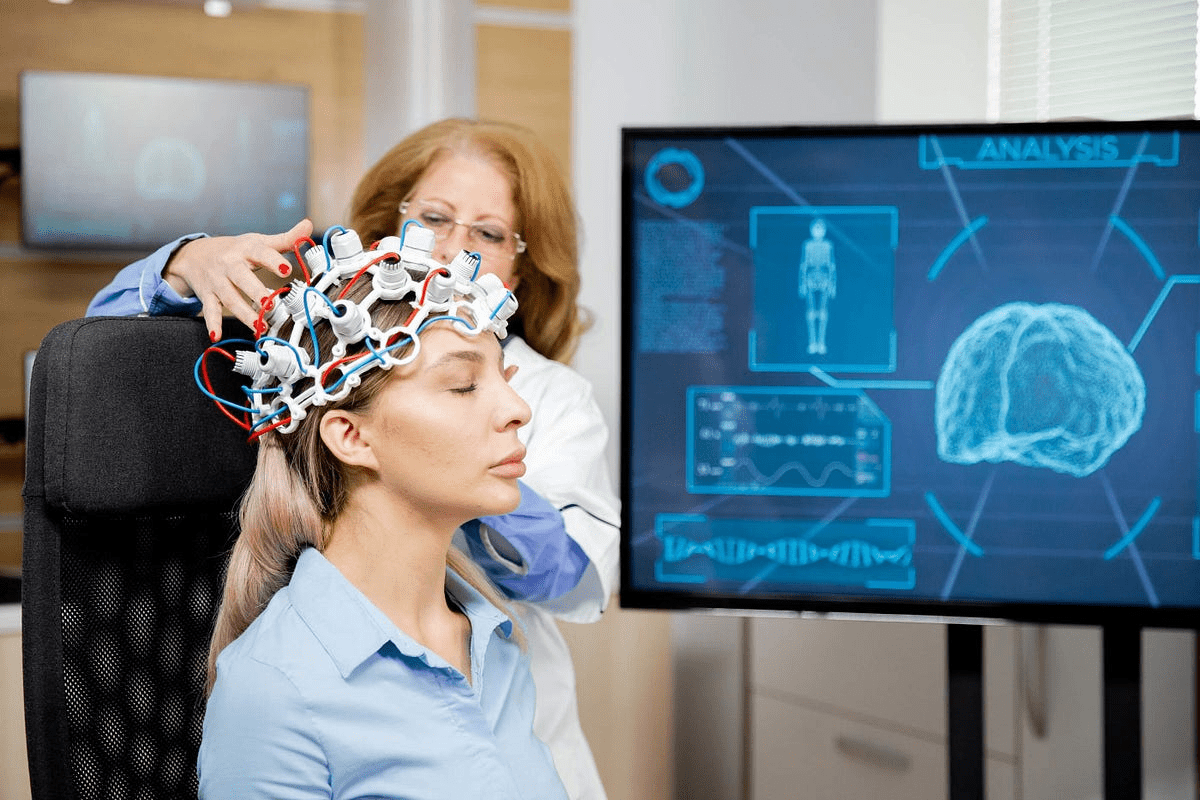
Initial Assessment and ECG Interpretation
When a patient might have third-degree AV block, a full check-up is done. This includes looking at their medical history and doing a physical exam. The ECG is a key tool for spotting complete AV block. Reading ECGs well is important to see the gap between heart beats.
Additional Diagnostic Testing
More tests like echocardiography or stress tests might be done. They help check how well the heart works and find reasons for the block. These tests help doctors understand the heart better and decide what to do next.
Differential Diagnosis Considerations
When diagnosing, other AV block types and conditions that look like third-degree AV block on ECG must be considered. A thorough check is key to confirm the diagnosis and plan treatment. As one study points out,
“Accurate diagnosis of third-degree AV block is critical for appropriate treatment and prevention of complications.”
Emergency Management of Complete Heart Block
Complete heart block is a serious condition that can be life-threatening. When someone has third-degree AV block, we must act fast. Our goal is to keep them stable and prevent more problems.
Temporary Transcutaneous Pacing
One quick fix for complete heart block is temporary transcutaneous pacing. This method uses electrical impulses to keep the heart rate steady. It’s not a permanent fix, but it’s a vital step towards better treatment.
Key aspects of temporary transcutaneous pacing include:
- Rapid initiation to address severe bradycardia
- Use in emergency settings where immediate pacing is required
- Temporary measure until a permanent pacemaker can be implanted
Pharmacological Interventions
Along with pacing, we use medicines to help manage symptoms and heart rate. Atropine or isoproterenol might be used, but their success can vary.
| Medication | Use in Complete Heart Block | Notable Considerations |
| Atropine | May increase heart rate in some cases | Effectiveness can be limited in complete heart block |
| Isoproterenol | Can improve heart rate and contractility | Requires careful monitoring due to possible side effects |
Preparation for Definitive Treatment
The main goal is to get the patient ready for a permanent pacemaker. This means making sure they’re stable, fixing any underlying issues, and planning for the pacemaker.
Preparation steps include:
- Stabilizing the patient’s hemodynamic status
- Evaluating the need for a permanent pacemaker
- Planning for pacemaker implantation, including choosing the right pacemaker
By taking these steps, we help patients with complete heart block get the care they need. This improves their chances of a better life and quality of life.
Long-term Treatment and Pacemaker Therapy
Third-degree AV heart block treatment often includes a permanent pacemaker. This device has changed how we manage this condition. Pacemaker therapy greatly improves life quality and survival for patients.
Indications for Permanent Pacemaker
A permanent pacemaker is usually needed for third-degree AV block. This is true for patients with symptomatic bradycardia, significant pauses, or poor escape rhythms. Symptoms like bradycardia really affect a patient’s life quality.
- Symptomatic bradycardia
- Significant pauses or asystole
- Inadequate escape rhythms
- Post-myocardial infarction third-degree AV block
Types of Pacemakers and Selection Criteria
There are single-chamber and dual-chamber pacemakers available. The right one depends on the patient’s needs and health. Dual-chamber pacemakers are often chosen because they keep the heart beating in sync.
| Type of Pacemaker | Characteristics | Selection Criteria |
| Single-Chamber | Paces either the atrium or ventricle | Used in patients with chronic atrial fibrillation |
| Dual-Chamber | Paces both atrium and ventricle | Preferred for maintaining AV synchrony |
Post-Implantation Care and Monitoring
After the pacemaker is put in, it’s important to check how it’s working. Adjustments might be needed, and patients should know about any lifestyle changes. Regular check-ups help keep the pacemaker working well and catch any problems early.
Knowing about pacemaker use helps doctors give better care to patients with third-degree AV heart block. This leads to better outcomes for these patients.
Conclusion
Knowing the basics about third degree AV heart block is key for diagnosis and treatment. This serious condition blocks all electrical signals from the atria to the ventricles. It needs quick action and treatment.
We talked about the main ECG signs, like complete AV dissociation and escape rhythms. These are vital for spotting this issue. Treatments like pacemakers can greatly help patients, improving their life quality.
Healthcare teams can offer top care by spotting the signs early and acting fast. Our aim is to give full support and the latest medical care to patients from around the world. We want the best results for them.
FAQ
What is third degree AV heart block?
Third degree AV heart block, also known as complete heart block, is a serious heart condition. It happens when electrical signals from the atria to the ventricles are completely blocked. This causes the atria and ventricles to beat on their own.
What are the symptoms of third degree AV heart block?
Symptoms include severe slow heart rate, tiredness, and trouble exercising. People may also experience fainting and Stokes-Adams attacks. These happen because the heart doesn’t pump enough blood.
What causes third degree AV heart block?
It can be caused by heart disease, heart attacks, or damage to the heart’s electrical system. Medications, birth defects, and diseases that spread to the heart can also cause it.
How is third degree AV heart block diagnosed?
Doctors use an electrocardiogram (ECG) to diagnose it. The ECG shows that the heart’s electrical signals are not working together properly.
What are the characteristic ECG findings of third degree AV heart block?
The ECG shows that the heart’s electrical signals are not synchronized. This means the atria and ventricles beat at different rates. The atria usually beat faster than the ventricles.
What is the role of escape rhythms in third degree AV heart block?
The ventricles often start an escape rhythm to keep the heart beating. This rhythm can be from the junction or ventricles. But, it’s often not enough to keep the heart working well.
How is third degree AV heart block treated?
Treatment usually involves a permanent pacemaker to help the heart beat at a normal rate. In emergencies, temporary pacing or medication may be used.
What are the different types of pacemakers used to treat third degree AV heart block?
There are different pacemakers, like single-chamber and dual-chamber ones. The choice depends on the patient’s needs and health situation.
What is the significance of preserved sinus function in third degree AV heart block?
Having preserved sinus function means the atria can help the heart some. But, the main problem is the ventricles beating too slow.
How is pacemaker function monitored after implantation?
After the pacemaker is put in, it’s checked regularly. The settings might need to be changed. Patients also need to know about any lifestyle changes or precautions.
References
- Camasão, D. B., & Mantovani, D. (2021). The mechanical characterization of blood vessels and their substitutes in the continuous quest for physiologically relevant performances: A critical review. Mechanics Research Communications, 114, 103655. https://www.sciencedirect.com/science/article/pii/S2590006421000144