A thoracic aortic aneurysm is a serious condition. It happens when the aorta, the main blood vessel, balloons out in the chest. This can be very dangerous if not treated quickly. Medical experts say that quick diagnosis and treatment are key.How do they fix a thoracic aortic aneurysm? thoracic aortic aneurysm icd 10 Learn the crucial repair methods and the powerful surgical and endovascular options today.
At our medical center, we use the latest methods to treat tortuous thoracic aorta and other related issues. The icd10 code for thoracic aortic aneurysm is important for diagnosis and insurance. We focus on clear communication and caring for our patients with this condition.
Key Takeaways
- Thoracic aortic aneurysm is a serious condition requiring prompt medical attention.
- The icd10 code for thoracic aortic aneurysm is important for diagnosis.
- Timely treatment can greatly improve patient outcomes.
- Our medical team uses the latest techniques for treatment.
- Compassionate care is a key part of our treatment approach.
Understanding Thoracic Aortic Aneurysms

It’s important to know about thoracic aortic aneurysms to treat them. These occur when the aorta, a key blood vessel, expands in the chest area.
Definition and Pathophysiology
A thoracic aortic aneurysm is when the aorta gets bigger than 1.5 times its normal size. It happens due to damage to the aorta’s walls and inflammation.
The tortuosity of the thoracic aorta also affects aneurysm development. Tortuosity means the aorta twists, raising the risk of aneurysms.
Prevalence and Risk Factors
Thoracic aortic aneurysms are less common than abdominal ones. They become more common with age. Certain factors increase the risk, such as:
- Hypertension
- Atherosclerosis
- Genetic disorders (e.g., Marfan syndrome, Ehlers-Danlos syndrome)
- Family history of aortic aneurysms
- Smoking
Knowing these risk factors helps in early detection and management.
Natural History and Progression
The course of thoracic aortic aneurysms depends on their size, location, and cause. Small ones might not change, but big ones are more likely to rupture. The size criteria for treatment are key.
The ascending aortic aneurysm size is important for deciding when to operate. Guidelines suggest surgery for aneurysms over a certain size.
Regular check-ups are vital for those with thoracic aortic aneurysms. This helps prevent serious problems and improves their health.
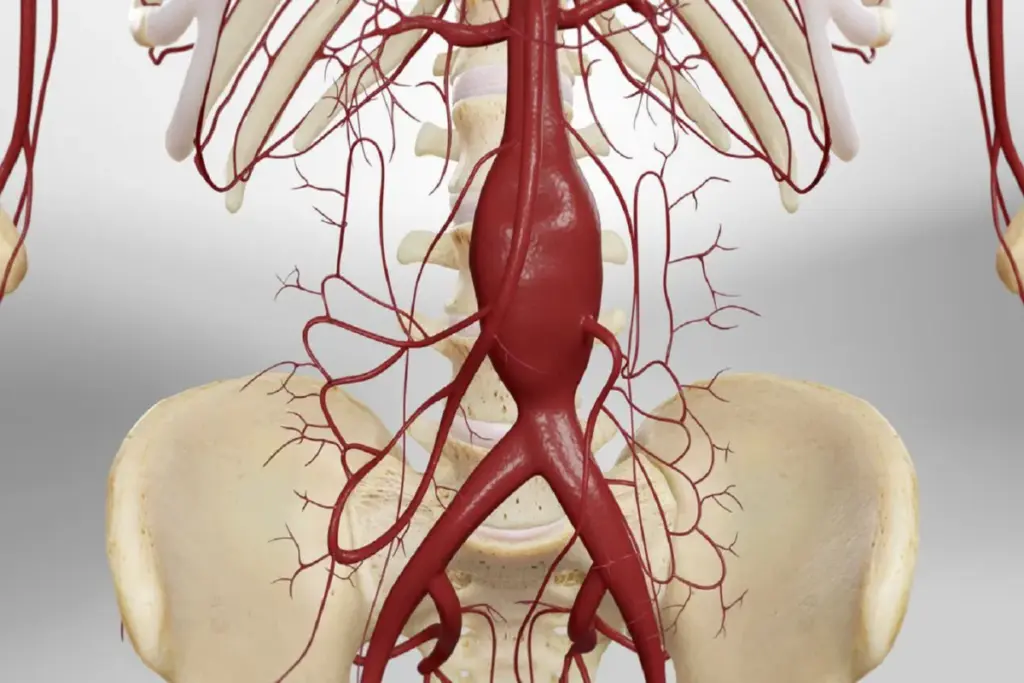
Anatomy of the Thoracic Aorta

The thoracic aorta is key to our heart’s health. Knowing its anatomy is vital for treating aneurysms. We’ll look at its segments, branches, and size to understand it fully.
Segments of the Thoracic Aorta
The thoracic aorta has three main parts: the ascending aorta, the aortic arch, and the descending thoracic aorta. Each part is unique and important for the aorta’s function.
The ascending aorta starts at the left ventricle and reaches the sternal angle. The aortic arch then curves backward and left, becoming the descending thoracic aorta. This part goes through the thoracic cavity.
Branches of the Thoracic Aorta
The thoracic aorta has several branches that supply blood to different areas. The brachiocephalic trunk, left common carotid artery, and left subclavian artery are among them. Knowing these branches is key for treating thoracic aortic aneurysms.
These branches are vital for the head, neck, and upper limbs. Any issues with them can cause serious problems.
Normal Size Parameters
The thoracic aorta’s size changes along its length. The ascending aorta is usually 2.8 to 3.8 cm wide. The descending thoracic aorta is smaller, about 2.0 to 2.5 cm wide. Knowing these sizes helps spot aneurysms.
To better understand, here’s an image of the thoracic aorta’s anatomy:
Understanding the thoracic aorta’s normal anatomy and sizes helps doctors diagnose and treat aneurysms. This improves patient care.
Types of Thoracic Aortic Aneurysms
The thoracic aorta can develop aneurysms in different segments. Each segment has its own clinical implications. Knowing these differences is key to finding the best treatment.
Ascending Aortic Aneurysms
Ascending aortic aneurysms happen in the part of the aorta closest to the heart. They can affect the aortic root and the aortic valve. Symptoms often don’t show until the aneurysm gets big enough to cause problems or rupture.
“Early detection is key to preventing complications,” say cardiovascular specialists.
Aortic Arch Aneurysms
Aortic arch aneurysms happen in the curved part of the aorta. This part supplies blood to the head and upper body. These aneurysms are hard to treat because they’re close to the brain’s blood supply. Careful planning is needed to protect the brain during repair.
Descending Thoracic Aortic Aneurysms
Descending thoracic aortic aneurysms happen in the part of the aorta that goes down through the chest. These aneurysms can be very serious if they rupture. Monitoring and timely intervention are critical to prevent bad outcomes.
Thoracoabdominal Aortic Aneurysms
Thoracoabdominal aortic aneurysms go from the chest into the abdominal aorta. These complex aneurysms need special treatment plans. “The management of thoracoabdominal aortic aneurysms is a big challenge in vascular surgery,” say experts.
Each type of thoracic aortic aneurysm has its own challenges. A tailored approach is needed for each one. Understanding these differences is key to providing the best care.
Diagnosis and Clinical Presentation
Diagnosing thoracic aortic aneurysms can be tricky. It’s key to catch it early for the best treatment.
Symptoms and Signs
Most thoracic aortic aneurysms don’t show symptoms until they burst or press on nearby tissues. Symptoms like chest pain, back pain, or trouble swallowing can happen. Spotting these signs early is critical for quick action.
Some people might feel hoarseness or have trouble breathing due to the aneurysm. Because symptoms vary, finding the right diagnosis can be tough.
Physical Examination Findings
Physical checks might not always point to a thoracic aortic aneurysm. Yet, finding a pulsatile mass or hearing a murmur can hint at its presence.
It’s important to do a detailed physical exam. Look at the pulses and blood pressure in both arms. Any differences could mean a problem with the aorta.
Screening Recommendations
Screening for thoracic aortic aneurysms isn’t for everyone. But, it’s advised for those with a family history or genetic conditions like Marfan syndrome.
For those at high risk, we suggest using ultrasound or CT scans for early detection.
The Thumb Test for Aortic Aneurysm
The thumb test, or Steinberg sign, is a simple way to check for an aortic root aneurysm. It’s often used in Marfan syndrome patients. You check if the thumb goes past the ulnar border when you overlap your fingers.
This test is just one part of a full check-up that includes imaging and other tests.
Imaging Techniques for Diagnosis
Imaging is key in finding and treating thoracic aortic aneurysms. Knowing the aneurysm’s size, shape, and where it is helps doctors choose the right treatment.
Computed Tomography Angiography (CTA)
CTA is great for spotting thoracic aortic aneurysms. It uses CT scans with contrast to see the aorta and its branches. CTA shows the aneurysm’s details and how it fits with nearby structures.
CTA is easy to find, quick, and shows clear images. But, it uses harmful radiation and contrast that can hurt the kidneys.
Magnetic Resonance Angiography (MRA)
MRA is also good for checking thoracic aortic aneurysms. It uses MRI with or without contrast to see the aorta. MRA is best for those who can’t have CTA because of kidney issues or contrast allergies.
MRA gives great images without radiation. But, it’s not as common as CTA, and it takes longer to get images.
Echocardiography and TEE
Echocardiography, like TTE and TEE, helps with thoracic aortic aneurysms, mainly in the ascending aorta. TEE gives clear aorta pictures, perfect for surgery.
Echocardiography is safe and doesn’t use radiation. But, it depends on the person doing it, and it might miss parts of the aorta.
Aortography and X-ray Findings
Aortography is not as common now but can give important aorta info. It injects contrast into the aorta to see its inside.
Aortography shows the aorta’s inside well but is risky. It can cause bleeding and harm to blood vessels.
Thoracic Aortic Aneurysm ICD-10 Coding and Classification
Accurate ICD-10 coding for thoracic aortic aneurysms is key for medical records and billing. We’ll look into the details of ICD-10 coding for these aneurysms. This includes codes for different types and complications.
ICD-10 Codes for Different Types of Thoracic Aneurysms
The ICD-10 system has specific codes for thoracic aortic aneurysms. For example, aneurysms of the thoracic aorta are coded based on their location and type.
The code for a thoracic aortic aneurysm, unspecified, is I71.2. There are more specific codes for aneurysms in different parts of the thoracic aorta.
Coding for Complications and Rupture
When a thoracic aortic aneurysm ruptures, the coding changes. The ICD-10 code for a ruptured thoracic aortic aneurysm is under I71. Specific subcodes show the rupture.
Rupture is a serious medical emergency. Accurate coding is vital for managing the patient and billing.
Documentation Requirements for Proper Coding
Proper documentation is key for accurate ICD-10 coding. It includes details on the aneurysm’s location, size, and complications.
Healthcare providers must document thoroughly. This supports the chosen ICD-10 codes.
|
Description |
ICD-10 Code |
|---|---|
|
Thoracic aortic aneurysm, unspecified |
I71.2 |
|
Ruptured thoracic aortic aneurysm |
I71.1 |
|
Thoracic aortic aneurysm, dissected |
I71.0 |
Size Criteria and Guidelines for Intervention
Managing thoracic aortic aneurysms involves size criteria and guidelines. These factors greatly affect patient outcomes and treatment success. They help us decide when to perform surgery or use endovascular methods.
Guidelines for Ascending Aortic Aneurysms
For ascending aortic aneurysms, surgery is usually recommended when the aneurysm is over 5.5 cm. But, this size can change based on the patient’s health and genetic conditions like Marfan syndrome. In such cases, surgery might be needed at a smaller size.
The aneurysm’s growth rate is also key. Aneurysms growing fast (more than 0.5 cm a year) might need surgery sooner, even if they’re not yet 5.5 cm.
Guidelines for Descending Thoracic Aneurysms
Descending thoracic aortic aneurysms have their own guidelines. Surgery is often considered when the aneurysm is over 6.0 to 6.5 cm. The decision also depends on symptoms, the patient’s health, and the aneurysm’s shape.
Endovascular repair is becoming more common for these aneurysms, mainly for patients at high risk for open surgery.
Aortic Root Dilatation Guidelines
Aortic root dilatation can lead to aneurysm formation. Guidelines suggest surgery when the aortic root is over 5.0 cm in patients with Marfan syndrome or similar high-risk conditions.
For those without these conditions, surgery is recommended at a diameter of 5.5 cm or more.
Growth Rate Considerations
The rate at which an aneurysm grows is very important. Fast-growing aneurysms are at higher risk of rupture and might need treatment sooner.
- Monitoring: Regular imaging is key to track aneurysm growth.
- Risk Assessment: Doctors must weigh the risk of rupture against the risks of treatment.
- Personalized Care: Treatment plans should be tailored to each patient, considering their health, aneurysm details, and genetic factors.
By following these guidelines, we can better manage thoracic aortic aneurysms. This improves patient outcomes and lowers the risk of rupture.
Preoperative Assessment and Risk Stratification
Before surgery, doctors carefully assess and classify the risks for patients with thoracic aortic aneurysms. This detailed check helps spot possible dangers. It lets doctors plan how to lower these risks.
Cardiac Evaluation
Checking the heart is key for patients getting thoracic aortic aneurysm repair. Doctors look at the patient’s health history, ECG results, and echocardiography. They check the heart’s function and look for heart disease.
Key components of cardiac evaluation:
- Medical history review
- Electrocardiogram (ECG)
- Echocardiography
- Stress testing (if necessary)
- Coronary angiography (if indicated)
Pulmonary Function Assessment
Assessing the lungs is important for patients. It helps predict breathing problems after surgery. Tests include spirometry, lung volume measurements, and blood gas analysis.
|
Pulmonary Function Test |
Normal Value |
Interpretation |
|---|---|---|
|
Spirometry (FEV1) |
80-120% predicted |
Assesses airway obstruction |
|
Lung Volume Measurements |
Within normal limits |
Evaluates lung volume and capacity |
|
Arterial Blood Gas Analysis |
pH 7.35-7.45, PaCO2 35-45 mmHg |
Assesses gas exchange and ventilation |
Renal Function Evaluation
Checking the kidneys is vital for patients. It helps predict kidney problems after surgery. Doctors look at serum creatinine, eGFR, and urine output.
Risk Scoring Systems
Doctors use risk scoring systems like EuroSCORE II to predict surgery outcomes. These systems consider age, health conditions, and surgery complexity.
Common risk scoring systems:
- EuroSCORE II
- Society of Thoracic Surgeons (STS) Score
- Cardiac Anesthesia Risk Evaluation (CARE) score
Non-Surgical Management Options
Non-surgical methods are key in treating thoracic aortic aneurysms. They are important for those not ready for surgery or as a support to surgery.
Blood Pressure Control Medications
Keeping blood pressure in check is vital for thoracic aortic aneurysms. Antihypertensive medications lower aortic wall pressure, slowing aneurysm growth. We often use ACE inhibitors or calcium channel blockers for this.
Beta-Blocker Therapy
Beta-blockers are a mainstay in non-surgical management. They lessen heart contraction force and heart rate, reducing aortic wall stress. Beta-blocker therapy slows aneurysm growth and is advised for specific aortic aneurysms.
Lifestyle Modifications
Lifestyle changes are critical in managing thoracic aortic aneurysms. Quitting smoking is essential, as it’s a major risk factor. Eating well, exercising, and managing stress also boost cardiovascular health.
Monitoring Protocols for Small Aneurysms
Small aneurysms need regular checks for size changes. We use CT or MRI scans to monitor growth. This helps us adjust treatment plans and consider surgery if needed.
Combining these non-surgical methods helps manage thoracic aortic aneurysms well. It’s a detailed approach that tackles the condition’s many aspects.
Indications for Surgical Intervention
Knowing when to choose surgery for thoracic aortic aneurysms is key to avoiding rupture and keeping patients safe. The choice to operate is based on a detailed look at several factors.
Size-Based Criteria
The size of the aneurysm is a big factor in deciding if surgery is needed. Aneurysms that are bigger are more likely to burst. For example, those over 5.5 cm in diameter usually need surgery. But, this can change based on the patient’s health and the aneurysm’s details.
Symptom-Based Criteria
Aneurysms that cause symptoms, like chest pain or trouble breathing, often need surgery. Symptoms can mean the aneurysm is more urgent to fix.
Emergency Indications
When an aneurysm ruptures or dissects, surgery is urgent. These situations are very serious and need quick action. The aim of emergency surgery is to keep the patient stable and avoid more harm.
Special Considerations for High-Risk Patients
For those at high risk of surgery problems, the decision is made with extra care. Age, health issues, and overall well-being are all looked at closely. Sometimes, other treatments or a wait-and-see approach might be better.
We look at each patient’s unique case to decide the best action. Surgery is always weighed against the patient’s health and the aneurysm’s specifics.
Open Surgical Repair Techniques
Open surgical repair is key for treating thoracic aortic aneurysms. It offers hope to those with complex aortic issues. We use it to fix different parts of the thoracic aorta, giving our patients the care they need.
Ascending Aorta and Root Repair
Fixing the ascending aorta and root is a detailed job. We use a median sternotomy to get to the aorta. Cardiopulmonary bypass is essential for safely putting in a new graft.
In cases of the aortic root, we might do a Bentall procedure or a valve-sparing root replacement. This depends on what the patient needs.
Key steps in ascending aorta repair include:
- Careful dissection of the aorta
- Establishment of cardiopulmonary bypass
- Resection of the aneurysmal segment
- Implantation of a prosthetic graft
Aortic Arch Repair Procedures
Aortic arch repair is tough because of its role in blood flow to the brain. We use deep hypothermic circulatory arrest and selective antegrade cerebral perfusion. This keeps the brain blood flowing during surgery.
The extent of arch replacement can vary. It depends on how big the aneurysm is.
Descending Thoracic Aorta Repair
Fixing the descending thoracic aorta usually means a left thoracotomy. We figure out how big the aneurysm is to plan the best surgery. We use distal aortic perfusion and cerebrospinal fluid drainage to protect the spinal cord.
Important considerations for descending thoracic aorta repair include:
- Preoperative planning to assess the aneurysm’s extent
- Intraoperative monitoring to detect spinal cord ischemia
- Postoperative care to manage possible complications
By using these open surgical repair methods, we can treat thoracic aortic aneurysms well. This improves our patients’ outcomes.
Endovascular Repair Procedures
Endovascular repair has changed how we treat thoracic aortic aneurysms. It’s a less invasive method than traditional surgery. This approach has made recovery faster and reduced surgery risks. We’ll look at endovascular techniques like TEVAR, hybrid procedures, and fenestrated and branched endografts.
Thoracic Endovascular Aortic Repair (TEVAR)
TEVAR is a minimally invasive method. It involves placing a stent-graft in the aorta to block the aneurysm from blood flow. This stops the aneurysm from getting bigger or rupturing. The stent-graft is put in through the femoral artery, guided by X-rays.
TEVAR has many benefits. It lowers the risk of complications and death compared to open surgery. Patients also have shorter hospital stays and less pain after surgery. But, it’s important to choose the right patients for this treatment.
Hybrid Procedures
Hybrid procedures mix open surgery with endovascular repair for complex aortic aneurysms. They’re great for aneurysms that affect the aortic arch or thoracoabdominal aorta. This method offers a customized treatment plan for complex cases.
For example, a hybrid procedure might include a surgical bypass to fix critical aortic branches. Then, an endovascular stent-graft is placed to cover the aneurysm. This way, complex aneurysms can be treated with less open surgery.
Fenestrated and Branched Endografts
Fenestrated and branched endografts are advanced devices for treating aortic aneurysms with critical branch vessels. Fenestrated endografts have openings for branch vessel perfusion. Branched endografts have dedicated branches for aortic branch connection.
|
Device Type |
Description |
Clinical Use |
|---|---|---|
|
Fenestrated Endografts |
Endografts with fenestrations for branch vessel perfusion |
Aneurysms involving critical aortic branches |
|
Branched Endografts |
Endografts with dedicated branches for aortic branches |
Complex thoracoabdominal aortic aneurysms |
In conclusion, endovascular repair procedures like TEVAR, hybrid procedures, and fenestrated and branched endografts are big steps forward in treating thoracic aortic aneurysms. These methods offer patients less invasive options than traditional surgery. They have the chance to improve outcomes and reduce recovery times.
Special Patient Populations
Managing thoracic aortic aneurysms is complex. It needs special plans for different groups. Some patients face unique challenges because of their health, age, or family history.
Marfan Syndrome Management
Marfan syndrome patients face a big challenge. They are at high risk for aortic root dilatation and aneurysms. Early diagnosis and monitoring are key to prevent serious problems. We suggest regular echocardiography and MRI to watch aortic size and decide on surgery.
Other Genetic Aortopathies
Other genetic conditions like Ehlers-Danlos syndrome and Loeys-Dietz syndrome also raise the risk of aortic aneurysms. Genetic counseling and testing are important to find at-risk family members. A team of doctors and geneticists work together to manage these conditions.
Elderly Patients
Elderly patients with aortic aneurysms face extra challenges. They often have other health issues and are less able to recover. A thorough check before surgery is vital. We look at heart, lung, and kidney health to decide the best treatment.
Familial Aortic Aneurysm Disease
Familial thoracic aortic aneurysms and dissections (FTAAD) run in families without known genetic syndromes. Screening first-degree relatives is advised. This can lead to better outcomes. We watch for aneurysms and may suggest surgery based on size and growth.
Postoperative Care and Rehabilitation
After thoracic aortic aneurysm surgery, postoperative care and rehabilitation are key. We aim to prevent complications, help healing, and improve function. This is vital for patient recovery.
Immediate Postoperative Management
Right after surgery, patients are closely watched in an ICU. We focus on managing pain, keeping blood pressure stable, and supporting breathing. This helps them recover smoothly. A study says the first 24-48 hours are very important.
We watch for bleeding, organ problems, and brain function. Pain is managed with a mix of epidural and IV drugs.
Common Complications
Even with better surgery, complications can happen. These include breathing issues, kidney problems, and spinal cord damage. Spotting and treating these early is key to avoid lasting harm.
A study found spinal cord problems occur in 3% to 10% of patients. This shows why constant monitoring is essential.
Recovery Timeline and Rehabilitation
Recovery time varies based on surgery type and patient health. Usually, it takes months to fully recover. A structured rehab program is vital for better function and life quality.
Rehab includes physical therapy, nutrition advice, and mental support. “A good rehab plan can greatly improve recovery and lower heart risks,” a specialist said.
By focusing on detailed post-op care and rehab, we can better help patients after thoracic aortic aneurysm surgery.
Conclusion
Managing thoracic aortic aneurysms needs a detailed plan. This includes the latest diagnostic tools, tailored treatments, and careful follow-up care. At our institution, we aim to offer top-notch healthcare to international patients with thoracic aortic aneurysm.
Our team works together with patients to meet their specific needs. We use the newest medical technology and treatment methods. Our goal is to improve our patients’ lives and achieve the best results.
We keep improving our treatment for thoracic aortic aneurysms. Our promise is to give our patients the best care, support, and advice at every step. We believe this approach is key to the best outcomes for our patients.
FAQ
What is a thoracic aortic aneurysm?
A thoracic aortic aneurysm occurs when the aorta in the chest expands excessively, potentially affecting any section of the vessel.
What are the risk factors for developing a thoracic aortic aneurysm?
Risk factors include high blood pressure, smoking, and atherosclerosis. Also, genetic conditions like Marfan syndrome and family history of aortic aneurysms play a role.
How is a thoracic aortic aneurysm diagnosed?
Doctors use imaging like CT angiography, MRI, or echocardiography to diagnose. They might do this if you have symptoms or if they find something during another test.
What are the symptoms of a thoracic aortic aneurysm?
Symptoms include chest or back pain, shortness of breath, coughing, or trouble swallowing. But many aneurysms don’t show symptoms until they burst.
How is the size of a thoracic aortic aneurysm measured?
Doctors use CT or MRI to measure the size. They look at the biggest part of the aneurysm to decide if it’s a risk and if it needs treatment.
What is the thumb test for aortic aneurysm?
The thumb test isn’t a standard way to check for aneurysms. But, doctors might use pulse checks and other tests to look for them. Imaging is the best way to confirm a diagnosis.
What are the guidelines for intervening in a thoracic aortic aneurysm?
Guidelines say to operate if the aneurysm is big, growing fast, causing symptoms, or if your health is at risk.
What are the treatment options for thoracic aortic aneurysms?
Treatment depends on the size and growth of the aneurysm. Options include watching it closely, taking medicine, open surgery, or endovascular repair like TEVAR.
What is TEVAR?
TEVAR is a minimally invasive procedure. It involves placing a stent-graft in the aorta to block blood flow to the aneurysm.
How is Marfan syndrome managed in relation to thoracic aortic aneurysms?
Managing Marfan syndrome means regular aorta checks, beta-blockers to slow growth, and sometimes surgery early on.
What is the importance of postoperative care after thoracic aortic aneurysm repair?
Postoperative care is key to watch for and manage complications. It helps ensure healing and improves recovery and long-term health.
Can lifestyle modifications help manage thoracic aortic aneurysms?
Yes, changes like quitting smoking, controlling blood pressure, exercising, and eating well can help manage the condition and lower risks.
What is the ICD-10 code for thoracic aortic aneurysm?
The ICD-10 code for thoracic aortic aneurysm is I71.2. Codes vary based on whether it’s dissecting or non-dissecting and other details.
How often should a thoracic aortic aneurysm be monitored?
Monitoring frequency depends on the aneurysm’s size and growth, and your health. Small aneurysms are usually checked every 6 to 12 months.
References
Centers for Disease Control and Prevention. Evidence-Based Medical Insight. Retrieved from https://www.cdc.gov/heartdisease/aortic_aneurysm.htm








