Last Updated on November 13, 2025 by

Unexplained bruising can be a worrying sign. It might mean there’s a blood disorder. Thrombocytopenia, or a low platelet count, is a big risk for bruising and bleeding. Can thrombocytopenia bruising cause? Yes. Understand this unlucky side effect and why low platelets lead to excessive bleeding.
With fewer platelets, the body can’t make blood clots well. This makes it easy to bruise and bleed. This issue can hit people with certain health problems or those on certain meds.
We’ll dive into how thrombocytopenia connects to bruising and bleeding. Our experts will also cover the causes and treatments.
Key Takeaways
- Thrombocytopenia is a condition with a low platelet count.
- A low platelet count can lead to more bruising and bleeding.
- Certain health issues or meds can cause thrombocytopenia.
- Knowing the causes of thrombocytopenia is key to good treatment.
- Our experts will talk about the treatments for thrombocytopenia.
Understanding Thrombocytopenia
Thrombocytopenia is a condition where you have too few platelets in your blood. It’s a big health issue that affects many people around the world. To get what thrombocytopenia means, you need to know about platelets and their role in your body.
Definition of Thrombocytopenia
Thrombocytopenia happens when your platelet count is lower than it should be. Platelets, or thrombocytes, are small blood cells that help your blood clot. A healthy platelet count is between 150,000 and 450,000 per microliter of blood.
If your count falls below 100,000 platelets per microliter, you have thrombocytopenia.
Normal Platelet Count vs. Low Platelet Count
A normal platelet count is key for your body to clot blood and stop bleeding. But if your count is low, you’re more likely to bleed. A 2024 study found that 40.3% of people with thrombocytopenia showed signs of bleeding.
Knowing the difference between a normal and low platelet count is important for treating thrombocytopenia.
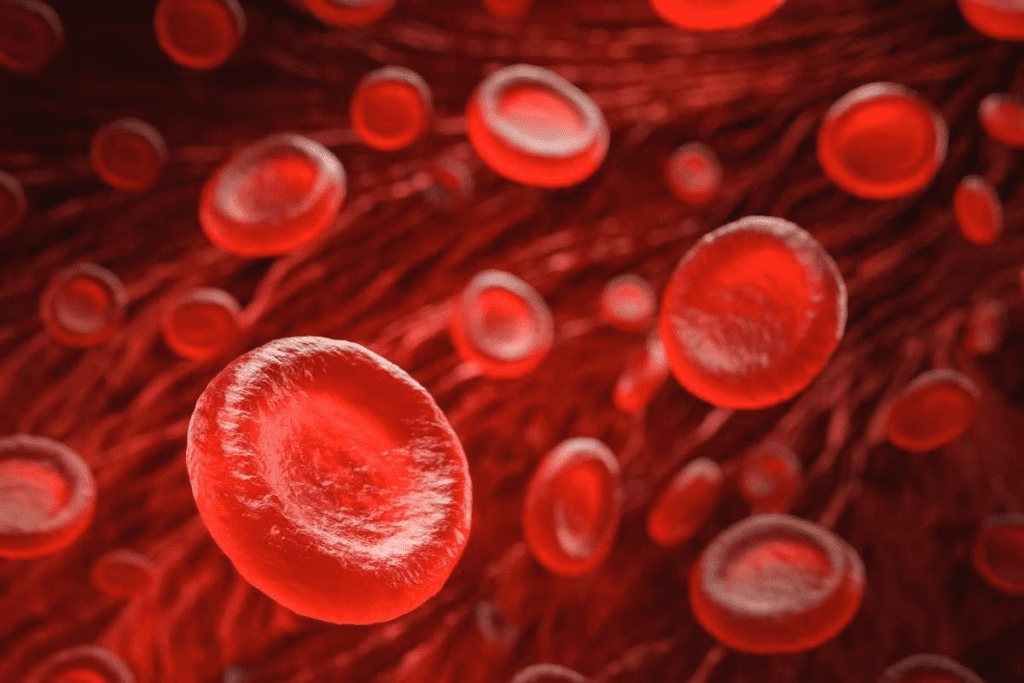
The Role of Platelets in Blood Clotting
Platelets are vital for blood clotting. They stick to injuries in blood vessels, form a plug, and then get strengthened by fibrin. This stops bleeding. But with thrombocytopenia, there are fewer platelets, making it harder to stop bleeding.
In short, to understand thrombocytopenia, you need to know its definition, the normal platelet count, and how platelets help with clotting. This knowledge is key to diagnosing and treating the condition.
The Relationship Between Thrombocytopenia and Bruising
Thrombocytopenia is when you have too few platelets. Platelets help your blood clot. Without enough, you might bruise easily and bleed more.
How Low Platelet Count Leads to Bruising
Low platelets make it hard for your body to clot blood. This means even small injuries can cause big bruises. The severity of bruising can vary depending on the degree of thrombocytopenia.
Platelets usually form a plug at injury sites to stop bleeding. But with fewer platelets, this plug might not form well. This leads to more bleeding and bruising.

Statistical Evidence of Thrombocytopenia Causing Bruising
Research shows that many people with thrombocytopenia get bruises. About 8% say they bruise easily. Also, studies find that 0.14 per 100,000 people have thrombocytopenia with bruising.
The link between thrombocytopenia and bruising is clear from studies. It shows why treating thrombocytopenia is key to preventing bruising and bleeding.
Knowing how thrombocytopenia causes bruising is vital. It helps doctors and patients make better choices. This knowledge can lead to better health outcomes.
Clinical Manifestations of Thrombocytopenia
Knowing the symptoms of thrombocytopenia is key to early treatment. This condition, marked by low platelet count, can cause various bleeding issues. We’ll look at common symptoms, the range of bleeding severity, and when to see a doctor.
Common Symptoms Beyond Bruising
People with thrombocytopenia may have symptoms beyond just bruising. They might see bleeding gums, easy bruising, and prolonged bleeding from small cuts. Some notice petechiae, small red or purple spots, often on the legs or where skin is pressed.
Severe symptoms include internal bleeding, like blood in urine or stool, or intracranial hemorrhage in extreme cases. Women might face heavy menstrual periods, which is a big worry.
Severity Spectrum of Bleeding Manifestations
The severity of bleeding in thrombocytopenia depends on the platelet count. Those with higher counts might have mild symptoms, while very low counts can lead to severe bleeding. Bleeding can range from mild oozing to life-threatening hemorrhages.
The risk of bleeding grows as platelet counts drop. For example, counts below 30,000/mm ³ increase the risk of serious bleeding.
When to Seek Medical Attention
People with thrombocytopenia need to know when to get medical help. If you have severe bleeding, headaches, or confusion, seek help right away. These could be signs of a serious problem.
Also, if you see blood in your urine or stool, or have heavy or prolonged menstrual bleeding, see your doctor quickly.
Types of Bruising Associated with Thrombocytopenia
Bruising from thrombocytopenia can show up in different ways. These include petechiae, ecchymosis, and purpura. Knowing these types helps doctors diagnose and treat the condition better.
Petechiae: Small Red or Purple Spots
Petechiae are small dots on the skin from tiny capillary bleeding. They look like a rash and are common in people with low platelet counts. These spots are usually painless but can be a clear sign of thrombocytopenia.
Ecchymosis: Larger Bruised Areas
An ecchymosis a bigger bruise from bleeding into the skin or mucous membranes. These bruises can be big and happen after just a little injury. Without enough platelets, people with thrombocytopenia might get bigger bruises.
Purpura: Purple-Colored Patches on Skin
Purpura shows as purple patches on the skin from bleeding under the skin. It can be small or big and often means a low platelet count. Seeing purpura can be a warning sign of serious thrombocytopenia and needs quick doctor visits.
Our study shows that about 71.7% of cases with platelet counts under 30,000/mm ³ had more serious bleeding. Spotting these signs early is key to managing thrombocytopenia well.
Causes of Thrombocytopenia
Thrombocytopenia is a complex condition with many causes. These include decreased platelet production, increased destruction, and effects from medications. Knowing these causes helps in diagnosing and managing the condition.
Decreased Platelet Production
One main cause of thrombocytopenia is when the bone marrow doesn’t make enough platelets. This can happen due to bone marrow failure, leukemia, or myelodysplastic syndromes. When the bone marrow can’t produce enough platelets, it leads to thrombocytopenia.
Increased Platelet Destruction
Another cause of thrombocytopenia is when platelets are destroyed faster than they can be made. This can happen in conditions like Immune Thrombocytopenia (ITP). In ITP, the immune system attacks platelets, leading to their destruction. ITP is a common cause of thrombocytopenia, showing how important the immune system is in this condition.
For more information on ITP and its management, we can refer to resources that provide detailed insights into the condition, such as the article on thrombocytopenia from the American Academy of Family Physicians.
Medication-Induced Thrombocytopenia
Certain medications can cause thrombocytopenia by either reducing platelet production or increasing their destruction. Common culprits include heparin, certain antibiotics, and anticonvulsants. Medication-induced thrombocytopenia is a significant concern, as it can often be resolved by stopping the offending medication.
The causes of thrombocytopenia can be summarized as follows:
- Decreased platelet production due to bone marrow disorders
- Increased platelet destruction, often due to immune system disorders like ITP
- Medication-induced effects, where certain drugs lead to thrombocytopenia
Immune Thrombocytopenia (ITP): A Major Cause
Immune thrombocytopenia (ITP) is a condition where the immune system attacks platelets. This leads to a low platelet count. Patients often experience bruising and bleeding.
Pathophysiology of ITP
The immune system mistakenly attacks platelets in ITP. This causes the premature destruction of platelets, mainly in the spleen. The exact triggers are not fully understood, but genetics and environment play a role.
Key aspects of ITP pathophysiology include:
- Autoantibody production against platelet antigens
- Premature platelet destruction in the spleen
- Inadequate platelet production in the bone marrow
Primary vs. Secondary ITP
ITP can be primary or secondary. Primary ITP has no underlying cause. Secondary ITP is linked to diseases, infections, or medications.
Distinguishing between primary and secondary ITP is key for treatment.
Recovery Rates and Prognosis
Recovery from ITP varies. Studies show 37.4% of patients recover within a year. Recovery depends on age, severity, and treatment response.
“The management of ITP requires a thorough approach, considering the patient’s health and condition specifics.”
Knowing recovery rates helps manage patient expectations and guide treatment.
Correlation Between Platelet Count and Bleeding Risk
It’s important to know how platelet count affects bleeding risk. A lower platelet count means a higher chance of bleeding problems.
Studies show that platelets that react more can help prevent bleeding. This shows how platelet count and function work together to affect bleeding risk. We’ll look closer at this, focusing on key levels that show bleeding risk and what can change this risk.
Critical Thresholds for Bleeding Risk
Knowing when bleeding risk goes up is key in managing low platelet counts. While everyone is different, some levels are more important than others.
The 30,000/mm ³ Threshold
A platelet count of 30,000/mm ³ is a key level where bleeding risk goes up a lot. People with counts below this are at higher risk. They might need more careful management to lower this risk.
Factors That Modify Bleeding Risk
Platelet count is not the only thing that affects bleeding risk. Other things like platelet function, other bleeding disorders, and anticoagulant use can also play a part.
Knowing these factors helps create a better plan. It’s not just about the platelet count. It’s about the whole risk picture of the patient.
Diagnosing Thrombocytopenia-Related Bruising
To understand bruising in thrombocytopenia, we need a detailed approach. We check the platelet count and other blood tests. This helps us see how severe the condition is and its effect on health.
Complete Blood Count (CBC) Analysis
A Complete Blood Count (CBC) is key for diagnosing thrombocytopenia. It looks at red blood cells, white blood cells, and platelets. This test tells us a lot about the patient’s blood health.
- Platelet count: To see if thrombocytopenia is present.
- Red blood cell count: To check for anemia or other issues.
- White blood cell count: To look at the immune system’s response.
Peripheral Blood Smear
A Peripheral Blood Smear is another tool for diagnosis. It involves looking at blood under a microscope. This test can spot problems with blood cells, like platelets, and shed light on the cause.
- Look at platelet size and shape.
- Check for platelet clumping or sticking together.
- Find any odd cells or inclusions.
Bone Marrow Examination
In some cases, a Bone Marrow Examination is needed. This test takes a bone marrow sample for analysis.
This test can show if thrombocytopenia is due to platelet production issues or another problem.
Treatment Approaches for Thrombocytopenia
Thrombocytopenia treatment varies based on the cause and how severe it is. A good plan must tackle the root cause and the symptoms.
Addressing the Underlying Cause
First, we find and treat the main reason for thrombocytopenia. This might mean changing medications or treating diseases like leukemia.
Medication Adjustment: If a drug is causing the problem, stopping or changing it can help. We watch patients closely to make sure these changes are safe and work well.
Medication Options
There are many medicines to help with thrombocytopenia. These include:
- Corticosteroids: These are often the first choice to boost platelet counts by reducing immune attacks.
- Intravenous Immunoglobulin (IVIG): IVIG can quickly increase platelet counts, which is helpful in severe cases.
- Thrombopoietin Receptor Agonists: Drugs like romiplostim and eltrombopag help make more platelets in the bone marrow.
These medicines are key in managing the condition and avoiding serious problems.
Surgical Interventions
Surgery might be needed in some cases. For example, removing the spleen can help those with immune thrombocytopenia (ITP) who don’t get better with other treatments. The spleen often destroys platelets in ITP.
Managing Bruising and Bleeding Symptoms
Bruising and bleeding are common problems with thrombocytopenia. They need quick and proper handling. It’s tough to deal with these symptoms, but having good ways to manage them is key.
First Aid for Thrombocytopenia-Related Bleeding
Act fast when bleeding happens. Apply gentle pressure to the bleeding site first. Use a clean cloth or gauze for this.
If bleeding is serious or doesn’t stop, get medical help right away. Keep the patient calm and comfy while waiting.
Supportive Care Measures
Supportive care is important for managing symptoms. Stay away from activities that could hurt you, like contact sports. Be careful with sharp objects too.
- Use a soft-bristle toothbrush to avoid gum bleeding
- Don’t take blood-thinning meds like aspirin or NSAIDs without a doctor’s say-so
- Make your space safe by removing things that could cause falls
Wearing protective gear, like helmets or knee pads, can also help prevent injuries.
Special Considerations for High-Risk Populations
Thrombocytopenia poses special challenges for certain groups. At Liv Hospital, we offer top-notch care for international patients. We understand the unique needs of these groups.
Thrombocytopenia in Pregnancy
Pregnant women with thrombocytopenia need close monitoring. Gestational thrombocytopenia usually goes away after pregnancy. But we must check for other causes like immune thrombocytopenia (ITP) or preeclampsia.
We make sure pregnant women get the right care. This helps avoid any problems.
Pediatric Thrombocytopenia
Children with thrombocytopenia might have different reasons than adults. Neonatal thrombocytopenia can be caused by the mother’s health or the baby’s own issues. We focus on the child’s health and growth.
Elderly Patients with Low Platelet Counts
Elderly people often have other health issues and take medicines that affect platelets. Medication-induced thrombocytopenia is a big worry. We check their meds and manage their thrombocytopenia carefully.
Thrombocytopenia in Cancer Patients
Cancer patients face a high risk of thrombocytopenia from chemo, radiation, or cancer in the bone marrow. Chemotherapy-induced thrombocytopenia can limit treatment and raise bleeding risks. We team up with oncologists to manage it well.
By knowing the special needs of these groups, we can give them better care. This improves their health and life quality.
Conclusion
Thrombocytopenia is a condition where you have too few platelets. This makes it easier to bruise and bleed.
Knowing about thrombocytopenia and bruising is important. It helps both patients and doctors. Spotting the signs early can lead to better care and fewer problems.
Diagnosing thrombocytopenia involves several steps. These include blood tests and other exams. Finding the cause is key to treating it.
Treating thrombocytopenia can help prevent bruising and bleeding. This improves life quality. In summary, understanding thrombocytopenia is vital for better health outcomes.
FAQ’s:
What is thrombocytopenia, and how does it relate to bruising?
Thrombocytopenia is when you have too few platelets in your blood. This can cause more bruising and bleeding. It’s because your body can’t make blood clots as well.
What are the normal platelet count ranges, and how is thrombocytopenia diagnosed?
Normal platelet counts are between 150,000 and 450,000 per microliter of blood. Doctors use a complete blood count (CBC) to find out if you have thrombocytopenia.
What are the common symptoms of thrombocytopenia beyond bruising?
Symptoms include small red spots on the skin (petechiae), larger bruises (ecchymosis), and purple patches (purpura). You might also bleed from your gums, nose, or stomach.
How does immune thrombocytopenia (ITP) affect platelet count?
ITP makes your immune system attack and destroy platelets. This lowers your platelet count and raises your risk of bleeding and bruising.
What is the significance of the 30,000/mm ³ platelet count threshold?
A count below 30,000/mm ³ means you’re at high risk for bleeding and bruising. It’s a critical number to watch.
How is thrombocytopenia-related bruising managed?
Doctors treat the cause, use medicines to boost platelet count, and advise avoiding injuries. They also tell you to apply pressure to stop bleeding.
Are there any specific considerations for pregnant women with thrombocytopenia?
Pregnant women need close monitoring because of the risk of bleeding during delivery. It can also affect the baby.
Can medications cause thrombocytopenia?
Yes, some medicines can lower platelet count. They might reduce platelet production or increase their destruction.
What are the treatment options for thrombocytopenia?
Treatment includes addressing the cause, medicines like corticosteroids, and sometimes surgery like splenectomy for severe cases.
How does thrombocytopenia affect cancer patients?
Cancer patients are more likely to get thrombocytopenia from chemotherapy or radiation. It’s important to manage it to avoid bleeding.
What is the role of platelet count in determining bleeding risk?
Platelet count is key in assessing bleeding risk. Lower counts mean a higher risk of bleeding and bruising.
What are petechiae, ecchymosis, and purpura?
Petechiae are small spots, ecchymosis are larger bruises, and purpura are purple patches. All can be signs of thrombocytopenia.
References
Ashworth, I. (2021). Thrombocytopenia: The good, the bad and the ugly. British Journal of Haematology. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9135082/
Jan, M. A., Khalil, S., & Rahman, F. (2004). Thrombocytopenia in children. Journal of Pakistan Medical Institute, 18(4), 369-371. Retrieved from https://jpmi.org.pk/index.php/jpmi/article/view/900