We talk a lot about the need for healthy blood cells. But low platelet count can cause big problems. Thrombocytopenia, or low platelet count, can make clotting too little or bleeding too much.
So, what are platelets? They are blood cells that help stop bleeding by forming clots. If your bone marrow doesn’t make enough, you might face bleeding issues. This could lead to a serious clotting disorder like immune thrombocytopenic purpura (ITP).
Knowing about platelet counts is key to understanding thrombocytopenia’s risks. We’ll look into why keeping platelet levels healthy is important to avoid these problems.
Key Takeaways
- Thrombocytopenia is a condition characterized by low platelet count.
- Low platelet count can lead to bleeding complications.
- Understanding platelet counts is critical for assessing risks.
- Immune thrombocytopenic purpura (ITP) is a possible clotting disorder.
- Keeping platelet levels healthy is vital to avoid issues.
Understanding Platelets and Their Role in Blood Clotting
Platelets are key to how our body stops bleeding after injuries. They are also known as thrombocytes. Their job is to clump and clot blood vessel injuries to prevent bleeding.
What Are Platelets and Normal Platelet Counts
Platelets are tiny blood cells made in the bone marrow. They are vital for blood clotting. This process stops bleeding when a blood vessel is hurt. A normal count is between 150,000 and 450,000 platelets per microliter (μL) of blood.
Normal Platelet Count: 150,000 – 450,000/μL
| Platelet Count (/μL) | Status |
|---|---|
| Below 150,000 | Low Platelet Count (Thrombocytopenia) |
| 150,000 – 450,000 | Normal |
| Above 450,000 | High Platelet Count (Thrombocytosis) |
How Platelets Function in Hemostasis
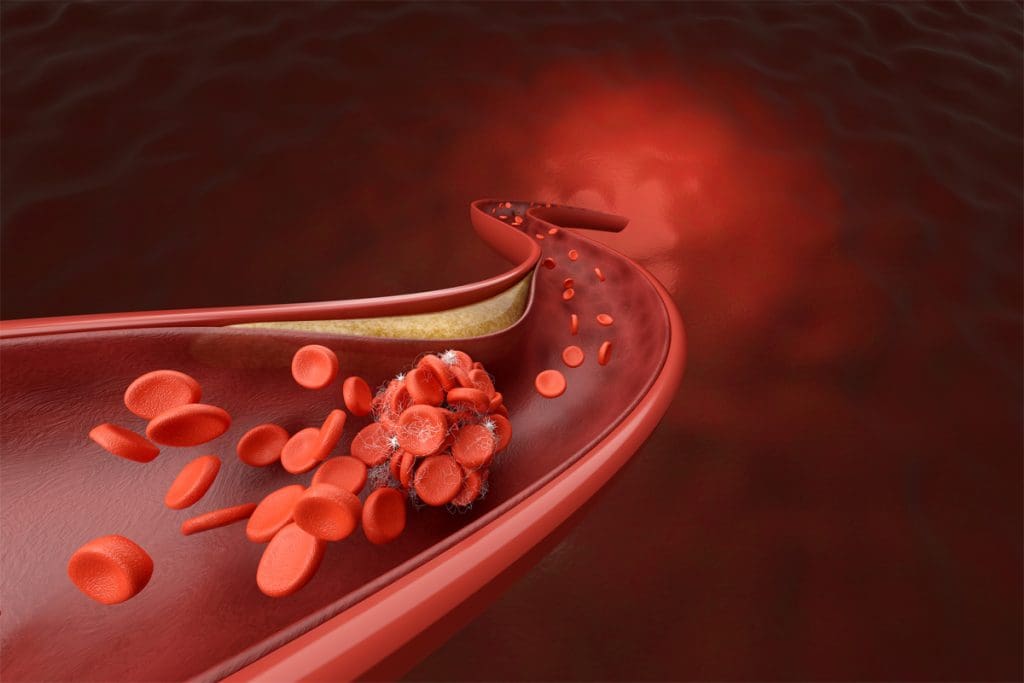
Platelets are essential in stopping bleeding after an injury. When a blood vessel is damaged, platelets stick to the injury. They clump together to form a plug.
This plug is then strengthened by fibrin, a protein that creates a mesh. This mesh forms a blood clot that seals the injured vessel.
The work of platelets is complex, involving adhesion, activation, and aggregation. Knowing how platelets function is important for diagnosing and treating conditions like thrombocytopenia.
What is Thrombocytopenia?
Thrombocytopenia is a condition where there are not enough platelets in the blood. Platelets help blood to clot. Without enough, bleeding can become a problem.
Definition and Diagnosis of Thrombocytopenia
Thrombocytopenia happens when there are less than 150,000 platelets per microliter of blood. A PLT blood test is used to check for this. It’s key for finding and understanding the severity of the condition.
The ICD-10 classification is used to code thrombocytopenia in medical records. Knowing how to diagnose and classify it is important for treatment.
Classification Based on Platelet Count
Thrombocytopenia is divided into levels based on platelet count. Mild cases might not show symptoms, but severe cases can be dangerous. The level helps decide how to treat it.
- Mild Thrombocytopenia: Platelet count between 100,000 and 150,000 per microliter.
- Moderate Thrombocytopenia: Platelet count between 50,000 and 100,000 per microliter.
- Severe Thrombocytopenia: Platelet count below 50,000 per microliter.
PLT Blood Test and Diagnosis
A PLT blood test is the main way to diagnose thrombocytopenia. It counts the platelets. Other tests might be needed to find why the platelet count is low.
Knowing the causes and types of thrombocytopenia is key to managing it. We’ll look at causes and treatments next.
Immune Thrombocytopenic Purpura (ITP): The Primary Clotting Disorder
Immune Thrombocytopenic Purpura (ITP) is a clotting disorder that affects millions. It’s caused by a low platelet count due to the immune system attacking platelets. We’ll look at how common it is, why it happens, and how it’s diagnosed and treated.
Prevalence and Pathophysiology
ITP is an autoimmune disease found in about 9.5 per 100,000 adults. It happens when the immune system makes antibodies against platelets, marking them for destruction. This mainly happens in the spleen, causing a low platelet count.
A study on NCBI shows the immune system’s role in ITP. Knowing how it works helps in managing the disease.
Primary vs. Secondary ITP
ITP can be either primary or secondary. Primary ITP doesn’t have other conditions, while secondary ITP does. Knowing the type helps choose the right treatment.
| Characteristics | Primary ITP | Secondary ITP |
|---|---|---|
| Underlying Conditions | None | Present (e.g., infections, autoimmune diseases) |
| Autoantibody Production | Yes | Yes, often triggered by underlying condition |
| Treatment Approach | Focuses on increasing platelet count | Addresses underlying condition and ITP |
ICD-10 Classification for Thrombocytopenia
The ICD-10 system has specific codes for thrombocytopenia and ITP. The code for ITP is D69.3. Accurate coding is key for tracking and billing.
“The ICD-10 classification is vital for diagnosing and managing thrombocytopenia. It helps healthcare providers track and treat it well.”
” Clinical Guidelines
Understanding ITP and its types is important for healthcare providers. It helps them create effective treatment plans. We’ll look at other clotting disorders related to thrombocytopenia next.
Other Clotting Disorders Associated with Thrombocytopenia
Thrombocytopenia can cause several clotting disorders. These include TTP, HIT, DIC, and HELLP syndrome. It’s important to understand these conditions to provide the best care for patients.
Thrombotic Thrombocytopenic Purpura (TTP)
TTP is a rare blood disorder. It causes blood clots in small blood vessels. This leads to thrombocytopenia and microangiopathic hemolytic anemia.
Symptoms of TTP include purpura, neurological issues, and kidney failure.
Heparin-Induced Thrombocytopenia (HIT)
HIT is an immune reaction to heparin. It leads to thrombocytopenia and can cause severe blood clots.
Disseminated Intravascular Coagulation (DIC)
DIC is a condition with widespread clotting and bleeding. It can be caused by sepsis, trauma, or cancer. This leads to thrombocytopenia and the use up of clotting factors.
HELLP Syndrome
HELLP syndrome is a serious condition in pregnancy. It includes hemolysis, high liver enzymes, and low platelet count (thrombocytopenia). It’s a variant of preeclampsia and can harm both mother and baby.
| Condition | Key Characteristics | Associated Risks |
|---|---|---|
| TTP | Microangiopathic hemolytic anemia, thrombocytopenia | Neurological symptoms, renal failure |
| HIT | Immune-mediated thrombocytopenia, thrombosis | Severe thrombotic complications |
| DIC | Widespread clotting and bleeding, thrombocytopenia | Organ failure, severe bleeding |
| HELLP Syndrome | Hemolysis, elevated liver enzymes, thrombocytopenia | Maternal and fetal morbidity |
Common Causes of Low Platelet Count
It’s important to know why people have low platelet counts. This helps doctors find the right treatment. We’ll look at the main reasons for low platelet counts to help you understand better.
Immune-Mediated Causes
Some cases of low platelet count happen when the immune system goes wrong. Immune thrombocytopenic purpura (ITP) is when the body makes antibodies against platelets. This can happen for many reasons, like other autoimmune diseases or infections.
Medication-Induced Thrombocytopenia
Some medicines can lower platelet counts as a side effect. This includes heparin, antibiotics like linezolid, and some anticonvulsants. Heparin-induced thrombocytopenia (HIT) is very serious and can cause blood clots. It happens when the body makes antibodies against heparin and platelets.
Infection-Related Thrombocytopenia
Infections can also lower platelet counts. This can happen when viruses like HIV or hepatitis C infect the bone marrow. Or, it can be because of the immune system attacking platelets.
Bone Marrow Disorders
Bone marrow problems can also cause low platelet counts. Conditions like leukemia, lymphoma, and aplastic anemia can harm the bone marrow. This makes it hard to make platelets. Myelodysplastic syndromes, which affect how blood cells are made, can also cause this problem.
Knowing the causes helps doctors find the best way to treat low platelet counts.
Treatment Options to Increase Platelet Count
To tackle low platelet counts, several treatments are available. These range from medical options to making lifestyle changes. The right treatment depends on the cause of low platelets, how severe it is, and the person’s health.
Medical Interventions
Medical treatments are often the first step for low platelets. These include:
- Corticosteroids to reduce platelet destruction
- Immunoglobulins to temporarily increase platelet count
- Thrombopoietin receptor agonists to stimulate platelet production
These treatments aim to either stop platelet destruction or boost new platelet production.
Surgical Approaches
In some cases, surgery is needed. The most common surgery is:
- Splenectomy, which involves removing the spleen, a common site of platelet destruction
This surgery is for those with severe low platelets who don’t get better with medicine.
Natural Remedies and Dietary Approaches
Along with medical and surgical treatments, natural remedies and diet changes can help. These include:
- Eating foods rich in vitamin B12 and folate, key for platelet making
- Avoiding foods that can harm platelet function or making
- Drinking plenty of water to keep overall health up
| Treatment Option | Description | Benefit |
|---|---|---|
| Corticosteroids | Reduce platelet destruction | Increase platelet count |
| Immunoglobulins | Temporarily increase platelet count | Rapid improvement in platelet count |
| Thrombopoietin receptor agonists | Stimulate platelet production | Long-term increase in platelet count |
| Splenectomy | Remove the spleen to reduce platelet destruction | Permanent reduction in platelet destruction |
By using these treatments together, people with low platelets can manage their condition better. This improves their quality of life.
Conclusion: Living with Thrombocytopenia-Related Clotting Disorders
We’ve looked into the complex world of thrombocytopenia and its link to clotting disorders. It’s key to know about platelet count and how it affects health. With the right care, people with thrombocytopenia can live healthy lives.
Managing thrombocytopenia means keeping an eye on platelet count and following treatment plans. Making lifestyle changes is also important. Knowing about the condition helps people take care of their health and avoid problems.
Handling thrombocytopenia well needs a mix of medical care, lifestyle changes, and learning about the condition. It’s vital to work with doctors to create a treatment plan that fits each person’s needs.
By being active and informed in managing thrombocytopenia, people can live better and avoid serious issues. We’re dedicated to top-notch healthcare and support for patients from around the world.
FAQ
What is thrombocytopenia?
Thrombocytopenia is when you have too few platelets in your blood. This can cause bleeding problems. Doctors use a PLT blood test to find out if you have it. They then figure out how bad it is based on your platelet count.
What are the normal platelet counts?
Normal platelet counts are between 150,000 and 450,000 per microliter of blood. If your count is lower, you might have thrombocytopenia.
What is the role of platelets in blood clotting?
Platelets are key in stopping bleeding. They form clots when a blood vessel gets hurt. This helps stop the bleeding.
What is Immune Thrombocytopenic Purpura (ITP)?
ITP is an autoimmune disease. It makes your immune system attack your platelets. This leads to a low platelet count. It’s a main cause of thrombocytopenia.
What are the common causes of low platelet count?
Low platelet counts can come from many places. This includes autoimmune diseases, medicines, infections, and problems with the bone marrow.
How is thrombocytopenia diagnosed?
Doctors use a PLT blood test to find thrombocytopenia. They then figure out how severe it is based on your platelet count.
What are the treatment options for thrombocytopenia?
There are many ways to treat thrombocytopenia. This includes medicine, surgery, and natural remedies. Eating the right foods can also help manage it.
What is the ICD-10 classification for thrombocytopenia?
The ICD-10 is a code for medical billing. It helps classify thrombocytopenia. This makes it easier for insurance and medical records.
Can thrombocytopenia be associated with other clotting disorders?
Yes, thrombocytopenia can link to other clotting problems. This includes TTP, HIT, DIC, and HELLP syndrome.
How can I increase my platelet count?
To boost your platelet count, you can try medicine or eat foods that help. Foods rich in nutrients can support platelet production.
References
- MedlinePlus. (2024). Immune thrombocytopenic purpura (ITP). U.S. National Library of Medicine. https://medlineplus.gov/ency/article/000535.htm