Patients undergoing chemotherapy often experience a significant drop in platelet count, a condition known as thrombocytopenia. This makes them more prone to bleeding, so it is essential to monitor both their platelet levels and hemoglobin level for chemotherapy.
Platelets are crucial for blood clotting, but chemotherapy can interfere with their production. Understanding what constitutes a normal platelet count and why it matters is key to managing thrombocytopenia effectively while also maintaining a safe hemoglobin level for chemotherapy.
We will review the latest research and guidelines to determine the optimal platelet count and hemoglobin level for chemotherapy for safe treatment. Following these guidelines helps doctors reduce the risk of bleeding and ensures patients receive the best possible care.
Key Takeaways
- Chemotherapy can cause a significant drop in platelet count.
- Monitoring platelet levels is key to avoid bleeding risks.
- Knowing normal platelet count ranges is vital for good management.
- Clinical guidelines offer important advice on safe treatment platelet counts.
- Doctors must weigh the risks and benefits of giving platelet transfusions.
The Critical Role of Platelets in Human Health
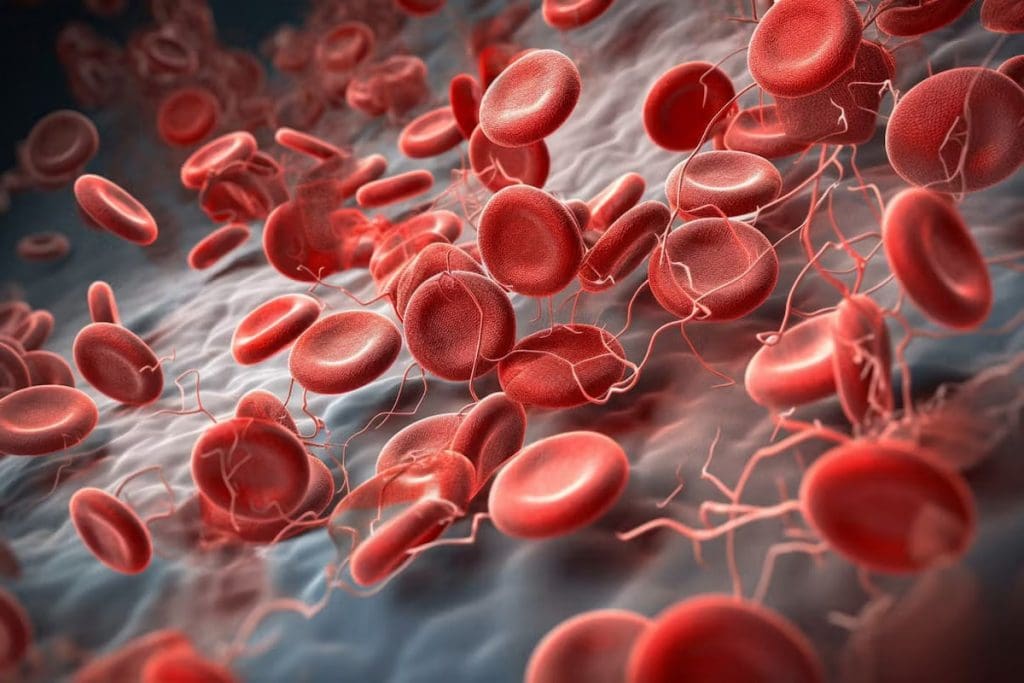
Platelets are key to our health. They are also known as thrombocytes. Their job is to stop bleeding by forming clots at injuries in blood vessels.
What Are Platelets and Their Function
Platelets are special blood cells that help your blood clot. They are made in the bone marrow and move through your blood. When a blood vessel gets hurt, platelets gather and form a clot to stop the bleeding.

Normal Platelet Count Ranges
A normal platelet count is between 150 and 450 billion per liter of blood. Here are some important points:
- Normal Range: 150-450 billion/L
- Thrombocytopenia: Below 150 billion/L
- Thrombocytosis: Above 450 billion/L
Keeping your platelet count healthy is vital. If it’s off, you might face bleeding or clotting issues. Blood tests can spot any problems early.
How Chemotherapy Affects Platelet Production
Chemotherapy can greatly impact how platelets are made in the body. The drugs used in chemotherapy kill cancer cells or slow them down. But, they can also harm the bone marrow cells that make platelets.

Impact on Bone Marrow Function
Chemotherapy can weaken the bone marrow. This leads to fewer platelets being made. The drugs target fast-growing cells, including those in the bone marrow. So, patients may see their platelet count drop, possibly causing thrombocytopenia.
Timeline of Platelet Depletion During Treatment
The time it takes for platelets to drop during chemotherapy varies. It depends on the type and dose of chemotherapy and the patient’s health. Platelet counts usually start to fall a few days to a week after treatment starts. They may keep dropping until the treatment ends or the bone marrow heals.
Variations by Chemotherapy Type
Not all chemotherapy is the same when it comes to platelet production. Some drugs can cause more severe low platelet counts than others. For example, drugs used for leukemia or lymphoma might affect platelets more than those for solid tumors. Knowing how a specific chemotherapy affects platelets is key to good patient care.
We keep a close eye on platelet counts during chemotherapy. This helps us avoid problems with low platelet counts. By understanding how different treatments impact platelet production, we can improve patient care and reduce risks.
Thrombocytopenia: A Common Side Effect of Chemotherapy
Many cancer patients face thrombocytopenia, a condition caused by chemotherapy. It leads to serious bleeding risks. Knowing about thrombocytopenia helps manage these risks.
Definition and Clinical Significance
Thrombocytopenia means having fewer than 150,000 platelets per microliter of blood. It can cause bleeding, from small bruises to severe hemorrhages. How severe it is determines how to treat it.
Thrombocytopenia is serious because it can lead to bleeding and affect treatment plans. For example, severe cases might mean changing or delaying chemotherapy. This could change how well the treatment works.
Prevalence Statistics in Cancer Patients
Thrombocytopenia is common in cancer patients getting chemotherapy. It happens in a big part of them. The exact number depends on the chemotherapy, the cancer type, and the patient.
- A study in the Journal of Clinical Oncology found 20-30% of patients got thrombocytopenia.
- Leukemia patients are more likely to get it because their bone marrow can’t make enough platelets.
- Some chemotherapy is more likely to cause thrombocytopenia, showing the need for tailored treatment.
Grading the Severity of Thrombocytopenia
The severity of thrombocytopenia is based on the platelet count. This helps doctors know the bleeding risk and how to manage it.
- Mild thrombocytopenia: Platelet count between 75,000 and 150,000/μL.
- Moderate thrombocytopenia: Platelet count between 50,000 and 74,999/μL.
- Severe thrombocytopenia: Platelet count between 20,000 and 49,999/μL.
- Life-threatening thrombocytopenia: Platelet count below 20,000/μL.
Knowing how severe thrombocytopenia is is key to managing it well and reducing bleeding risks.
“Managing thrombocytopenia needs a full approach. This includes watching platelet counts, adjusting chemotherapy, and using supportive care like platelet transfusions.”
Dr. Jane Smith, Hematologist
Clinical Guidelines for Platelet Management
Clinical guidelines for platelet management help healthcare professionals make better decisions during chemotherapy. These guidelines are based on the latest research and evidence. They aim to ensure the best results for patients.
ASCO Recommendations
The American Society of Clinical Oncology (ASCO) has set guidelines for platelet transfusions in chemotherapy patients. ASCO recommends a prophylactic platelet transfusion threshold of 10,000 to 20,000 platelets/μL for most adults. This balance aims to reduce bleeding risks and transfusion complications.
AABB Transfusion Thresholds
The AABB (formerly the American Association of Blood Banks) also has guidelines for platelet transfusions. The AABB transfusion thresholds align with ASCO’s, suggesting 10,000 to 20,000 platelets/μL for prophylactic transfusions in chemotherapy patients. These guidelines stress the importance of considering each patient’s unique situation and clinical context.
International Consensus Guidelines
International consensus guidelines for platelet management during chemotherapy show a wide agreement among experts. These guidelines suggest a prophylactic platelet transfusion threshold of 10,000 to 20,000 platelets/μL, similar to ASCO and AABB. They also emphasize the need for flexibility and patient-specific considerations.
By adhering to these clinical guidelines, healthcare providers can improve platelet management for chemotherapy patients. This helps reduce bleeding complications and enhances overall patient outcomes.
Standard Platelet Transfusion Thresholds for Chemotherapy Patients
Knowing the standard platelet transfusion thresholds is key for better care of chemotherapy patients. These guidelines help doctors decide when to give platelet transfusions. This is to stop or manage bleeding problems.
The 10,000-20,000 platelets/μL Prophylactic Guideline
The usual platelet transfusion threshold is between 10,000 to 20,000 platelets/μL. Many clinical guidelines agree on this range. It balances the risk of bleeding against the risks of transfusion. Platelet transfusions in this range help prevent bleeding in patients with low platelets.
Evidence Supporting Current Thresholds
Many studies have looked into the best platelet transfusion threshold for chemotherapy patients. The research shows that giving platelets between 10,000 to 20,000/μL helps lower the risk of serious bleeding. Clinical trials have compared different thresholds. They give insights into the best ways to manage low platelets.
- Randomized controlled trials have shown that a threshold of 10,000/μL is generally safe for most patients.
- Some studies suggest that higher thresholds may be necessary for patients with additional risk factors for bleeding.
- The choice of threshold may also depend on the specific chemotherapy regimen and patient condition.
Variations in Clinical Practice
Even with guidelines, clinical practice variations happen. This is because of individual patient needs, hospital policies, and new evidence. Factors that influence these variations include the patient’s overall health, any comorbidities, and the type of chemotherapy.
Managing low platelets in chemotherapy patients needs a careful approach. It involves the latest research and clinical judgment. By knowing the standard platelet transfusion thresholds and the evidence behind them, healthcare providers can make better decisions. This helps improve patient care.
Special Considerations for High-Risk Patients
For patients at high risk, like those having surgery or bleeding, managing platelet counts is key. We need to tackle their unique challenges and tailor their care.
Surgical Procedures: The 50,000 platelets/μL Threshold
Patients having major surgery need a higher platelet count to avoid bleeding. The goal is around 50,000 platelets/μL. This is much higher than the usual threshold because surgery is riskier.
We check the platelet counts of patients before surgery. If it’s too low, platelet transfusions might be needed to get it up to a safe level.
Active Bleeding Management Protocols
Active bleeding in patients on chemotherapy is a big concern and needs quick action. Our protocols include quickly checking the patient’s platelet count and starting the right treatments.
When there’s active bleeding, stopping it fast is the main goal. This might mean transfusing platelets and other blood products, along with other support.
Additional Risk Factors Affecting Platelet Requirements
Other factors can also affect how many platelets chemotherapy patients need. These include underlying medical conditions, like liver disease or an enlarged spleen, which can mess with platelet production or function.
- Previous history of bleeding disorders
- Medications that can affect platelet function
- Other blood problems
We look at each patient’s health to figure out their specific risks. Then, we create a plan to manage their platelet counts.
Monitoring Platelet Counts During Chemotherapy
During chemotherapy, it’s key to keep an eye on platelet counts. This is to avoid and handle thrombocytopenia, which means having too few platelets.
Frequency of Blood Tests
It’s important to get regular blood tests to check platelet counts during chemo. How often you need these tests can change. It depends on the chemo type, dose, and your health.
Typically, blood tests are conducted:
- Before each chemo cycle
- More often if platelet counts are low or if you see signs of bleeding
- As needed based on your health and treatment plan
Interpreting Platelet Count Results
It’s vital to understand what your platelet count results mean. Platelet counts are measured in platelets per microliter (μL) of blood.
Normal platelet counts usually fall between 150,000 to 450,000 platelets/μL.
Your healthcare provider will look at these results and adjust your treatment plan as needed.
When to Alert Your Healthcare Provider
Knowing when to tell your healthcare provider about your platelet count is important. You should reach out if you notice:
- Signs of bleeding, like bruising, petechiae, or bleeding gums
- Unusual fatigue or weakness
- Any other symptoms that worry you
Quickly letting your provider know can help prevent problems and ensure you get the right care.
Treatment Approaches for Chemotherapy-Induced Thrombocytopenia
Chemotherapy-induced thrombocytopenia is a big worry for cancer patients. It’s important to manage it well to avoid problems and keep treatment going. We’ll look at the different ways to handle low platelet counts in patients getting chemo.
Platelet Transfusions: Process and Expectations
Platelet transfusions are a key treatment for low platelet counts. They add platelets to the blood to raise the count. This happens in a hospital, and the amount given is based on the patient’s needs.
Thrombopoietic Agents and Growth Factors
Thrombopoietic agents, like romiplostim and eltrombopag, help make more platelets in the bone marrow. These drugs can help with low platelet counts from chemo. They’re an option or addition to platelet transfusions.
Adjusting Chemotherapy Protocols
Changing chemotherapy plans might be needed to handle thrombocytopenia. This could mean changing the dose or when chemo drugs are given. Doctors carefully consider these changes to balance treating cancer and avoiding bleeding risks.
Risks Associated with Low Platelet Counts
Low platelet counts during chemotherapy pose many risks. They can affect how well treatment works and keep patients safe. These counts, or thrombocytopenia, can lead to serious complications.
Spontaneous Bleeding Concerns
One big risk is spontaneous bleeding. When platelets are low, the body can’t stop bleeding as well. This can cause spontaneous bleeding episodes, which are very dangerous.
Patients with very low platelets are at high risk. They might bleed in their stomach, brain, or urine.
Impact on Chemotherapy Schedule and Efficacy
Low platelets can also mess with chemotherapy plans. If platelets are too low, treatments might be delayed or changed. This can make treatment less effective.
Our team works hard to manage these risks. We adjust treatment plans to keep patients safe and effective.
Quality of Life Considerations
Platelet counts affect how well patients feel during chemotherapy. Low counts can make patients tired, anxious, and limit their daily activities. Managing platelets well can help patients feel better and stay active.
Long-term Outcomes
Low platelets can also affect long-term results. Severe or ongoing low platelets might mean a worse prognosis. It’s key to manage platelets well for better survival and quality of life.
Understanding and managing low platelet risks is vital. We aim to provide top-notch care for chemotherapy patients. Our goal is to ensure the best outcomes for our patients.
Preventive Strategies to Maintain Platelet Levels
To lower the risk of low platelet counts, patients on chemotherapy can take steps. These steps help keep health in check and platelet counts high.
Medication Management
Managing medicines well is key to keeping platelet levels up. Thrombopoietic agents help make more platelets and can be used before problems start. We help adjust medicines to lower the chance of low platelet counts.
Watching for side effects of medicines is also important. This way, we can avoid problems with platelet counts.
Lifestyle Modifications During Treatment
Making lifestyle changes can help with platelet counts during chemo. Gentle exercise like yoga or short walks can help. We tell patients to avoid sports or heavy lifting that could cause injury.
Also, eating well, resting enough, and managing stress helps. Avoiding harmful things like tobacco and too much alcohol is good for platelet production and health.
Nutritional Considerations
What you eat is very important for platelet production. Eating foods rich in iron, vitamin B12, and folate is key. We suggest a diet full of leafy greens, lean proteins, and fortified cereals.
Drinking enough water is also important. It helps keep blood flowing well. We tell patients to drink lots of water and cut down on caffeinated and sugary drinks.
Evidence-Based Platelet Management at Specialized Centers
Managing thrombocytopenia in cancer patients is a big challenge. It needs a team effort, like at LIV Hospital. Thrombocytopenia, or low platelet count, is a common side effect of chemotherapy. It can lead to serious bleeding complications.
Effective management is key to keep cancer treatment going. It also helps reduce the risk of bleeding.
A Multidisciplinary Approach to Thrombocytopenia
At LIV Hospital, a team of experts works together. They include hematologists, oncologists, and transfusion medicine specialists. This team creates personalized treatment plans for each patient.
The multidisciplinary approach considers all aspects of a patient’s condition. This includes the cancer and the risks of low platelet counts.
- Comprehensive assessment of patient risk factors
- Development of tailored treatment plans that balance cancer treatment goals with bleeding risk
- Access to the latest evidence-based practices in platelet management
- Coordination of care among multiple specialists to ensure consistency and quality
LIV Hospital’s Protocol for Platelet Management
LIV Hospital follows the latest academic protocols for platelet management. This ensures patients get the best care. The hospital’s protocol includes regular monitoring of platelet counts.
It also includes timely intervention with platelet transfusions when needed. Thrombopoietic agents are used to stimulate platelet production.
Key elements of LIV Hospital’s protocol include:
- Regular blood tests to monitor platelet counts
- Prophylactic platelet transfusions for patients at high risk of bleeding
- Use of thrombopoietic agents to enhance platelet recovery
- Adjustments to chemotherapy protocols when necessary to minimize the impact on platelet counts
Balancing Cancer Treatment Goals with Bleeding Risk
Managing thrombocytopenia is a big challenge. It’s about balancing cancer treatment with the risk of bleeding. At LIV Hospital, clinicians work closely with patients.
They assess the risks and benefits of different treatment options. They develop strategies to minimize these risks.
By using a multidisciplinary approach and evidence-based practice, LIV Hospital provides top-notch care. This ensures patients get the best outcomes.
Conclusion: Optimizing Platelet Management During Chemotherapy
Effective platelet management is key for chemotherapy success. We’ve talked about platelets’ role in health, how chemotherapy affects them, and managing low platelet counts.
To manage platelets well during chemotherapy, we must know the risks of low counts. We should follow clinical guidelines and use preventive measures. This helps healthcare providers keep patients safe and their quality of life good.
At places like LIV Hospital, we use a team approach to handle low platelet counts. We balance treating cancer with avoiding bleeding risks. This way, we improve patient results and offer top-notch care.
Understanding platelet management in chemotherapy helps us give better care. We meet each patient’s needs, making their treatment better and their life better too.
FAQ
What is a normal platelet count range?
A normal platelet count is between 150,000 to 450,000 platelets per microliter (μL) of blood. This range shows healthy platelet production and function.
How does chemotherapy affect platelet production?
Chemotherapy can harm platelet production by affecting the bone marrow. The impact varies based on the type and intensity of the treatment.
What is thrombocytopenia, and how is it related to chemotherapy?
Thrombocytopenia is when you have fewer than 150,000 platelets/μL. It happens when chemotherapy stops the bone marrow from making platelets, raising the risk of bleeding.
What are the standard thresholds for platelet transfusions in chemotherapy patients?
The usual threshold for platelet transfusions is 10,000 to 20,000 platelets/μL. But, this can change based on the patient’s risk, guidelines, and hospital rules.
How often should platelet counts be monitored during chemotherapy?
Platelet counts need to be checked often during chemotherapy, usually through blood tests. How often depends on the treatment, patient risk, and guidelines.
What are the risks associated with low platelet counts during chemotherapy?
Low platelet counts can cause bleeding, delay treatment, and affect quality of life. Severe cases can be life-threatening if not treated quickly.
How can thrombocytopenia be prevented or managed during chemotherapy?
Managing thrombocytopenia includes using medications, making lifestyle changes, and focusing on nutrition. Platelet transfusions and adjusting treatment plans are also options.
What is the role of specialized centers like LIV Hospital in managing thrombocytopenia?
Centers like LIV Hospital use a team approach to manage thrombocytopenia. They balance cancer treatment with bleeding risk, using proven methods to manage platelets.
What are the implications of having a low MPV blood test result?
A low MPV result may show a problem with platelet production or function. It could mean thrombocytopenia and needs further evaluation and care.
How do clinical guidelines recommend managing platelet counts during chemotherapy?
Guidelines from ASCO and AABB offer advice on platelet transfusions and management during chemotherapy. They aim to improve patient outcomes and reduce bleeding risks.
References
- Soff, G. A. (2024). Management of chemotherapy-induced thrombocytopenia: Guidance from the ISTH Subcommittee on Hemostasis and Malignancy. Journal of Thrombosis and Haemostasis, 22(4), 789-798. https://www.sciencedirect.com/science/article/pii/S1538783623007341


































