Thrombocytopenia is a condition where you have a low platelet count. This can cause serious bleeding problems. A platelet count under 10,000/μL is very dangerous. It can lead to life-threatening bleeding, making it a medical emergency. When is thrombocytopenia an emergency? Learn the thrombocytopenia emergency criteria and the dangerous low platelet counts that require immediate, powerful care.
It’s important to know when thrombocytopenia is an emergency. At places like LivHospital, doctors are ready to spot these dangers. They know the key signs that mean you need help right away.
Key Takeaways
- Thrombocytopenia is a condition characterized by a low blood platelet count.
- A platelet count below 10,000/μL is considered a medical emergency due to the high risk of spontaneous bleeding.
Understanding the critical criteria for thrombocytopenia emergencies is important for both patients and healthcare providers.
- Quick medical help is key to avoiding serious problems.
- Top healthcare places are essential for treating thrombocytopenia patients.
Understanding Thrombocytopenia and Its Significance
Thrombocytopenia, or low platelet count, makes it hard for the body to form blood clots. This can lead to bleeding problems. It’s important for doctors and patients to understand thrombocytopenia to manage and treat it well.
Definition and Normal Platelet Ranges
Thrombocytopenia means having fewer platelets than usual. Platelets should be between 150,000 and 450,000 per microliter of blood. They help the blood clot, and not enough can cause bleeding.
Classification of Thrombocytopenia Severity
The severity of thrombocytopenia depends on the platelet count:
- Mild: 100,000 to 150,000 platelets/μL
- Moderate: 50,000 to 100,000 platelets/μL
- Severe: Below 50,000 platelets/μL
- Very Severe: Below 20,000 platelets/μL
Each level shows a different risk for bleeding.
Impact of Low Platelets on Hemostasis
Hemostasis is how the body stops bleeding. Platelets are key in this process by forming clots. Low platelet counts make it hard to stop bleeding. This can cause easy bruising, nosebleeds, and even life-threatening bleeding.
Common Causes of Thrombocytopenia
Thrombocytopenia, or low platelet count, has many causes. It can happen when platelet production, destruction, or distribution is affected.
Decreased Platelet Production
One main cause of thrombocytopenia is when the body makes fewer platelets. This can happen in aplastic anemia, where the bone marrow doesn’t make enough blood cells. Other conditions, like leukemia or myelodysplastic syndrome, can also lower platelet production.
Increased Platelet Destruction
Increased platelet destruction is another big reason for thrombocytopenia. This can be due to the immune system attacking platelets, as in immune thrombocytopenia (ITP). Other causes include thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS), where blood clots use up platelets.
Sequestration of Platelets
Sequestration of platelets means platelets get stuck in organs, like the spleen. This can happen in hypersplenism, often linked to liver disease or splenomegaly. It leads to fewer platelets in the blood.
Drug-Induced Thrombocytopenia
Some medicines can cause thrombocytopenia. This can happen through immune attacks or by stopping platelet production. Drugs like heparin, vancomycin, and anti-inflammatory drugs are common culprits. Drug-induced thrombocytopenia is serious because these drugs are widely used.
Knowing the causes of thrombocytopenia is key to treating it well. By finding out why platelets are low, doctors can give the right treatment.
Clinical Manifestations of Low Platelet Counts
Low platelet counts, or thrombocytopenia, can cause a range of symptoms. These can range from mild bruising to severe bleeding. The severity of symptoms depends on how low the platelet count is.
Mild to Moderate Thrombocytopenia Symptoms
People with mild to moderate thrombocytopenia might see small spots on their skin. These spots, called petechiae, are from tiny hemorrhages. They might also bruise easily or have ecchymosis, which are bigger bruises.
These symptoms happen because the body can’t make blood clots well. This makes it hard to stop bleeding in the skin.
Severe Thrombocytopenia Presentations
Severe thrombocytopenia can cause serious bleeding. Patients might have gingival bleeding, epistaxis (nosebleeds), or menorrhagia (heavy menstrual bleeding). In the worst cases, there could be gastrointestinal bleeding or intracranial hemorrhage.
Recognizing Life-Threatening Bleeding Signs
It’s important to know the signs of serious bleeding in thrombocytopenia. Symptoms like severe headache, confusion, or weakness on one side of the body could mean an intracranial hemorrhage. Also, hematemesis (vomiting blood) or melena (black, tarry stools) could mean bleeding in the gut.
Quick medical help is key in these situations.
Thrombocytopenia Emergency Criteria: When to Act Immediately
In severe cases of thrombocytopenia, we need to act fast. It’s important to know when to rush to the hospital. This ensures we give the right care quickly.
Critical Platelet Count Below 10,000/μL
A platelet count under 10,000/μL is a big warning sign. At this level, the risk of bleeding is very high. Prompt platelet transfusion might be needed to save lives.
High-Risk Bleeding Manifestations
Some bleeding signs are very serious and need quick action. These include:
- Spontaneous bleeding from multiple sites
- Large or expanding hematomas
- Bleeding into vital organs (e.g., intracranial hemorrhage)
Spotting these signs early is key to avoiding serious problems.
Neurological and Renal Dysfunction Red Flags
Neurological symptoms like confusion or headaches are serious. So are signs of kidney problems. Prompt evaluation is vital to catch and treat these issues fast.
Evidence of Hemolysis as a Warning Sign
Jaundice or dark urine can signal serious issues like TTP or HUS. These need quick medical help to avoid serious harm.
Knowing when to act fast in thrombocytopenia cases is critical. It helps us save lives and improve health outcomes.
Life-Threatening Thrombocytopenic Disorders
Thrombocytopenia can turn into an emergency due to certain critical disorders. These include heparin-induced thrombocytopenia (HIT) and disseminated intravascular coagulation (DIC). Both can cause severe problems if not treated quickly.
Heparin-Induced Thrombocytopenia (HIT)
Heparin-induced thrombocytopenia is a serious condition caused by heparin use. It lowers platelet counts and can lead to severe blood clots. The diagnosis of HIT is based on clinical presentation and laboratory tests, including ELISA for anti-PF4/heparin antibodies. Treatment involves stopping heparin and starting other anticoagulants.
Disseminated Intravascular Coagulation (DIC)
Disseminated intravascular coagulation is a serious condition where blood clots form in small blood vessels. This leads to low platelet counts and the use up of clotting factors. The clinical presentation can vary from asymptomatic to severe bleeding or thrombosis. Treatment includes addressing the cause, supportive care, and sometimes replacing clotting factors and platelets.
Emergency Diagnostic Approach to Severe Thrombocytopenia
Severe thrombocytopenia needs a quick and detailed diagnosis to avoid serious issues. A low platelet count requires immediate evaluation to find the cause and start treatment.
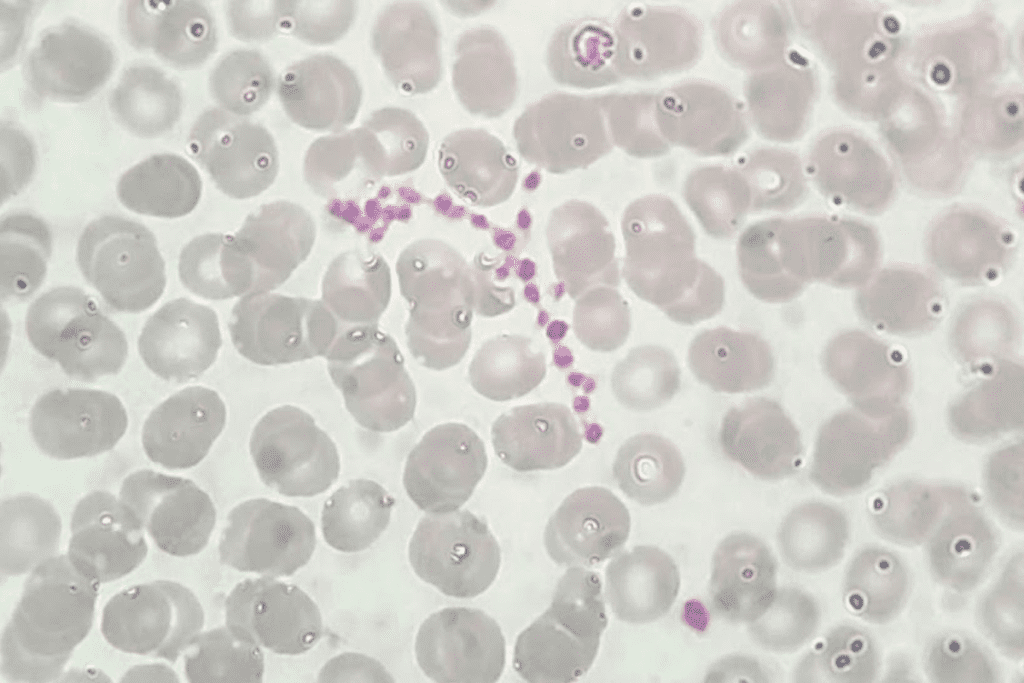
Immediate Laboratory Evaluation
The first step is to run lab tests right away. A complete blood count (CBC) checks the platelet count and other blood cells. A peripheral smear looks for blood cell shape issues, like schistocytes or blasts, to find the cause.
Other tests include blood chemistry tests for liver and kidney health, and coagulation studies for DIC. These help figure out why the platelet count is low and guide treatment.
Imaging Studies in Emergency Settings
In some cases, imaging studies are needed to find the cause of severe thrombocytopenia. Ultrasound can spot a big spleen, which might be holding onto platelets. CT scans can find tumours or infections that might be causing the low platelet count.
Differential Diagnosis in Acute Presentations
There are many possible causes for severe thrombocytopenia, like heparin-induced thrombocytopenia (HIT), disseminated intravascular coagulation (DIC), and thrombotic thrombocytopenic purpura (TTP). A good history and physical exam are key to narrowing down the possible causes.
By using lab and imaging results along with clinical findings, doctors can accurately diagnose and treat severe thrombocytopenia.
Emergency Management of Critical Thrombocytopenia
Managing critical thrombocytopenia is urgent and critical. It’s needed to stop severe bleeding. When platelet counts are very low, the risk of bleeding grows. So, quick and right treatment is key.
Platelet Transfusion Protocols and Thresholds
Platelet transfusions are vital for severe thrombocytopenia. This is true when counts are below 10,000/μL or if there’s active bleeding. The choice to give platelets depends on many things.
These include the cause of low platelets, if there’s bleeding, and the patient’s overall health.
We follow set rules for giving platelets. These rules help ensure the transfusion is safe and effective.
- Platelet concentrates are given to boost platelet counts and lower bleeding risk.
- We watch the platelet counts after transfusion to see if it worked.
- We might use special blood products to lower the chance of bad reactions.
Pharmacological Interventions in Acute Settings
Along with platelet transfusions, we use medicines to treat critical thrombocytopenia. The choice of medicine depends on why the platelets are low.
- Corticosteroids help by reducing platelet destruction or boosting production.
- Intravenous immunoglobulin (IVIG) helps by calming the immune system’s attack on platelets in immune-related cases.
- Thrombopoietin receptor agonists help make more platelets in some cases of low platelets.
We pick the best medicine for each patient based on their specific situation and why their platelets are low.
Special Populations with Unique Thrombocytopenia Risks
Thrombocytopenia can affect anyone, but some groups face special risks. It’s important to understand these differences to give the best care.
Pregnancy-Associated Thrombocytopenia Emergencies
Pregnancy can make diagnosing and managing thrombocytopenia harder. Conditions like gestational thrombocytopenia, preeclampsia, and HELLP syndrome can cause it. These are serious and can be dangerous.
It’s key to watch platelet counts in pregnant women, even more so if they have bleeding disorders. We need to watch for signs of severe thrombocytopenia, like severe bleeding or thrombosis.
Pediatric Thrombocytopenia Crises
Children with thrombocytopenia face unique challenges. Causes can range from autoimmune disorders to bone marrow failure. We must carefully figure out why they have it.
Managing pediatric thrombocytopenia often means supportive care and, in serious cases, platelet transfusions. We also need to think about the emotional impact on kids and their families.
Geriatric Considerations in Acute Thrombocytopenia
Older adults are more likely to have thrombocytopenia due to health issues, medicines, and bone marrow changes. A comprehensive geriatric assessment is vital to find the causes and manage them.
In older patients, managing thrombocytopenia must consider their overall health. This includes their kidney and heart function and how medicines might interact. We also need to watch for bleeding risks.
Immunocompromised Patients
People with weakened immune systems, like those with HIV/AIDS, cancer treatment, or immunosuppressive therapy, are at higher risk. The reason for their weakened immune system affects platelet production or survival.
Managing thrombocytopenia in these patients needs a team effort. This includes infectious disease specialists and hematologists. We must handle the complex relationship between their condition, treatment side effects, and thrombocytopenia.
Prevention and Monitoring After Thrombocytopenia Emergencies
After a thrombocytopenia emergency, patients need careful management to avoid future episodes. We will discuss how to prevent critical thrombocytopenia from happening again. We will also talk about long-term monitoring.
Preventing Recurrence of Critical Thrombocytopenia
To prevent recurrence, we must address the causes of thrombocytopenia. This means changing treatments that lower platelet counts and managing underlying conditions. “Identifying and treating the underlying cause is key to preventing more thrombocytopenia,” say doctors.
- Adjusting medications that may cause thrombocytopenia
- Treating underlying conditions like infections or autoimmune diseases
- Making lifestyle changes to lower bleeding risk
Long-term Monitoring Strategies
Long-term monitoring is vital for patients who have had thrombocytopenia emergencies. Regular check-ups and blood tests track platelet counts. They help adjust treatment plans as needed.
- Regular blood tests to monitor platelet counts
- Follow-up appointments with healthcare providers to check overall health
- Adjusting treatment plans based on the patient’s condition
By using these strategies, we can greatly lower the risk of future thrombocytopenia emergencies. It’s a team effort between healthcare providers and patients for the best results.
Conclusion: Optimizing Outcomes in Thrombocytopenia Emergencies
Managing thrombocytopenia emergencies well needs a full plan. This includes quick action, correct diagnosis, and good treatment. We’ve talked about the key steps in handling these emergencies, like knowing the condition, spotting emergency signs, and using the right management.
A low platelet count can cause serious bleeding. So, starting treatment quickly is key to avoiding bad outcomes. By knowing the emergency signs, doctors can spot at-risk patients early and act fast to help them.
Handling thrombocytopenia emergencies well means working together. This includes using platelet transfusions, medicines, and watching patients closely. With a team effort, we can make sure patients do better and avoid serious problems from low platelet counts.
FAQ
What is thrombocytopenia?
Thrombocytopenia is when you have too few platelets in your blood. Platelets help your blood clot. Having too few can cause bleeding problems.
What is considered a critical platelet count for a thrombocytopenia emergency?
If your platelet count is below 10,000/μL, it’s a big problem. It means you’re at high risk for serious bleeding.
What are the common causes of thrombocytopenia?
There are many reasons for low platelet counts. These include not making enough platelets, losing them too fast, or drugs causing it. Other conditions can also play a part.
What are the symptoms of mild to moderate thrombocytopenia?
Mild to moderate thrombocytopenia might make you bruise easily. You might see small spots on your skin or get nosebleeds. The severity depends on how low your platelet count is.
How is severe thrombocytopenia managed in an emergency setting?
For severe cases, doctors might give you platelet transfusions. They might also use medicines to help. It depends on why you have it, how bad it is, and if you’re bleeding.
What is heparin-induced thrombocytopenia (HIT), and why is it life-threatening?
HIT happens in some people on heparin. It causes a big drop in platelets. This can lead to severe clots, making it very dangerous if not treated right away.
How is disseminated intravascular coagulation (DIC) related to thrombocytopenia?
DIC is when your blood clots too much and bleeds too much. It often happens with low platelet counts because platelets are used up in clots. It needs quick treatment.
What are the special considerations for managing thrombocytopenia in pregnancy?
Pregnancy makes managing thrombocytopenia tricky. Doctors have to think about the mom and the baby. They tailor treatment based on the cause and how bad it is.
How can the recurrence of critical thrombocytopenia be prevented?
To avoid it coming back, find out why it happened. Stay away from drugs that can cause it. Keep an eye out for signs that it might come back.
What is the importance of long-term monitoring after a thrombocytopenia emergency?
Watching your health over time is key. It helps catch problems early. It also helps manage long-term conditions and adjust treatments to keep you safe.
What are the risks associated with low platelet counts in immunocompromised patients?
People with weakened immune systems face more risks. They might bleed more because of low platelets. They need careful watching to avoid serious problems.
How does thrombocytopenia affect hemostasis?
Low platelets mess with your body’s ability to clot blood. Platelets are key to stopping bleeding. Without enough, you’re at risk for more bleeding.
References
- Gauer, R. L. (2022). Thrombocytopenia: Evaluation and management. American Family Physician, 106(3), 305-313. https://www.aafp.org/pubs/afp/issues/2022/0900/thrombocytopenia.html
Zheng, X. L., et al. (2025). 2025 focused update of the 2020 ISTH guidelines for thrombotic thrombocytopenic purpura. Journal of Thrombosis and Haemostasis. https://www.sciencedirect.com/science/article/pii/S1538783625003605










