Last Updated on October 21, 2025 by mcelik
We often hear about blood clots and their risks. But what is a thrombus? It’s a solid or semisolid mass in our blood system. It’s made of blood parts like platelets, fibrin, red and white blood cells. Understand the thrombus meaning is and learn key facts about thrombi and blood clots in the body.
Thrombosis is when a blood clot forms inside a blood vessel. This blocks blood flow in our system. Knowing about thrombi risks is key for early treatment and care. At LivHospital, we focus on advanced care and solutions for blood clots.
It’s important to know how blood clots form. This helps us understand the balance between stopping bleeding and avoiding clots. Blood clotting involves many parts of the blood, like platelets, fibrin, and blood cells.
Blood clotting is how the body reacts to injury. When a blood vessel gets hurt, the body quickly acts. It uses platelets and the coagulation cascade to make a clot.
This process has several steps. First, the blood vessel tightens. Then, platelets form a plug. Lastly, fibrin makes a clot that traps blood cells and platelets.
The coagulation cascade is a series of chemical reactions. Fibrin forms a mesh that traps blood cells and platelets. This creates a solid clot. Clotting factors, proteins in blood plasma, help control this process.
While clotting is vital, it can become harmful. A clot that blocks a key vessel can cause serious problems. This includes stroke or myocardial infarction.
Understanding what causes harmful clotting is key. Risk factors like genetics, lifestyle, and medical conditions can lead to dangerous clots.
| Component | Role in Clot Formation |
| Platelets | Activate and aggregate to form the initial plug |
| Fibrin | Forms a mesh-like structure to stabilize the clot |
| Blood Cells | Trapped within the fibrin mesh, contributing to clot volume |
“The formation of a thrombus is a complex interplay of various cellular and molecular components. Understanding this process is key for finding effective treatments.”
The term ‘thrombus’ is key in healthcare. It’s linked to serious health issues like strokes and heart attacks. We’ll look into what ‘thrombus’ means, its history, and how it differs from an embolus.
The word ‘thrombus’ comes from the Greek “thrombos,” meaning clump. It’s been used in medicine for over a century to describe blood clots in vessels. Knowing its roots helps us understand its role in medical history.
Thrombi have been linked to many health problems. Over time, doctors have learned a lot about them. This knowledge has helped in treating heart and blood vessel diseases.
It’s important to know the difference between a thrombus and an embolus. A thrombus is a clot in a blood vessel. An embolus is a clot or particle that travels and blocks a vessel. If a thrombus breaks off, it becomes an embolus, which can cause serious problems like pulmonary embolism or stroke.
To better understand the differences and similarities, let’s compare them in a table:
| Characteristics | Thrombus | Embolus |
| Definition | A blood clot that forms within a blood vessel | A clot or particle that travels through the bloodstream and lodges in a vessel |
| Formation Location | Forms in situ within a blood vessel | Forms elsewhere and travels to lodge in a vessel |
| Clinical Implication | Can cause local obstruction or remain asymptomatic | Can cause obstruction at a distant site, leading to severe conditions |
Knowing the difference between a thrombus and an embolus is vital for treating vascular diseases. It shows how important accurate medical terms are. It also highlights the need for deep knowledge in handling blood clot issues.
Knowing how a thrombus works is key to understanding heart problems. A thrombus, or blood clot, is made up of many parts. These parts include cells and molecules.
Platelets, fibrin, and blood cells are the main parts of a thrombus. Platelets are tiny cells that start the clotting process. When a blood vessel gets hurt, platelets stick together to form a plug.
Fibrin is a liver-made protein that turns into strands during clotting. These strands catch blood cells, making the clot stable. The mix of these parts changes based on the clot’s location and type.
A blood clot diagram shows how a thrombus is structured. It displays platelets, fibrin strands, and blood cells trapped in the clot. Seeing a thrombus’s layout helps us understand how it forms and works.
The structure of a thrombus changes over time. This is because the body breaks down clots through fibrinolysis. Keeping the balance between clotting and dissolving is vital for healthy blood vessels.
In summary, a thrombus is a complex mix of blood parts. Knowing its makeup and structure is key to understanding heart diseases and finding treatments.
Knowing the different types of thrombi is key to treating blood clots well. They can form in arteries, veins, and the heart. Each place has its own special traits and health issues.
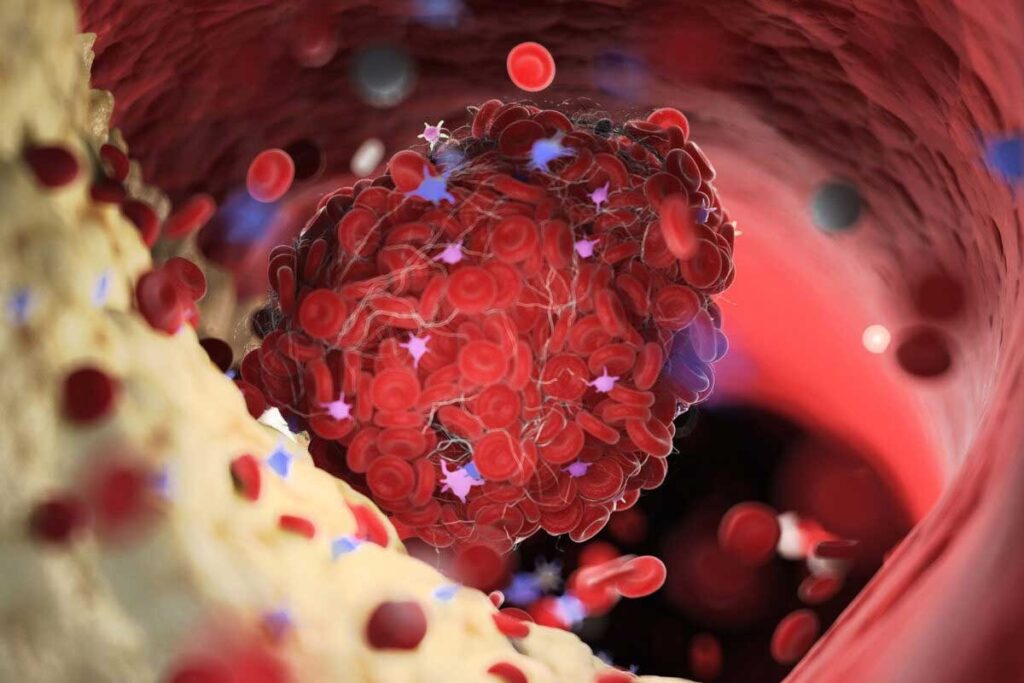
Arterial thrombi happen in arteries, which carry blood away from the heart. They’re linked to atherosclerosis, where plaque builds up. This can cause blood flow problems and lead to clotting.
Arterial thrombi can block blood flow, harming tissues.
The main features of arterial thrombi are:
Venous thrombi form in veins, which bring blood back to the heart. They’re common in the legs and linked to deep vein thrombosis (DVT). They’re caused by blood stasis, clotting issues, or damage to the vein lining, as Virchow’s triad explains.
The dangers of venous thrombi include:
Cardiac thrombi form in the heart, usually due to heart rhythm problems, heart attacks, or heart muscle issues. These clots are risky because they can travel to the brain or limbs, causing strokes or limb problems.
Cardiac thrombi’s main traits are:
In summary, knowing about the different thrombi types is vital for good treatment. Each type has its own causes and health risks, needing a specific care plan.
Knowing where thrombi form is key to diagnosing and treating conditions. Thrombi can appear in different parts of the body, each with its own effects. The place a thrombus forms affects its impact and symptoms.
Cerebral thrombi form in the brain’s blood vessels and can lead to ischemic strokes. A thrombus in a cerebral artery blocks oxygen and nutrients to brain tissue. This can cause a stroke, with severity based on the thrombus’s size and location.
Risk factors for cerebral thrombi include high blood pressure, diabetes, and atherosclerosis. Knowing these risk factors helps prevent and treat early.
Coronary thrombi form in arteries that supply blood to the heart. A coronary thrombus can block an artery, leading to a heart attack. This blockage damages heart muscle by cutting off oxygen and nutrients.
“The formation of a coronary thrombus is often the result of plaque rupture in an atherosclerotic artery, highlighting the importance of managing cardiovascular risk factors.”
Deep vein thrombosis (DVT) occurs in the deep veins, usually in the legs. It causes pain, swelling, and warmth in the affected limb. If part of the thrombus breaks off, it can travel to the lungs and cause a pulmonary embolism, a serious condition.
| Condition | Location | Potential Complication |
| Cerebral Thrombi | Brain | Ischemic Stroke |
| Coronary Thrombi | Heart | Myocardial Infarction |
| Deep Vein Thrombosis | Legs | Pulmonary Embolism |
In conclusion, the location of a thrombus is critical for its impact on the body. Knowing where thrombi can form and their risks is essential for diagnosis and treatment.
An occlusive thrombus blocks the whole blood vessel. This is a serious emergency because it stops blood flow to tissues or organs. It’s a big problem.
The formation of an occlusive thrombus is complex. It starts with platelet activation and the coagulation cascade. This leads to fibrin and blood cells building up.
As the thrombus grows, it can block the vessel completely. Thrombus formation is influenced by many factors. These include blood flow, vessel wall issues, and blood composition.
“The complete obstruction of a blood vessel by a thrombus is a catastrophic event,” doctors say. It can cause severe tissue damage or organ dysfunction. The outcome depends on the vessel’s location, size, and collateral circulation.
Tissue ischemia happens when blood flow is not enough. An occlusive thrombus can cause severe ischemia. This can lead to tissue necrosis if not treated quickly.
The effects of tissue ischemia and necrosis are severe. They can cause organ failure or even death. It’s a serious situation.
Understanding occlusive thrombi and their effects is key to finding treatments. Quick medical action is needed to restore blood flow and prevent permanent damage.
Knowing what increases the risk of thrombus is key to preventing and managing blood clots. Many factors can lead to clot formation. We’ll look at each one closely.
Genetics play a big part in clotting disorders. If your family has a history of blood clots, you might be at higher risk. Certain genetic mutations, like Factor V Leiden, can also raise your risk. We’ll dive into these genetic risks and what they mean for your clotting risk.
Key genetic risk factors include:
Our lifestyle and environment also affect our clotting risk. Smoking harms blood vessels and raises arterial clot risk. Being inactive or overweight can also increase venous clot risk. We’ll see how these habits impact clotting.
Lifestyle changes can help:
Some medical conditions raise your risk of blood clots. Conditions like cancer, heart disease, and autoimmune disorders can increase clot risk. We’ll explore how these conditions affect clotting risk.
Medical conditions that increase clot risk:
Virchow’s triad explains the three main causes of blood clots: changes in blood flow, increased clotting tendency, and damage to blood vessel lining. Understanding this triad is key to grasping how clots form. We’ll break down each part and its role in clotting risk.
The components of Virchow’s triad:
By understanding these risk factors and how they work together, we can better prevent and manage blood clots. Knowing about genetic predispositions, lifestyle factors, medical conditions, and Virchow’s triad is vital for reducing clot risk and improving patient care.
The COVID-19 pandemic has shown us how SARS-CoV-2 affects our blood’s ability to clot. Studies are revealing that microthrombi are key in how the disease works.
SARS-CoV-2 can mess with our blood’s clotting system, raising the risk of blood clots. Microthrombi formation is a big part of this, blocking small blood vessels and harming organs.
“Microthrombi in COVID-19 patients are linked to more severe disease and death,” studies say. SARS-CoV-2 affects coagulation in many ways, through different cells and molecules.
Microthrombi in COVID-19 patients can really hurt our organs. For example, in the lungs, they can make acute respiratory distress syndrome (ARDS) worse, a big problem in severe cases.
It’s important to understand microthrombi’s role in COVID-19 to find better treatments. As we learn more, treating coagulation problems will be key in fighting the disease.
“Recognizing microthrombi as a major factor in COVID-19 highlights the need for a full approach to care. This includes anticoagulant therapies and other ways to lower the risk of blood clots.”
Thrombosis symptoms vary based on where and what type of clot forms. Clots can block arteries or veins. Symptoms range from mild to severe, depending on the clot’s size and the organ it affects.
Arterial thrombosis happens when a clot blocks an artery. This can cut off blood to vital organs. Symptoms can be sudden and severe.
A clot in the heart’s arteries can cause a heart attack. Symptoms include chest pain, shortness of breath, and dangerous heart rhythms.
Clots in the brain’s arteries can lead to a stroke. Symptoms include sudden weakness, trouble speaking, and vision changes.
Venous thrombosis occurs when a clot forms in a vein. Deep vein thrombosis (DVT) often affects the legs. Symptoms include swelling, pain, warmth, and redness in the affected limb.
Some DVT cases have no symptoms. It’s important to know the risk factors.
If a clot breaks loose and goes to the lungs, it can cause a pulmonary embolism. Symptoms include sudden shortness of breath, chest pain, and coughing up blood.
Certain symptoms need immediate medical help. These include:
Knowing these emergency signs can save lives. If you or someone you know has these symptoms, seek medical help right away.
Here’s a summary of key symptoms for arterial and venous thrombosis:
| Condition | Common Symptoms |
| Arterial Thrombosis | Chest pain, shortness of breath, sudden weakness or numbness, difficulty speaking |
| Venous Thrombosis (DVT) | Swelling, pain, warmth, redness in the affected limb |
| Pulmonary Embolism | Sudden shortness of breath, chest pain, coughing up blood |
Knowing how to spot and stop thrombi is key to better health. Doctors use a mix of checks, scans, and blood tests to find and understand thrombi.
Many scans help find thrombi:
Lab tests are also vital for finding thrombi. They include:
Stopping thrombi is just as important as finding them. People at high risk can try these steps:
Understanding how to diagnose and prevent thrombi helps doctors keep patients safe. This leads to better health outcomes.
Knowing about thrombi is key to staying healthy. We’ve looked into what thrombus is, how it forms, and its dangers. We’ve also talked about how it can cause serious problems like stroke and heart attack.
Being aware of thrombi is essential for preventing and treating related issues. By knowing the risks and signs, people can get help fast. This can lower the chance of serious problems.
Understanding thrombi can improve health outcomes. Thrombi can appear anywhere in the body and cause big problems if not treated. By spreading the word about thrombi, we can help lower the number of cases and deaths.
A thrombus is a blood clot that forms inside a blood vessel. It blocks the blood flow. It’s made of platelets, fibrin, and blood cells.
A thrombus forms in a blood vessel. An embolus is a clot that breaks loose and travels through the blood. It can block blood flow elsewhere in the body.
Risk factors include genetic predispositions and lifestyle choices like smoking and obesity. Medical conditions like cancer and heart disease also increase the risk. Changes in blood flow, hypercoagulability, and injury to the blood vessel walls are part of Virchow’s triad.
Symptoms depend on where the thrombus is. Arterial thrombosis can cause pain, numbness, and weakness. Venous thrombosis may cause swelling, redness, and warmth. Severe chest pain, trouble breathing, and sudden numbness or weakness are emergency signs.
Diagnosis uses imaging like ultrasound, CT scans, and MRI. Laboratory tests like D-dimer assays also help. They show where and if a thrombus is present.
Yes, prevention includes anticoagulant medications and compression stockings. Regular exercise and a healthy diet also help. People at high risk, like those with a history of thrombosis, should take these steps.
An occlusive thrombus blocks blood flow completely. It can cause tissue ischemia and necrosis.
Research shows SARS-CoV-2 can affect blood clotting. This leads to microthrombi, which can harm organs in severe COVID-19 cases.
Consequences include tissue ischemia, necrosis, and organ dysfunction. The severity depends on the thrombus’s location and size. In severe cases, it can cause life-threatening conditions like stroke or heart attack.
References
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us