Every year, thousands of people face thyroid removal surgery. It’s a turning point, balancing hope for a cure with the knowledge of lasting changes. The thought of thyroid surgery can be scary. But, thanks to medical progress, results have gotten much better.
In the US, about 44,000 new cases of thyroid cancer happen every year. The 5-year survival rate is 98.4%. This means most people do well after thyroidectomy. We aim to provide top-notch care and support for patients from around the world.
Key Takeaways
- Thyroid removal is a significant surgery, but modern techniques have improved outcomes.
- The prevalence of thyroid cancer is substantial, with 44,000 new cases in the US each year.
- The 5-year relative survival rate for thyroid cancer is 98.4%.
- Proper treatment significantly improves patient outcomes.
- Advancements in medical care have made thyroid surgery more manageable.
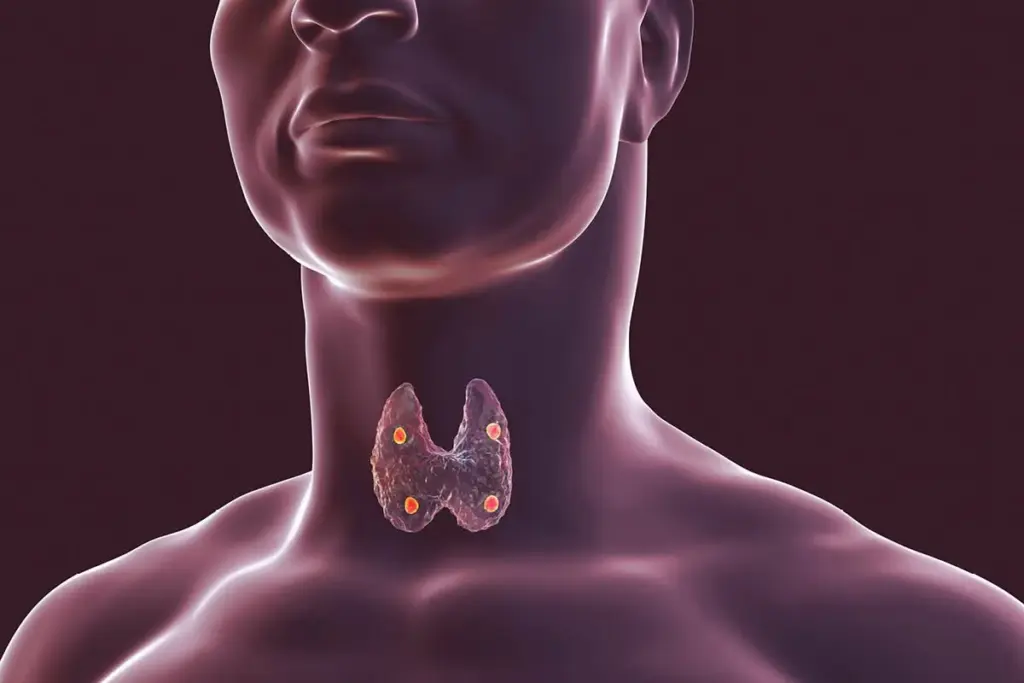
Understanding the Thyroid Gland and Its Functions

The thyroid gland is a butterfly-shaped organ in the neck. It makes thyroid hormones, which are key for our body’s functions. Knowing about its anatomy and role helps us understand the effects of thyroid gland removal or thyroidectomy surgery.
Anatomy of the Thyroid Gland
The thyroid gland is in the front of the neck, below the Adam’s apple. It looks like a butterfly, with two lobes and a narrow isthmus. It has a lot of blood vessels, which is important for making thyroid hormones.
This gland’s structure is made for producing and releasing thyroid hormones into the blood. The pituitary gland, at the brain’s base, controls this with thyroid-stimulating hormone (TSH).
Role of Thyroid Hormones in the Body
Thyroid hormones, like thyroxine (T4) and triiodothyronine (T3), are vital. They help with metabolism, heart rate, and energy levels. They also help with growth and development, mainly in kids and teens.
It’s important to have the right balance of thyroid hormones. Too much or too little can cause health problems. This might mean needing a thyroid operation or thyroidectomy removal.
What is a Thyroidectomy?
Thyroidectomy, or thyroid removal surgery, is a medical operation. It treats various thyroid disorders, like cancer and nodules. This surgery removes part or all of the thyroid gland. The thyroid gland is a vital endocrine gland in the neck.
Definition and Types of Thyroidectomy Procedures
A thyroidectomy can be categorized into several types. These depend on how much of the gland is removed. The main types are:
- Total Thyroidectomy: This involves removing the whole thyroid gland. It’s often recommended for thyroid cancer or severe thyroid disease.
- Partial or Lobectomy: This type removes one lobe of the thyroid gland. It’s considered when the disease is only on one side of the gland.
|
Type of Thyroidectomy |
Description |
Common Indications |
|---|---|---|
|
Total Thyroidectomy |
Removal of the entire thyroid gland |
Thyroid cancer, severe thyroid disease |
|
Partial/Lobectomy |
Removal of one lobe of the thyroid gland |
Disease limited to one lobe, suspicious nodules |
When is Thyroid Removal Necessary?
Thyroid removal is necessary in several situations. These include:
- Thyroid Cancer: Confirmed or suspected thyroid cancer is a primary reason for thyroidectomy.
- Goiter or Large Nodules: Symptoms or suspected malignancy in goiters or nodules often require surgery.
- Hyperthyroidism: Surgery is an option when hyperthyroidism can’t be controlled with medication or radioactive iodine.
Understanding thyroidectomy procedures is key for those with thyroid issues. Consulting with healthcare professionals helps find the best treatment plan for each condition.
Is Having a Thyroidectomy Really a Big Deal?
Medical technology and surgery have improved a lot. Now, thyroidectomy is safer and quicker. Patients get better results and heal faster.
Medical Perspective on Thyroid Removal
Thyroidectomy is a big surgery but often needed for thyroid issues. Thyroidectomy surgeons are key to success. They choose between thyroid lobectomy or total thyroidectomy based on the patient’s needs.
New surgery methods have made thyroidectomy better. Surgeons now do less damage and patients heal faster. This makes surgery a good option for many.
Quality of Life After Surgery
People worry about life after thyroidectomy. But, most can live normally again. Hormone therapy is needed for some, but it’s manageable.
Recovery means adjusting to new meds and health checks. But, most can get back to normal in weeks. Following doctor’s orders and attending check-ups is key.
Modern Advances in Thyroid Surgery
Thyroid surgery has gotten better, with new, less invasive methods. Minimally invasive procedures and robotic-assisted surgery reduce scars and recovery time.
These advances make recovery better and the experience more positive. As technology grows, thyroid surgery will keep getting safer and more effective.
Common Reasons for Thyroid Removal

Several thyroid conditions may require the removal of the thyroid gland, a procedure known as thyroidectomy. This surgery is often considered when thyroid issues become severe or malignant. We will outline the common reasons for thyroid removal, including thyroid cancer, goiter, nodules, and hyperthyroidism.
Thyroid Cancer
Thyroid cancer is a significant indication for thyroidectomy. The most common types of thyroid cancer are papillary, follicular, medullary, and anaplastic thyroid cancer. Thyroid carcinoma surgery is often the primary treatment for thyroid cancer, and in many cases, it involves the removal of the entire thyroid gland.
The decision to perform a thyroidectomy for cancer is based on the type and stage of the cancer, as well as the patient’s overall health. In some cases, a partial thyroidectomy may be performed, where only the affected portion of the gland is removed.
Goiter and Nodules
A goiter refers to the enlargement of the thyroid gland, which can cause discomfort, difficulty swallowing, and breathing problems. Thyroid nodules are lumps that form within the thyroid gland and are very common. While most nodules are benign, some can be cancerous.
When goiter or nodules cause significant symptoms or are suspected to be malignant, thyroid removal surgery may be recommended. The extent of the surgery depends on the size and nature of the goiter or nodules.
Hyperthyroidism
Hyperthyroidism is a condition where the thyroid gland produces excess thyroid hormones, leading to symptoms such as weight loss, palpitations, and anxiety. In some cases, thyroidectomy surgery is considered for the treatment of hyperthyroidism, when other treatments have failed or are not suitable.
Drugs for thyroidectomy are often used to manage the condition before surgery, ensuring the patient is euthyroid (has normal thyroid hormone levels) before undergoing the procedure.
In conclusion, thyroid removal is a necessary treatment for various thyroid conditions. Understanding the reasons for thyroidectomy can help patients prepare for the surgery and the subsequent management of their thyroid health.
Thyroid Cancer Statistics in the United States
In the United States, a lot of people get thyroid cancer every year. There are trends in how often it happens. Knowing about these stats is key for both patients and doctors.
Incidence and Prevalence
About 44,000 new cases of thyroid cancer are found in the US each year. This is a big part of all cancer cases. It shows how important it is to catch it early.
More people are getting thyroid cancer over time. This is because doctors can find it better and more people know about it.
|
Year |
Estimated New Cases |
Prevalence Rate |
|---|---|---|
|
2015 |
62,450 |
12.1 per 100,000 |
|
2020 |
44,000 (approx.) |
13.4 per 100,000 |
Survival Rates After Treatment
The 5-year survival rate for thyroid cancer in the US is 98.4%. This means most people live a long time after treatment. This is thanks to treatments like thyroidectomy removal and surgery.
Experts say, “The high survival rate for thyroid cancer is because of early detection and better surgery, like thyroid operation and thyroidectomy.”
“Early detection and treatment of thyroid cancer significantly improve patient outcomes, with many patients experiencing full recovery.”
Pre-Surgery Evaluation and Preparation
A thorough pre-surgery assessment is key for those about to have a thyroidectomy. It makes sure patients are ready for surgery, reducing risks and improving results.
Diagnostic Tests
Several tests are done before a thyroidectomy to check the thyroid gland and the patient’s health. These include:
- Thyroid function tests to check hormone levels
- Ultrasound to see the thyroid gland and nodules
- Fine-needle aspiration biopsy to find cancerous cells
- Blood tests to check overall health and find any issues
|
Diagnostic Test |
Purpose |
|---|---|
|
Thyroid Function Tests |
Evaluate thyroid hormone levels |
|
Ultrasound |
Visualize thyroid gland and nodules |
|
Fine-needle Aspiration Biopsy |
Check for cancerous cells |
|
Blood Tests |
Assess overall health and detect abnormalities |
Consultation with Specialists
Patients will meet with several specialists before surgery. These include:
- Endocrinologists to manage thyroid hormone levels
- Surgeons specializing in thyroidectomy procedures
- Anesthesiologists to discuss anesthesia options
These meetings are important. They help address concerns, explain the surgery, and plan for recovery.
Physical Preparation
Getting physically ready is essential for a successful thyroidectomy. Patients should:
- Eat a healthy diet full of nutrients
- Stay hydrated and avoid hard activities before surgery
- Tell their surgeon about any medications or supplements
They might also need to stop certain medications that could affect surgery or healing.
Modern Thyroidectomy Techniques and Approaches
Modern thyroidectomy techniques have improved a lot. They offer better results for patients. New surgical tools and methods have made thyroid surgery safer and more effective.
Traditional Open Surgery
Traditional open thyroidectomy uses a neck incision to reach the thyroid gland. This method has been used for years. But, new techniques have made it better, with less scarring and faster recovery. Open surgery is also good for complex cases or when other methods don’t work.
Minimally Invasive Procedures
Minimally invasive thyroidectomy is becoming more popular. It has less pain and quicker recovery times. This method uses small incisions and results in less scarring. We use advanced tools for precise and safe surgery.
Robotic-Assisted Thyroidectomy
Robotic-assisted thyroidectomy is a big step forward in thyroid surgery. It allows for precise removal of the thyroid gland with less damage to nearby tissues. Robotic systems can lead to better results and happier patients.
Endoscopic Techniques
Endoscopic thyroidectomy uses a small camera and instruments through tiny incisions. It’s great for those worried about scarring. We perform endoscopic techniques with great care for the best results.
The table below shows the main features and benefits of modern thyroidectomy techniques:
|
Technique |
Key Features |
Benefits |
|---|---|---|
|
Traditional Open Surgery |
Standard incision in the neck |
Reliable for complex cases, refined to minimize scarring |
|
Minimally Invasive Procedures |
Smaller incisions, advanced surgical tools |
Less post-operative pain, quicker recovery |
|
Robotic-Assisted Thyroidectomy |
Precise dissection using robotic systems |
Less trauma to surrounding tissues, improved outcomes |
|
Endoscopic Techniques |
Small camera and instruments through tiny incisions |
Minimal scarring, beneficial for cosmetic concerns |
Understanding modern thyroidectomy techniques helps patients make better choices. We aim to provide the best treatment for each patient, ensuring the best results.
The Thyroidectomy Procedure Explained
Understanding the thyroidectomy procedure is key for those thinking about thyroid removal surgery. We’ll cover the main parts of the operation, from start to finish.
Anesthesia and Surgical Setup
A thyroidectomy is usually done under general anesthesia. This keeps the patient comfortable and pain-free. The surgical team will place the patient on the table, with their neck slightly up.
“General anesthesia creates a safe and controlled setting for both the patient and the surgical team,” says a top thyroid surgeon. “It lets us focus on the surgery’s details without worrying about the patient’s comfort.”
Step-by-Step Surgical Process
The thyroidectomy procedure has several important steps:
- Making a precise incision in the neck, usually along a natural skin crease to minimize visible scarring.
- Carefully dissecting through the tissues to expose the thyroid gland.
- Identifying and preserving the parathyroid glands and recurrent laryngeal nerve.
- Removing the thyroid gland, either partially or completely, depending on the patient’s condition.
- Closing the incision with sutures or staples, often using a technique that minimizes scarring.
Duration and Hospital Stay
The length of a thyroidectomy can vary, but it usually takes 1 to 3 hours. The surgery’s length depends on its complexity and if other procedures are done at the same time.
Most patients stay in the hospital for at least one night after surgery. The healthcare team watches for any immediate problems and makes sure the patient is recovering well before they go home.
Following the surgeon’s instructions and attending follow-up appointments is vital for a smooth recovery.
Choosing the Right Surgeon for Your Thyroidectomy
Finding the right thyroidectomy surgeon is key for a good surgery. Your surgeon’s skills and experience greatly affect your surgery’s success.
Importance of Surgical Volume and Experience
Studies show that patients with surgeons who do 26 or more thyroid surgeries a year do better. This shows why picking a surgeon with lots of experience is important.
Choosing an experienced surgeon offers many benefits:
- Less chance of complications
- More precise surgery
- Better care after surgery
- Happier patients
Questions to Ask Your Surgeon
When talking to possible thyroidectomy surgeons, ask the right questions. This helps you understand their experience and how they work.
Here are some questions to ask:
- How many thyroid surgeries have you done?
- What’s your rate of complications?
- What method do you use for thyroid surgery?
- How will you take care of me after surgery?
Finding High-Volume Thyroid Surgeons
To find a surgeon who does many thyroid surgeries, try these:
- Ask your doctor for suggestions
- Look up certified thyroid surgeons through medical societies
- Read online reviews and patient stories
By doing these things, you can find a skilled and experienced thyroidectomy surgeon.
Potential Risks and Complications of Thyroidectomy
It’s important for patients to know the risks of thyroidectomy. This surgery removes the thyroid gland and has its own set of risks and complications.
Vocal Cord Paralysis
Vocal cord paralysis is a serious issue that can happen during surgery. It can cause voice changes, like hoarseness or losing your voice. Studies show this happens in about 2-5% of cases.
Hypoparathyroidism
Hypoparathyroidism is another risk of thyroidectomy. It happens when the parathyroid glands are damaged or removed. This leads to low calcium levels in the blood, causing symptoms like numbness and muscle cramps. “The risk of hypoparathyroidism after thyroidectomy is a significant concern, as it can lead to long-term health issues if not properly managed,” say doctors.
Bleeding and Infection
Bleeding and infection are risks with any surgery, including thyroidectomy. Bleeding can cause swelling that presses on important neck structures. Infection is rare but can happen. Doctors use careful techniques and antibiotics to reduce these risks.
Other Possible Complications
Other complications include wound issues like seroma or keloid formation, and reactions to anesthesia. While these are less common, it’s good to know about them.
In summary, thyroidectomy is generally safe but comes with risks. Knowing these risks helps patients make informed choices. Talking to a healthcare provider about these complications prepares patients for what might happen with thyroid removal surgery.
Recovery Timeline After Thyroid Removal
Knowing what to expect after thyroid surgery is key. Everyone recovers differently, but there are common steps most people follow.
Immediate Post-Operative Period
Right after surgery, patients stay in the recovery room for a few hours. Many go home the same day, but some might need to stay overnight. During this time, you might feel:
- Neck pain or discomfort
- Swelling or bruising around the incision site
- Hoarseness or changes in voice
- Difficulty swallowing
These symptoms are usually short-lived and can be managed with pain meds and other support.
First Month Post-Surgery
In the first month, you’ll likely start feeling better. But, it’s important to:
- Follow your surgeon’s advice on wound care and follow-up visits
- Slowly increase your physical activity as you feel able
- Watch for any signs of complications, like infection or severe pain
Most people can get back to their usual activities in 2-4 weeks.
Long-term Recovery Expectations
Recovering from thyroid surgery long-term means adjusting to life without a thyroid. This often means starting hormone replacement therapy to manage hypothyroidism. You should:
- Work closely with your healthcare provider to adjust medication as needed
- Go to regular check-ups to keep an eye on your thyroid hormone levels
- Be aware of the long-term effects of hormone replacement therapy
With the right care, most people can live active, normal lives after thyroid surgery.
We support our patients every step of the way through recovery after thyroidectomy. We make sure they get all the care and support they need.
Life Without a Thyroid: Hormone Replacement Therapy
Living without a thyroid gland means taking thyroid hormone replacement medication every day. After a thyroidectomy, the body can’t make thyroid hormones anymore. These hormones are key for metabolism, energy, and health.
Adapting to life without a thyroid can be tough. But, with the right treatment, people can live normal, active lives. The key is understanding and following hormone replacement therapy.
Understanding Levothyroxine
Levothyroxine is the main medication for thyroid hormone replacement. It’s a synthetic version of thyroxine (T4), which the body turns into triiodothyronine (T3). T3 is the active hormone that helps with many body functions.
Levothyroxine is chosen because it lasts long in the body. This means it only needs to be taken once a day. It’s best to take it on an empty stomach in the morning for better absorption.
Dosage Adjustments and Monitoring
Finding the right dose of levothyroxine is key and might take some time. Things like weight, age, and other health issues can affect the dose. Regular blood tests help check hormone levels and adjust the dose as needed.
We suggest patients work closely with their doctors to get their levothyroxine dose just right. This teamwork helps keep hormone levels in check. It prevents both too little and too much thyroid hormone.
Potential Side Effects and Management
Levothyroxine is usually safe but can have side effects. These might include changes in appetite, weight, and mood. Rarely, it can cause allergic reactions or more serious side effects.
To handle side effects, it’s important to talk to your doctor about any changes or concerns. They might adjust the dosage or switch to a different type of levothyroxine to help.
In summary, hormone replacement therapy is essential after a thyroidectomy. By knowing how levothyroxine works, following the treatment plan, and working with doctors, patients can keep their hormone levels right. This helps them stay healthy and feel good.
Dietary and Lifestyle Considerations After Thyroidectomy
Recovering from thyroid surgery is more than just healing from the operation. It’s about making smart choices about what you eat and how you live. Understanding the role of nutrition, exercise, and managing your energy is key to feeling your best.
Nutrition Guidelines
Eating well is essential after thyroid surgery. Focus on foods that help your body heal and stay healthy. Include fruits, veggies, whole grains, lean proteins, and healthy fats in your diet. Drinking plenty of water is also important; aim for eight glasses a day.
Some people might need to change their diet based on their health issues. For example, those with hypothyroidism should watch their iodine intake. Talking to a healthcare provider or a dietitian can help you make the right choices.
|
Nutrient |
Food Sources |
Benefits |
|---|---|---|
|
Iodine |
Iodized salt, seaweed, dairy products |
Essential for thyroid hormone production |
|
Protein |
Lean meats, fish, eggs, legumes |
Supports healing and muscle strength |
|
Calcium |
Dairy products, leafy greens, fortified foods |
Crucial for bone health |
Physical Activity Recommendations
It’s good to stay active after thyroid surgery. Start with easy activities like walking or yoga. Gradually add more intensity as you feel more comfortable and have more energy. Always listen to your body and don’t push too hard, at least not at first.
Exercise helps you regain strength and can also boost your mood. But, check with your doctor before starting any new exercise, even if you’re feeling okay.
Managing Energy Levels
Energy levels can change after thyroid surgery. Make sure to rest and balance activity with rest. Don’t do too much and take breaks when needed.
Having a routine that includes rest, exercise, and social time can help keep your energy up. Also, getting enough sleep and eating well are important for your energy.
By choosing wisely about your diet and lifestyle, you can improve your recovery and quality of life after thyroid surgery.
International Standards and Best Practices in Thyroid Surgery
Thyroid surgery is key in treating many thyroid problems. Following international standards is vital for the best results. At livhospital.com, we stick to these standards to give our patients top-notch care.
We use the latest methods and techniques in thyroid surgery. This ensures our patients get all-around care. We think a team effort is best for managing thyroid issues.
Multidisciplinary Approach to Thyroid Care
A team of experts works together for complete care. This team includes endocrinologists, surgeons, and more. Together, they make sure patients get the right diagnosis and treatment.
At livhospital.com, our thyroid surgery team is highly skilled. They work with other specialists to create treatment plans that fit each patient’s needs.
|
Specialist |
Role in Thyroid Care |
|---|---|
|
Endocrinologist |
Diagnoses and manages thyroid disorders |
|
Surgeon |
Performs thyroid surgery, including thyroidectomy |
|
Radiologist |
Provides imaging studies to aid in diagnosis |
|
Pathologist |
Examines tissue samples to confirm diagnosis |
Quality Improvement Initiatives
We always look to improve our quality. We update our methods based on new research and guidelines. This helps us use the latest techniques to better our patients’ outcomes.
“The key to successful thyroid surgery lies in a combination of technical skill, experience, and a patient-centered approach.”
— Expert Thyroid Surgeon
Patient Safety Protocols
Keeping our patients safe is our main goal. We follow strict safety rules, like proper patient identification and infection control. Our team works hard to make sure our patients feel safe and supported.
By sticking to international standards in thyroid surgery, we ensure our patients get the best care. Whether it’s for thyroid cancer or carcinoma surgery, our team aims for outstanding results.
Emotional and Psychological Aspects of Thyroid Removal
Thyroid surgery can deeply affect patients emotionally and psychologically. Choosing to have a thyroidectomy is a big decision. It leads to a journey filled with physical and emotional challenges.
Coping with Body Changes
Patients often feel a range of emotions after thyroid surgery. The loss of the thyroid gland can make them question their identity and body control. It’s important to recognize these feelings as a normal part of healing.
Adjusting to life after surgery can be tough. This includes getting used to hormone replacement therapy. Having support from healthcare providers, family, and friends is key during this time.
Managing Mood Fluctuations
Mood swings and emotional ups and downs are common after surgery. Hormone level changes can cause anxiety, depression, or irritability. It’s vital to keep an eye on and manage these mood swings for overall health.
|
Emotional Challenge |
Management Strategy |
|---|---|
|
Anxiety |
Relaxation techniques, such as deep breathing or meditation |
|
Depression |
Counseling or therapy, support groups |
|
Irritability |
Regular exercise, stress management techniques |
Support Resources and Communities
Having the right support can greatly help after thyroidectomy. Support groups, online or in-person, offer a sense of belonging and understanding.
Healthcare providers can also guide you through the emotional side of thyroid removal. Talking openly with your healthcare team is essential for overcoming challenges.
By understanding the emotional and psychological effects of thyroidectomy and seeking support, patients can better handle their recovery journey.
Conclusion: Living a Full Life After Thyroid Removal
Having a thyroidectomy is a big deal, but with the right care, you can live fully after surgery. We’ve looked at what the thyroid gland does and the types of surgeries for it.
Today’s thyroid surgery methods are safer, helping you heal fast. With a skilled surgeon and team, you can face surgery with confidence.
Hormone therapy is key after thyroid surgery. Knowing about levothyroxine and how to adjust it helps manage your health.
It’s possible to live a full life after thyroid surgery. With the right medical support, you can beat the challenges and enjoy your life every day.
FAQ
What is a thyroidectomy?
A thyroidectomy is a surgery to remove part or all of the thyroid gland. It treats conditions like thyroid cancer, goiter, and hyperthyroidism.
Why is thyroidectomy necessary?
It’s needed for thyroid cancer, large goiters, and hyperthyroidism not helped by other treatments. A healthcare provider decides after a thorough check-up.
What are the different types of thyroidectomy procedures?
There are total, partial (thyroid lobectomy), and minimally invasive thyroidectomies. The choice depends on the condition and the patient’s health.
How long does it take to recover from a thyroidectomy?
Recovery time varies, but most people can get back to normal in a few weeks. The first few days may be uncomfortable and swollen, but pain meds help.
What are the possible risks and complications of thyroidectomy?
Risks include vocal cord paralysis, hypoparathyroidism, bleeding, and infection. But, these are rare with an experienced surgeon.
Will I need hormone replacement therapy after a thyroidectomy?
Yes, if you have a total thyroidectomy, you’ll need hormone therapy. The dosage is adjusted based on blood tests to keep hormone levels right.
How do I choose the right surgeon for my thyroidectomy?
Look for a surgeon with lots of experience and good patient outcomes. Ask about their approach and complication rates.
What are the benefits of minimally invasive thyroidectomy?
It has smaller incisions, less pain, and quicker recovery. It’s for some patients and done by skilled surgeons.
Can I expect to live a normal life after a thyroidectomy?
Yes, with proper care and follow-up, most people can live normally. This includes hormone therapy and regular doctor visits.
What dietary and lifestyle changes should I make after a thyroidectomy?
Eat a balanced diet, stay hydrated, and exercise regularly. These help manage energy and overall health.
How will I manage my energy levels after a thyroidectomy?
Rest well, exercise, and eat right. Working with your doctor to keep hormone levels right is also key.
Are there any support resources available for patients after a thyroidectomy?
Yes, there are online communities, support groups, and counseling. They help with the emotional and psychological aspects of thyroid removal.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK563279/





