
When the thyroid gland is removed through thyroid surgery, the body loses its main source of thyroid hormones. These hormones are key for controlling metabolism, energy, and overall health.
Recent studies show that total thyroidectomy happens in about 89% of cases. This shows how common this surgery is.
We will look into what happens after thyroid removal surgery. We’ll also talk about how to live without a thyroid gland. Thyroid surgery is often used to treat thyroid cancer, hyperthyroidism, and large goiters.
Key Takeaways
- Thyroid removal eliminates the body’s source of thyroid hormones.
- Patients require lifelong management to maintain hormone balance.
- Recent research highlights trends in complications and rising thyroid cancer rates.
- Evolving surgical recommendations aim to improve patient outcomes.
- Understanding the effects of thyroid removal is key for patients undergoing this surgery.
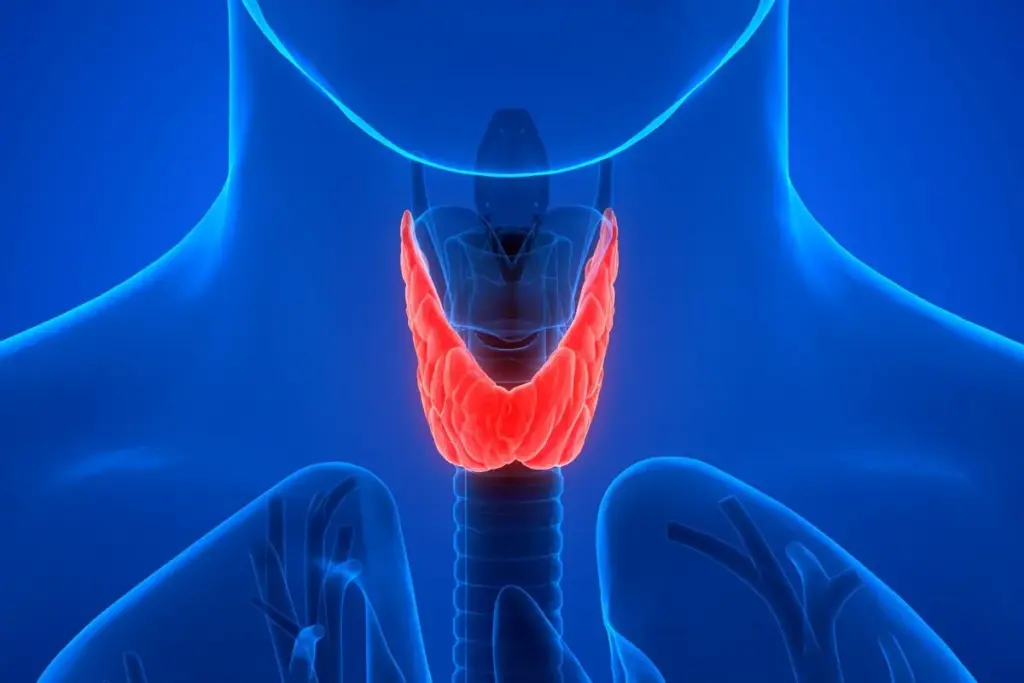
Understanding the Thyroid Gland and Its Functions
The thyroid gland is small but very important. It makes thyroid hormones. These hormones help control our metabolism, energy, and health.
The Role of Thyroid Hormones in Metabolism
Thyroid hormones are key for our metabolism. They help us use energy and control our weight. When they’re balanced, our body works well. But, if they’re off, we can get sick.
For example, during pregnancy, we need more thyroid hormones. This is because the mother and baby need more energy. It shows how important the gland is for big changes in our body.
How Thyroid Hormones Affect Body Systems
Thyroid hormones affect many parts of our body. They help our heart, brain, and reproductive system work right. For instance, they help our mood and brain function.
They also keep our heart healthy. If they’re not right, we might have heart problems. This includes irregular heartbeats or blood pressure changes.
Thyroid hormones are not just regulators of metabolism; they are essential for the overall homeostasis of the body, influencing nearly every organ and system.
- Regulate metabolism and energy levels
- Influence heart rate and cardiovascular health
- Affect brain function and neurological health
- Play a critical role in reproductive health
In summary, the thyroid gland and its hormones are key for our health. Knowing how they work is very important. This is true for people who have had or might have thyroid surgery.
Common Reasons for Thyroidectomy
Thyroidectomy is needed when thyroid issues harm a person’s health. The thyroid gland controls metabolism, energy, and hormones. Certain problems with this gland may require surgery.
Thyroid Cancer and Malignancies
Thyroid cancer is a main reason for thyroidectomy. There are four main types: papillary, follicular, medullary, and anaplastic. Doctors use biopsies to diagnose and surgery to remove the gland to stop cancer spread.
A study in the Journal of Clinical Endocrinology & Metabolism shows surgery for thyroid cancer has improved. It aims to reduce harm while keeping cancer under control. This shows the need for skilled surgeons in treating thyroid cancer.
|
Type of Thyroid Cancer |
Characteristics |
Treatment Approach |
|---|---|---|
|
Papillary Thyroid Cancer |
Most common type, often slow-growing |
Surgery, possibly followed by radioactive iodine therapy |
|
Follicular Thyroid Cancer |
May spread through blood vessels |
Surgery, with or without radioactive iodine therapy |
|
Medullary Thyroid Cancer |
Originates from parafollicular cells |
Surgery, with genetic testing recommended |
Hyperthyroidism and Graves’ Disease
Hyperthyroidism means the thyroid gland is too active. Graves’ disease, an autoimmune disorder, often causes this. If medicine doesn’t work or can’t be taken, surgery might be needed.
“Graves’ disease is the most common cause of hyperthyroidism, and thyroidectomy is considered for patients with severe symptoms or those who cannot be managed with antithyroid medications.”
— American Thyroid Association
Graves’ disease needs careful management, even more so in pregnant women. It can affect both the mother and the fetus.
Large Goiters and Nodules
Large goiters and nodules can cause discomfort and breathing problems. Surgery is considered if these issues are severe or if cancer is suspected.
Deciding on surgery for goiters or nodules depends on their size, symptoms, and biopsy results. Surgery can help relieve symptoms and improve life quality.
Types of Thyroid Removal Surgery
There are different ways to remove the thyroid gland, each with its own benefits. The right choice depends on the patient’s condition, the thyroid issue, and the surgeon’s opinion.
Total Thyroidectomy vs. Partial Thyroidectomy
Total thyroidectomy removes the whole gland. It’s often chosen for thyroid cancer, big goiters, or severe hyperthyroidism. Recent data shows it’s used in about 89% of cases.
Partial thyroidectomy removes just the affected part. It’s used when the disease is in one area and some thyroid function needs to be kept.
Key differences between total and partial thyroidectomy include:
- The extent of gland removal
- Indications for the procedure
- Potential impact on thyroid function post-surgery
Minimally Invasive Thyroidectomy Techniques
Minimally invasive techniques are becoming more popular. They promise less pain and quicker healing. These methods use small incisions and advanced tools for precise surgery.
“Minimally invasive thyroid surgery represents a significant advancement in the field, promising less discomfort and a faster return to normal activities.” -An Endocrine Surgeon
Thyroid Lobectomy Procedures
Thyroid lobectomy removes one lobe of the gland. It’s for patients with a nodule or tumor in one lobe. It’s a choice for those wanting to keep thyroid function or avoid hormone therapy.
The choice between these surgeries depends on many factors. These include the patient’s health, the thyroid condition, and the surgeon’s skill.
The Thyroidectomy Procedure: What to Expect
If you’re facing a thyroidectomy, knowing what to expect is key. We’ll guide you through the process. This will help ease your concerns and prepare you well.
Pre-Surgical Preparation
Preparation is essential before a thyroidectomy. High-volume surgeons can lower complication rates by 40%. This shows the importance of choosing the right team.
Preparation includes:
- A thorough medical check to assess health and risks.
- Imaging tests like ultrasound or CT scans to see the thyroid gland details.
- Blood tests to check thyroid function and health indicators.
- Adjusting medications if needed to prepare the thyroid for surgery.
- Education on recovery and home preparation.
During the Surgery
The thyroidectomy procedure removes the thyroid gland, either partially or fully. It’s done under general anesthesia for comfort. The surgeon makes a neck incision, and the extent of removal varies.
Minimally invasive techniques are used to reduce scarring and aid healing.
Immediate Post-Operative Care
After surgery, patients are watched in a recovery area for hours. Pain management is a top priority, and patients learn how to manage pain at home. It’s important to watch for signs of infection or complications like swallowing or breathing issues.
A follow-up appointment is set within a couple of weeks to check healing progress.
Understanding the thyroidectomy procedure and recovery helps patients prepare. With a skilled surgical team, the outcome is better, and the transition to post-surgery life is smoother.
Immediate Physical Changes After Thyroidectomy
After a thyroidectomy, patients see many changes right away. These changes can affect their health and daily life. They can be mild or serious.
Voice Changes and Throat Discomfort
Voice changes are common after thyroid surgery. Some people might sound hoarse or raspy. This is because the thyroid gland is close to the vocal cords.
Throat discomfort is also common. Patients might feel like there’s a lump in their throat or pain when swallowing. About 10% of patients might have nerve damage, but most recover fully.
Neck Appearance and Scarring
The neck can look different after surgery. Swelling and bruising are common at first. The swelling goes down, but some scars might stay.
Scars can worry patients. But, doctors use new methods to make scars smaller. Talking to a surgeon about these options can help.
Initial Energy Levels and Metabolism
Thyroid surgery changes how the body uses energy. Patients might feel tired at first. This is because their thyroid hormone levels are changing.
Patients need to adjust their lifestyle after surgery. They might need to eat differently and exercise more. Hormone replacement therapy helps get their metabolism back to normal.
Knowing about these changes helps patients prepare for life after surgery. While it takes time to adjust, many people live happy and active lives after recovery.
Hormone Replacement Therapy Following Thyroid Removal
After a thyroidectomy, hormone replacement therapy is key. The thyroid gland controls metabolism and energy. Without it, patients need lifelong hormone therapy to stay balanced.
Understanding Levothyroxine Treatment
Levothyroxine is a synthetic thyroid hormone, often given to thyroidectomy patients. It replaces the hormone the thyroid can’t make. This helps manage metabolism and energy. Levothyroxine is taken orally, once a day, on an empty stomach, for better absorption.
The goal is to keep thyroid hormone levels normal. This helps reduce hypothyroidism symptoms and improves health.
Finding the Right Dosage
Finding the right levothyroxine dosage is important. It depends on age, weight, health conditions, and why the thyroid was removed. Regular blood tests check hormone levels and adjust the dosage as needed.
This process needs patience and close doctor monitoring. It ensures the dosage is just right.
Alternative Thyroid Medications
Levothyroxine is the most common hormone replacement after thyroidectomy. But, there are other options like liothyronine and natural desiccated thyroid (NDT) extracts. Liothyronine is sometimes used with levothyroxine for patients with ongoing symptoms.
NDT extracts, from animal thyroid glands, have T4 and T3. Some patients prefer them for better symptom management. The choice depends on the patient’s needs and the doctor’s advice.
Managing Life Without a Thyroid Gland
Living without a thyroid gland is more than just taking medicine. It’s a big change in lifestyle. You need to adjust your daily routine, diet, and how you exercise.
Daily Medication Routines
After losing your thyroid, you’ll need synthetic hormones to replace the missing ones. It’s important to take your medicine at the same time every day. This helps your body absorb it better.
Working with your doctor to find the right dose is key. They’ll check your hormone levels with blood tests. Following your medication schedule is critical for keeping your hormones balanced.
Dietary Considerations
Your diet is very important when you don’t have a thyroid gland. There’s no special “thyroid diet,” but some foods can affect your medicine. Foods high in iodine, for example, can change your hormone levels. It’s important to eat a balanced diet with the right nutrients.
- Eat foods rich in selenium, zinc, and iron to help your thyroid.
- Watch out for soy and soy products, as they can affect how your medicine works.
- Avoid too much broccoli and cabbage, as they can harm your thyroid in large amounts.
Exercise and Physical Activity Adjustments
Exercise is great for your health, even without a thyroid gland. It helps with weight, mood, and energy, which can be hard to manage without thyroid hormones.
But, you should listen to your body and adjust your workout plan. Some people might need to do less based on how they feel. Talking to a doctor or fitness expert can help you make a plan that’s right for you.
Dealing with life without a thyroid gland can be tough, but it’s doable. With the right medicine, diet, and exercise, you can live a happy and active life. The number of people with thyroid cancer is expected to go up by nearly 30% by 2040. This shows how important it is to take care of your thyroid health.
Potential Complications of Thyroidectomy
Thyroidectomy is a common treatment for thyroid issues, but it comes with risks. Like any major surgery, there are complications to be aware of. This knowledge helps patients make informed decisions about their health.
Recurrent Laryngeal Nerve Injury
One major risk is injury to the recurrent laryngeal nerve. This nerve controls the vocal cords. Damage can lead to voice changes or even paralysis. Research shows this risk is about 10% of patients according to recent research.
We use advanced techniques and neuromonitoring to protect this nerve. This helps reduce the risk of injury.
Hypocalcemia and Parathyroid Issues
Hypocalcemia, or low calcium, is another risk. It can happen if the parathyroid glands are damaged or removed. Studies show permanent hypocalcemia affects up to 2% of patients.
To avoid this, we try to save the parathyroid glands. We also watch for signs of hypocalcemia after surgery. If needed, we provide calcium supplements.
Infection and Bleeding Risks
Thyroidectomy carries risks of infection and bleeding. We follow strict sterile procedures and use advanced methods to control bleeding. We teach patients to recognize signs of infection and bleeding.
This way, they can get help quickly if problems arise.
Psychological Impacts
The emotional effects of thyroidectomy should not be ignored. The surgery and hormone therapy can affect patients’ mental health. We offer counseling and support to help them adjust.
In summary, thyroidectomy comes with risks, but understanding them can help. Choosing an experienced team and following care instructions can improve outcomes. This way, patients can have a successful recovery.
Long-term Health Monitoring After Thyroid Removal
After having your thyroid gland removed, it’s important to keep an eye on your health. Regular check-ups and screenings are key. This ensures your treatment plan is working and makes any needed changes.
Regular Blood Tests and Hormone Level Checks
Checking hormone levels through blood tests is a big part of long-term care. These tests help make sure your thyroid hormone medication is right. We suggest getting hormone levels checked at least once a year. But, this might change based on your health.
Key aspects of blood tests include:
- Checking TSH (Thyroid-Stimulating Hormone) levels to ensure they are within the normal range.
- Monitoring free T4 and free T3 levels to assess the adequacy of thyroid hormone replacement.
Signs of Medication Adjustment Needs
It’s important for patients to know when they might need a medication change. Feeling tired, gaining or losing weight, or mood swings could mean it’s time to adjust your medication. We help patients spot these signs and adjust their treatment as needed.
Common signs that may require medication adjustment include:
- Persistent fatigue or weakness.
- Unexplained weight gain or loss.
- Mood changes, such as depression or anxiety.
Follow-up Cancer Surveillance (When Applicable)
If you had thyroid cancer, keeping an eye on it is very important. This might mean regular ultrasounds, blood tests for tumor markers, and other tests as advised by our specialists.
By being proactive with regular monitoring and care, patients can live well after thyroid surgery. We’re dedicated to supporting our patients every step of the way.
Life Expectancy After Thyroid Removal
Life expectancy after thyroidectomy depends on several factors. These include the condition that led to the surgery. We will look at the outcomes for different conditions and what affects long-term health. This will help patients understand their future better.
Statistical Outcomes for Different Conditions
Outcomes after thyroidectomy vary by condition. For example, those with thyroid cancer often have a good prognosis. They have high survival rates.
- Thyroid Cancer: Research shows that the 10-year survival rate for thyroid cancer patients is over 90% after surgery.
- Hyperthyroidism: Patients treated for hyperthyroidism see a big improvement in their quality of life. Their life expectancy is not greatly affected by the surgery.
- Benign Conditions: For those with benign conditions like large goiters or nodules, surgery can relieve symptoms. Their life expectancy is usually not affected.
Factors Affecting Long-term Prognosis
Several factors can impact long-term health after thyroidectomy. These include:
- Underlying Health Conditions: Existing health issues can affect overall health and life expectancy.
- Surgical Complications: Issues during or after surgery, like nerve injury or low calcium, can impact long-term health.
- Adherence to Medication: For those needing hormone replacement, sticking to the medication is key for health and preventing problems.
- Regular Follow-Up: Regular check-ups with healthcare providers are vital for monitoring health and adjusting treatment as needed.
By understanding these factors and staying proactive about health, patients can improve their long-term outlook after thyroidectomy.
Choosing the Right Thyroidectomy Surgeon
Thyroidectomy is a common surgery that needs a skilled surgeon for the best results. The right surgeon can make a big difference in your surgery’s success. It’s important to choose wisely.
The Importance of Surgical Volume and Experience
Studies show that experienced surgeons can cut complication rates by up to 40%. This highlights the need for a surgeon who does many thyroidectomies. Experience isn’t just about the number of surgeries. It’s also about handling surprises during surgery.
When looking at a surgeon’s credentials, consider these points:
- The number of thyroidectomy procedures they perform annually
- Their complication rates compared to national averages
- Their experience with cases similar to yours (e.g., thyroid cancer, large goiters)
Questions to Ask Your Surgeon
It’s vital to ask the right questions when you first meet your surgeon. Some important questions include:
- What is your experience with thyroid surgery, and how many procedures do you perform each year?
- What are your complication rates, and how do they compare to other surgeons?
- What approach do you take to thyroidectomy, and are there any alternative treatments we should consider?
These questions help you understand the surgeon’s skills and how they will care for you.
Finding Specialized Endocrine Surgeons
Endocrine surgeons focus on surgeries of the endocrine system, including thyroidectomy. They have extra training for these complex surgeries. To find a qualified endocrine surgeon, you can:
- Ask your primary care physician for a referral
- Check with professional organizations like the American Thyroid Association or the American Association of Endocrine Surgeons
- Research online, looking for surgeons with high ratings and positive patient reviews
By carefully choosing your thyroidectomy surgeon, you can greatly improve your surgery’s success and recovery.
Current Trends in Thyroid Surgery
The field of thyroid surgery is changing a lot. We’re moving towards more precise and less invasive treatments. New trends are shaping the future of thyroid surgery.
Less Radical Approaches When Appropriate
Now, guidelines suggest less radical thyroid surgery when it’s needed. This change is based on research showing less extensive surgery can work well. Less radical approaches help patients with low-risk thyroid cancers or benign conditions by removing less tissue.
A study shows less invasive thyroid surgery is becoming more common. This is thanks to better diagnostic tools and understanding of thyroid diseases.
Improved Diagnostic Accuracy
Our ability to diagnose thyroid nodules and cancers has improved a lot. Tools like fine-needle aspiration cytology (FNAC) and molecular marker analysis help make accurate diagnoses before surgery. Improved diagnostic accuracy helps choose the right surgery and avoid unnecessary ones.
Focus on Minimizing Patient Morbidity
Modern thyroid surgery aims to reduce patient discomfort. Methods like minimally invasive thyroidectomy and robotic-assisted surgery are used. These techniques reduce tissue damage, postoperative pain, and improve looks. Minimizing morbidity helps patients recover faster and live better after surgery.
“The goal of modern thyroid surgery is to achieve a balance between effective disease management and minimizing the impact on the patient’s quality of life.”
Thyroid surgery trends will keep changing with new research and technology. By using less radical methods, improving diagnosis, and focusing on patient comfort, we can improve outcomes and quality of life for patients.
Living Well After Thyroidectomy: Patient Stories
Thyroidectomy patients face a tough journey, but many stories show a life full of joy after surgery. It takes courage, support, and knowing how to manage your health.
Adjusting to the New Normal
After thyroidectomy, patients go through a tough adjustment. They must recover physically and adjust to a new routine with hormone therapy. Finding the right dosage of thyroid hormone medication is key to feeling better.
Keeping a journal of symptoms and medication effects is helpful. It helps patients understand what works best for them and talk better with doctors.
Strategies for Optimal Quality of Life
Living well after thyroidectomy needs a few key steps. Dietary adjustments are important, even without a thyroid gland. Regular exercise also helps keep energy up and health good.
- Maintaining a balanced diet
- Engaging in regular exercise
- Monitoring and managing stress
Support from loved ones and doctors is also key. Patients with support adjust better to their new life.
Support Groups and Resources
Connecting with others who’ve been through the same is very helpful. Support groups offer a place to share and get advice. Many groups also provide resources and info for life after thyroidectomy.
“Joining a support group was a turning point for me. Hearing others’ stories and sharing my own helped me feel less alone and more empowered to manage my condition.”
A thyroidectomy patient
By using these resources and being proactive about health, patients can live well after thyroidectomy. It’s about finding balance and using all the support available.
Future Developments in Thyroid Treatment
New research is leading to better thyroid treatments. As medical science grows, people with thyroid issues will get better care. This care will be more tailored to their needs.
Advances in Hormone Replacement Options
Hormone therapy is key for those without a thyroid. New developments include:
- New levothyroxine formulas that last longer and work better.
- Studies on combining hormones to match the body’s natural production.
- Work on dosing that fits each person’s genes and metabolism.
These changes aim to make hormone therapy more accurate and effective. This could greatly improve patients’ lives.
Emerging Surgical Techniques
Thyroid surgery is getting better too. New trends include:
- Less invasive surgeries that heal faster and leave less scar.
- Robotic surgery for more precise and flexible operations.
- Techniques to watch and protect important areas during surgery.
These new methods make surgery safer and more successful. Patients are getting better results from their surgeries.
Research on Thyroid Tissue Regeneration
Research on growing new thyroid tissue is exciting. Scientists are looking into:
- Stem cell treatments to grow or replace thyroid tissue.
- Creating thyroid tissue in labs using tissue engineering.
- Gene therapy to fix genetic problems in thyroid conditions.
These early research areas show great promise. They could lead to new treatments in the future.
The future of thyroid treatment looks bright. With ongoing research and new ideas, we’ll see better, more tailored treatments. These will be less invasive for patients with thyroid issues.
Conclusion: Embracing Life After Thyroid Removal
Life after thyroid removal can be tough, but with the right help, people can live well. We’ve looked at many parts of thyroidectomy, from the surgery to managing it long-term. We’ve also talked about new ways to treat thyroid issues.
Knowing these things helps patients deal with life after thyroidectomy better. With the right care, like hormone therapy and lifestyle changes, people can do great. We’ve shown how picking the right surgeon and staying up-to-date with thyroid surgery news is key.
With good care and support, people can have a great life after thyroid removal. We urge patients to take charge of their health. By using the latest in thyroid treatment, they can live a happy life after thyroidectomy. This makes life after thyroid removal a success story.
FAQ
What is thyroidectomy, and why is it performed?
Thyroidectomy is a surgery to remove part or all of the thyroid gland. It treats thyroid cancer, hyperthyroidism, large goiters, and nodules.
How does thyroid removal affect metabolism?
Removing the thyroid gland stops the main source of thyroid hormones. These hormones are key for metabolism. Patients need hormone replacement therapy to keep their metabolism healthy.
What are the different types of thyroidectomy procedures?
There are total and partial thyroidectomies. There are also minimally invasive and thyroid lobectomy procedures. Each has its own use and benefits.
What can I expect during and after thyroidectomy surgery?
Before surgery, patients prepare. During surgery, the thyroid gland is removed. After, they get care to manage any discomfort or complications.
How will thyroid removal affect my daily life?
After surgery, patients must manage their medication and diet. They also need to adjust their exercise and physical activity to stay healthy.
What are the possible complications of thyroidectomy?
Complications include nerve injury, low calcium, infection, and bleeding risks. There are also psychological impacts. Knowing these risks helps manage them.
How is hormone replacement therapy managed after thyroid removal?
Patients take levothyroxine. The dosage is adjusted based on blood tests to keep hormone levels right.
Can I live a normal life without a thyroid gland?
Yes, with the right hormone therapy and lifestyle changes, patients can live well. Regular health checks are key to staying healthy.
How does thyroidectomy impact life expectancy?
Life expectancy after surgery varies based on the reason for surgery. Outcomes differ for thyroid cancer, hyperthyroidism, and other conditions.
Why is choosing the right surgeon important for thyroidectomy?
The surgeon’s experience and skill greatly affect the surgery’s success. Patients should ask questions and look for specialized endocrine surgeons.
What are the current trends in thyroid surgery?
Trends include less invasive surgeries when possible. There’s also better diagnostic tools and a focus on reducing patient risks. This leads to better results for patients.
Are there any future developments in thyroid treatment?
Research is ongoing. It includes better hormone replacement options, new surgical techniques, and even regrowing thyroid tissue. These could lead to better treatments for thyroid conditions.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK563279/





