Last Updated on November 27, 2025 by Bilal Hasdemir

At Liv Hospital, we are committed to providing innovative and patient-centered care for ovarian cancer patients. Recent advancements in treatment options have significantly improved patient outcomes, offering a broader spectrum of effective therapies.
Effective treatment involves a range of drugs, including chemotherapy and targeted therapies. Medications such as paclitaxel, carboplatin, bevacizumab, and olaparib have shown efficacy in treating ovarian cancer. We emphasize the importance of personalized care, ensuring that each patient receives the most suitable treatment plan.
Our team is dedicated to delivering high-quality medical outcomes and implementing current academic protocols. By exploring the top cancer drugs used in ovarian cancer treatment, we aim to provide patients with the best possible care.
Key Takeaways
- Ovarian cancer treatment involves a range of effective drugs and therapies.
- Liv Hospital provides patient-centered care and innovative solutions.
- Chemotherapy and targeted therapies are key components of treatment.
- Personalized care ensures the best possible outcomes for patients.
- Recent advancements have significantly improved treatment options.
Ovarian Cancer Treatment Overview

Effective ovarian cancer treatment begins with understanding the disease’s various types and stages. Ovarian cancer is a complex disease that affects thousands of women worldwide, and its treatment requires a multifaceted approach.
Types and Stages of Ovarian Cancer
Ovarian cancer is categorized into several types based on the cells where the cancer begins. The most common type is epithelial ovarian cancer, which arises from the outer layer of the ovary. Other types include germ cell tumors and sex cord-stromal tumors. Understanding the type of ovarian cancer is crucial for determining the best treatment approach.
The stage of ovarian cancer is another critical factor in planning treatment. The FIGO (International Federation of Gynecology and Obstetrics) staging system is commonly used, ranging from Stage I (confined to the ovaries) to Stage IV (spread to distant organs).
Treatment Approaches and Protocols
The treatment of ovarian cancer depends on the type, stage, and the patient’s overall health. Surgery is often the first line of treatment, aiming to remove as much of the tumor as possible. Chemotherapy is commonly used before or after surgery to kill any remaining cancer cells.
Other treatment approaches include targeted therapy, which focuses on specific characteristics of cancer cells, and hormone therapy, which can be used for certain types of ovarian cancer. Clinical trials may also offer additional treatment options for some patients.
Cancer Drugs for Ovarian Cancer: Mechanisms and Classifications

Cancer drugs for ovarian cancer can be broadly classified into chemotherapy and targeted therapies, each with distinct mechanisms of action. Understanding these classifications is essential for determining the most effective treatment approach for ovarian cancer patients.
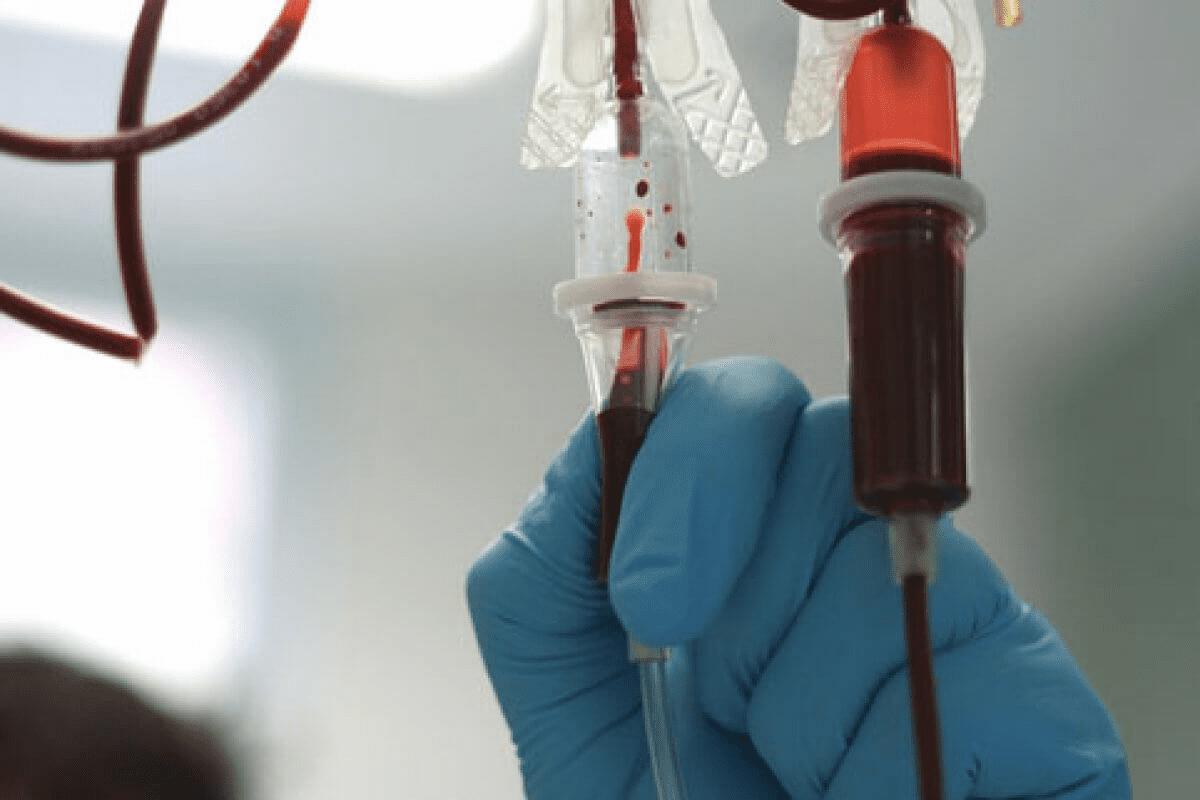
How Chemotherapy Targets Cancer Cells
Chemotherapy is a systemic treatment that uses drugs to kill cancer cells or stop them from dividing. We use chemotherapy drugs for ovarian cancer to target rapidly dividing cancer cells, thereby inhibiting tumor growth. Chemotherapy can be administered intravenously or orally, depending on the specific drug and treatment protocol.
The primary mechanism of chemotherapy involves interfering with the DNA replication process, thereby preventing cancer cells from proliferating. For instance, platinum-based chemotherapies, such as carboplatin, work by forming platinum-DNA adducts that damage DNA and trigger cell death.
Targeted Therapies vs. Traditional Chemotherapy
Targeted therapies differ from traditional chemotherapy in their specificity towards cancer cells. While chemotherapy affects both cancerous and healthy cells, targeted therapies are designed to target specific molecules involved in cancer growth and progression. For ovarian cancer, targeted therapies such as Bevacizumab (Avastin) and PARP inhibitors have shown significant promise.
Targeted therapies work by inhibiting specific pathways that are critical for cancer cell survival and proliferation. For example, Bevacizumab targets vascular endothelial growth factor (VEGF), thereby inhibiting angiogenesis, the process by which tumors form new blood vessels.
| Therapy Type | Mechanism of Action | Examples |
|---|---|---|
| Chemotherapy | Interferes with DNA replication, killing rapidly dividing cells | Carboplatin, Paclitaxel |
| Targeted Therapy | Targets specific molecules involved in cancer growth | Bevacizumab, Olaparib |
By understanding the mechanisms and classifications of cancer drugs for ovarian cancer, we can better appreciate the treatment options available and their potential benefits. As research continues to evolve, the development of new and more effective cancer drugs remains a critical focus in the fight against ovarian cancer.
Paclitaxel and Carboplatin: First-Line Combination Therapy
For many ovarian cancer patients, the combination of paclitaxel and carboplatin represents a standard and effective first-line treatment approach. This duo has been widely studied and is recognized for its synergistic effect in combating ovarian cancer.
Paclitaxel: Mechanism and Administration
Paclitaxel is a taxane that works by stabilizing microtubules, thereby inhibiting cell division and ultimately leading to cell death. It is typically administered intravenously, once every three weeks, though the exact dosing can vary based on patient-specific factors and treatment protocols.
We administer paclitaxel as part of a comprehensive treatment plan, carefully monitoring patients for potential side effects and adjusting dosages as necessary to optimize outcomes.
Carboplatin: Dosing and Efficacy
Carboplatin is a platinum-based chemotherapy drug that interferes with DNA replication, preventing cancer cells from reproducing. The dosing of carboplatin is often calculated using the Calvert formula, which takes into account the patient’s renal function to determine the appropriate dose.
Studies have shown that the combination of paclitaxel and carboplatin is highly effective in treating ovarian cancer, with significant improvements in survival rates. For more information on the duration of chemotherapy for stage 1 ovarian cancer, you can visit this resource.
| Treatment Component | Mechanism | Administration |
|---|---|---|
| Paclitaxel | Stabilizes microtubules, inhibiting cell division | Intravenous, every 3 weeks |
| Carboplatin | Interferes with DNA replication | Dose calculated using Calvert formula |
Managing Side Effects of Platinum-Based Therapy
While effective, platinum-based therapies like carboplatin can cause side effects, including nausea, fatigue, and hematologic toxicity. We take a proactive approach to managing these side effects, using supportive care measures to enhance patient comfort and compliance.
Key strategies for managing side effects include:
- Antiemetic medications to prevent nausea
- Growth factors to support blood cell production
- Regular monitoring of blood counts and renal function
By carefully managing side effects and tailoring treatment to individual patient needs, we can optimize the benefits of paclitaxel and carboplatin combination therapy.
Bevacizumab (Avastin): Targeting Tumor Blood Vessels
Bevacizumab (Avastin) is a targeted therapy that has shown considerable promise in treating advanced ovarian cancer. As an angiogenesis inhibitor, it works by blocking the formation of new blood vessels that tumors need to grow and metastasize.
How Bevacizumab Works as an Angiogenesis Inhibitor
Bevacizumab’s mechanism of action involves binding to vascular endothelial growth factor (VEGF), a protein that plays a critical role in angiogenesis. By inhibiting VEGF, bevacizumab effectively starves the tumor of the nutrients and oxygen it needs to proliferate. This targeted approach has been shown to improve outcomes in patients with advanced ovarian cancer.
Key benefits of bevacizumab include:
- Delayed tumor progression
- Improved overall survival in certain patient populations
- Potential for use in combination with chemotherapy regimens
Clinical Outcomes in Advanced Ovarian Cancer
Clinical trials have demonstrated the efficacy of bevacizumab in treating advanced ovarian cancer. Studies have shown that the addition of bevacizumab to standard chemotherapy regimens can significantly improve progression-free survival (PFS) and overall survival (OS) in certain patient groups.
Notable clinical outcomes include:
- Increased PFS in patients with high-risk disease
- Improved OS in patients with poor prognostic factors
- Effective management of symptoms and improved quality of life
Combination with Chemotherapy Regimens
Bevacizumab is often used in combination with chemotherapy to enhance its effectiveness. The combination of bevacizumab with paclitaxel and carboplatin has been shown to be particularly effective in treating advanced ovarian cancer.
Benefits of combination therapy include:
- Enhanced anti-tumor activity
- Potential for improved patient outcomes
- Flexibility in treatment planning
PARP Inhibitors: Olaparib, Niraparib, and Rucaparib
PARP inhibitors have revolutionized the treatment landscape for ovarian cancer, offering new hope to patients with specific genetic mutations. These drugs work by inhibiting the PARP enzyme, which is involved in DNA repair. In cancer cells with defective DNA repair mechanisms, such as those with BRCA1 and BRCA2 mutations, PARP inhibitors can cause cell death, thereby exerting their anti-tumor effect.
Olaparib (Lynparza): The First Approved PARP Inhibitor
Olaparib was the first PARP inhibitor to be approved for the treatment of ovarian cancer. It has shown significant efficacy in patients with BRCA mutations, improving progression-free survival (PFS) in both newly diagnosed and recurrent ovarian cancer.
Niraparib (Zejula) and Rucaparib (Rubraca): Comparing Efficacy
Niraparib and rucaparib are other PARP inhibitors that have been approved for ovarian cancer treatment. While all three drugs share a similar mechanism of action, there are differences in their efficacy and safety profiles. Niraparib has been shown to improve PFS in patients with recurrent ovarian cancer, regardless of their BRCA mutation status. Rucaparib has also demonstrated efficacy in treating ovarian cancer, particularly in patients with BRCA mutations.
Genetic Testing and BRCA Mutations
Genetic testing for BRCA1 and BRCA2 mutations is crucial in identifying patients who are most likely to benefit from PARP inhibitors. Patients with these mutations have impaired DNA repair mechanisms, making their cancer cells more susceptible to PARP inhibition.
To better understand the differences between olaparib, niraparib, and rucaparib, let’s examine their key characteristics:
| PARP Inhibitor | Approval Status | Efficacy in BRCA Mutations | Notable Side Effects |
|---|---|---|---|
| Olaparib (Lynparza) | Approved for first-line maintenance and recurrent ovarian cancer | Significant improvement in PFS | Nausea, fatigue, anemia |
| Niraparib (Zejula) | Approved for maintenance treatment of recurrent ovarian cancer | Improves PFS regardless of BRCA status | Thrombocytopenia, nausea, anemia |
| Rucaparib (Rubraca) | Approved for treatment of recurrent ovarian cancer | Significant efficacy in BRCA mutation carriers | Liver enzyme elevations, nausea, fatigue |
We have discussed the role of PARP inhibitors in ovarian cancer treatment, highlighting their mechanism, efficacy, and the importance of genetic testing for BRCA mutations. By understanding the differences between olaparib, niraparib, and rucaparib, healthcare providers can make informed decisions about the most appropriate treatment for their patients.
Oral Etoposide: Maintenance Therapy After Taxane Treatment
Oral etoposide has emerged as a viable maintenance therapy option for ovarian cancer patients following taxane treatment. This approach has garnered significant attention due to its potential to improve survival outcomes.
Research on Survival Outcomes
Recent studies have investigated the efficacy of oral etoposide as a maintenance therapy, showing promising results in terms of survival benefits. A key study published in a reputable oncology journal found that patients receiving oral etoposide after taxane treatment experienced improved progression-free survival rates.
“The use of oral etoposide as maintenance therapy represents a significant advancement in the treatment of ovarian cancer, offering patients an additional option to manage their disease.”
The data from various clinical trials suggest that oral etoposide can be an effective maintenance therapy, enhancing the overall treatment protocol for ovarian cancer patients.
Dosing Protocols and Administration
The administration of oral etoposide involves specific dosing protocols to maximize its efficacy while minimizing side effects. Typically, the dosage is adjusted based on patient response and tolerance.
| Dosing Protocol | Administration Schedule | Patient Monitoring |
|---|---|---|
| 50 mg/m² daily for 21 days | Every 28 days | Regular blood counts and toxicity assessment |
| 100 mg/m² daily for 14 days | Every 21 days | Regular assessment of response and side effects |
Patient Selection for Maintenance Therapy
Selecting the appropriate patients for oral etoposide maintenance therapy is crucial. Factors such as previous treatment response, overall health, and specific genetic markers are considered.
Key considerations include:
- Previous response to taxane treatment
- Presence of BRCA mutations
- Patient’s overall health and performance status
By carefully evaluating these factors, healthcare providers can identify patients who are most likely to benefit from oral etoposide maintenance therapy.
Doxorubicin and Topotecan: Second-Line Treatment Options
Ovarian cancer treatment often involves multiple lines of therapy, with doxorubicin and topotecan being key second-line choices. When initial treatments fail or the disease recurs, these chemotherapy drugs offer alternative approaches to managing the condition.
Liposomal Doxorubicin (Doxil): Reducing Toxicity
Liposomal doxorubicin, known by its brand name Doxil, is a formulation of doxorubicin encapsulated in liposomes. This design reduces the drug’s toxicity while maintaining its efficacy against ovarian cancer cells. By minimizing the free drug available to cause harm, liposomal doxorubicin decreases the risk of side effects such as cardiotoxicity and myelosuppression.
The use of liposomal doxorubicin allows for higher cumulative doses, potentially improving treatment outcomes for patients with recurrent ovarian cancer. Its administration is typically done intravenously, and the dosing schedule can vary based on the patient’s previous treatments and overall health.
Topotecan: Mechanism and Administration
Topotecan is a topoisomerase I inhibitor that works by interfering with the function of an enzyme that cancer cells need to divide and grow. It is administered intravenously, usually over 30 minutes, once daily for five consecutive days, every three weeks. The dosage may be adjusted based on the patient’s tolerance and response to the treatment.
Topotecan is recognized for its efficacy in treating recurrent ovarian cancer, particularly in patients who have previously received platinum-based chemotherapy. Its side effect profile includes myelosuppression, fatigue, and gastrointestinal symptoms, which are managed with supportive care measures.
Managing Recurrent Disease
Managing recurrent ovarian cancer requires a personalized approach, taking into account the patient’s previous treatments, the duration of their response, and their overall health. Doxorubicin and topotecan are valuable options in this context, offering different mechanisms of action that can be effective in controlling the disease.
The choice between doxorubicin and topotecan depends on various factors, including the patient’s previous exposure to anthracyclines or topoisomerase inhibitors, their renal function, and their preferences regarding potential side effects. Effective management of recurrent disease also involves supportive care, including symptom control and addressing any treatment-related toxicities.
By understanding the benefits and challenges associated with doxorubicin and topotecan, healthcare providers can tailor treatment plans to meet the individual needs of patients with recurrent ovarian cancer, improving their quality of life and potentially extending their survival.
Gemcitabine and Docetaxel: Alternative Chemotherapy Approaches
For patients with ovarian cancer, alternative chemotherapy options are crucial when standard treatments fail. We explore the role of gemcitabine and docetaxel in providing effective treatment alternatives.
Efficacy in Platinum-Resistant Disease
Gemcitabine has shown significant efficacy in treating platinum-resistant ovarian cancer. Its ability to inhibit DNA synthesis makes it a valuable option for patients who have developed resistance to platinum-based therapies.
In clinical studies, gemcitabine has demonstrated improved progression-free survival rates in patients with recurrent ovarian cancer. We consider gemcitabine a viable treatment choice for those with limited options.
Docetaxel as an Alternative to Paclitaxel
Docetaxel is another chemotherapy agent used in ovarian cancer treatment, particularly as an alternative to paclitaxel. Its mechanism of action involves inhibiting cell division, making it effective against rapidly dividing cancer cells.
Clinical trials have shown that docetaxel is comparable to paclitaxel in terms of efficacy, offering a valuable alternative for patients who experience adverse reactions or develop resistance to paclitaxel. We recommend considering docetaxel for patients who require a change in their chemotherapy regimen.
By understanding the benefits and efficacy of gemcitabine and docetaxel, we can provide ovarian cancer patients with more personalized and effective treatment plans.
Conclusion: Personalized Treatment Approaches for Ovarian Cancer
Personalized treatment approaches have revolutionized ovarian cancer care, enabling healthcare providers to tailor treatment plans to individual patient needs. At Liv Hospital, we recognize the importance of customized care in improving patient outcomes.
Our discussion has highlighted various cancer drugs for ovarian cancer, including Paclitaxel, Carboplatin, Bevacizumab, and PARP inhibitors like Olaparib and Niraparib. These treatments, often used in combination, have shown significant efficacy in managing ovarian cancer.
By understanding the unique characteristics of each patient’s cancer, we can develop targeted treatment strategies that maximize effectiveness while minimizing side effects. This personalized approach to ovarian cancer treatment has been shown to improve survival rates and quality of life for patients.
As we continue to advance in ovarian cancer treatment, our focus remains on providing high-quality, patient-centered care that addresses the complex needs of individuals affected by this disease.
FAQ
What are the most common ovarian cancer treatment drugs?
The most common ovarian cancer treatment drugs include paclitaxel, carboplatin, bevacizumab, olaparib, niraparib, and rucaparib, among others. These medications are used in various combinations and protocols to treat different types and stages of ovarian cancer.
How do chemotherapy drugs work in treating ovarian cancer?
Chemotherapy drugs target rapidly dividing cancer cells, inhibiting their growth and proliferation. In ovarian cancer, chemotherapy is often used in combination with other treatments, such as surgery and targeted therapies, to achieve optimal outcomes.
What is the role of targeted therapies in ovarian cancer treatment?
Targeted therapies, such as bevacizumab and PARP inhibitors, specifically target molecular mechanisms involved in ovarian cancer progression. These treatments can help improve outcomes and reduce side effects compared to traditional chemotherapy.
What are the benefits and side effects of paclitaxel and carboplatin?
Paclitaxel and carboplatin are commonly used as first-line combination therapy for ovarian cancer. While effective, they can cause side effects such as hair loss, fatigue, and neuropathy. Managing these side effects is crucial to ensure optimal treatment outcomes.
How does bevacizumab work in treating ovarian cancer?
Bevacizumab is an angiogenesis inhibitor that targets tumor blood vessels, reducing the supply of oxygen and nutrients to cancer cells. This can help slow disease progression and improve treatment outcomes in advanced ovarian cancer.
What are PARP inhibitors, and how are they used in ovarian cancer treatment?
PARP inhibitors, such as olaparib, niraparib, and rucaparib, are targeted therapies that exploit defects in DNA repair mechanisms in cancer cells. They are used to treat ovarian cancer, particularly in patients with BRCA mutations or other homologous recombination deficiencies.
What is the role of genetic testing in ovarian cancer treatment?
Genetic testing, including BRCA mutation testing, plays a crucial role in identifying patients who may benefit from targeted therapies, such as PARP inhibitors. This information helps guide treatment decisions and personalize care.
What are the alternative chemotherapy approaches for ovarian cancer?
Alternative chemotherapy approaches, such as gemcitabine and docetaxel, may be used in patients who are resistant to or intolerant of first-line treatments. These options can help manage disease progression and improve quality of life.
How is ovarian cancer treatment personalized?
Ovarian cancer treatment is personalized based on individual patient characteristics, including tumor type, stage, and genetic profile. This tailored approach helps optimize treatment outcomes and minimize side effects.
What are the benefits of oral chemotherapy pills for ovarian cancer?
Oral chemotherapy pills, such as etoposide, offer a convenient and flexible treatment option for ovarian cancer patients. They can be used as maintenance therapy or in combination with other treatments to improve outcomes.
What are the chemotherapy tablets used for ovarian cancer?
Chemotherapy tablets, including etoposide and topotecan, are used to treat ovarian cancer. These oral medications can be used in various treatment protocols, including maintenance therapy and second-line treatment.