Last Updated on November 18, 2025 by Ugurkan Demir

At Liv Hospital, we know how complex shoulder joint diseases can be. We offer different surgical options. Total shoulder arthroplasty and reverse shoulder arthroplasty are two main surgeries for severe shoulder damage.
Both surgeries aim to ease pain and improve function. But they have big differences in how they’re done and who they’re for. Total shoulder arthroplasty is best for those with arthritis and a healthy rotator cuff. It tries to keep the shoulder’s natural shape.
Reverse shoulder arthroplasty is for patients with torn rotator cuffs that can’t be fixed. It changes the shoulder’s structure to use the deltoid muscle instead.
Key Takeaways
- Two main surgeries exist for severe shoulder joint disease: orth and reverse shoulder arthroplasty.
- Total shoulder arthroplasty is for patients with arthritis and a healthy rotator cuff.
- Reverse shoulder arthroplasty is for those with torn rotator cuffs that can’t be fixed.
- The right surgery depends on the patient’s condition and body.
- Liv Hospital is dedicated to advanced, patient-centered orthopedic care.
Understanding Shoulder Replacement Surgery
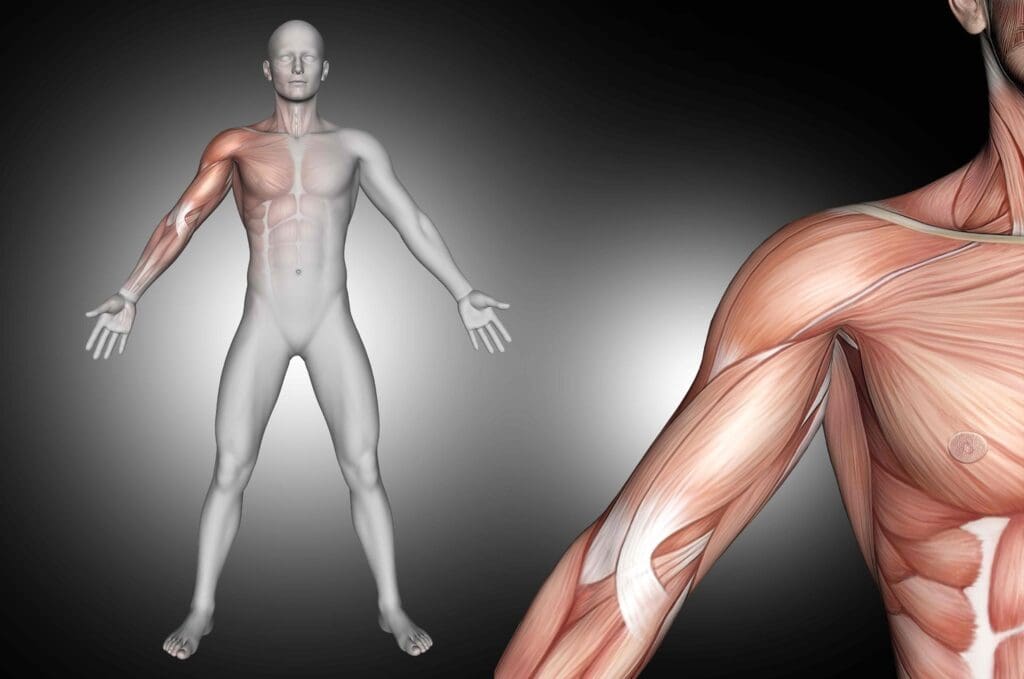
Exploring shoulder replacement surgery starts with understanding the shoulder joint. It’s made up of bones, muscles, tendons, and ligaments. These parts work together to allow for a wide range of motion.
The Anatomy of the Shoulder Joint
The shoulder joint, or glenohumeral joint, is a ball-and-socket joint. It connects the humerus (upper arm bone) to the scapula (shoulder blade). Surrounding it are muscles, like the rotator cuff, which help with stability and movement.
The rotator cuff muscles and others allow the shoulder to move in many directions. This makes it very mobile. But, it also makes the shoulder more prone to injuries and degenerative conditions.
When Shoulder Replacement Becomes Necessary
Shoulder replacement surgery is needed when the joint is severely damaged. This can happen due to osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis. These conditions cause pain, stiffness, and limited mobility, affecting a person’s quality of life.
In some cases, surgery may be needed for severe fractures or failed previous surgeries. The choice to have surgery is made after trying other treatments.
| Condition | Description | Treatment Outcome |
|---|---|---|
| Osteoarthritis | Wear and tear of the joint cartilage | Pain relief, improved mobility |
| Rheumatoid Arthritis | Autoimmune inflammation of the joint | Reduced inflammation, improved function |
| Post-Traumatic Arthritis | Arthritis following a traumatic injury | Restoration of joint function, pain reduction |
Evolution of Shoulder Arthroplasty Techniques
Shoulder arthroplasty techniques have improved a lot over time. Advances include better implant design, materials, and surgical methods. Traditional total shoulder arthroplasty (TSA) replaces the damaged joint with prosthetic parts that match the natural anatomy.
Recently, reverse total shoulder arthroplasty (RTSA) was developed for cases where the rotator cuff is badly damaged. RTSA changes the shoulder’s anatomy to improve stability and function for certain types of damage.
The field of shoulder arthroplasty is always evolving. Ongoing research aims to improve outcomes and offer more treatment options for shoulder disorders.
What is Total Shoulder Arthroplasty (TSA)?
For those with severe shoulder pain from arthritis, Total Shoulder Arthroplasty (TSA) is a hopeful solution. This surgery replaces the damaged joint with artificial parts. It helps ease pain and improve function.
Anatomical Design and Components
TSA aims to match the natural shoulder joint. It usually replaces both the ball and socket with artificial parts. The ball is often metal, and the socket can be plastic or metal. The choice depends on the patient’s needs and the surgeon’s choice.
The key components of TSA include:
- Humeral stem: Holds the prosthetic ball to the bone
- Humeral head: Replaces the natural ball of the shoulder
- Glenoid component: Replaces the natural socket of the shoulder
How TSA Replicates Natural Shoulder Mechanics
TSA tries to mimic the shoulder’s natural movement. It places the artificial parts with great care. This helps patients move better and feel less pain.
“The goal of TSA is to restore the natural kinematics of the shoulder joint, allowing patients to perform daily activities with ease and minimal discomfort.”
Ideal Candidates for Traditional TSA
TSA is best for those with severe arthritis and a healthy rotator cuff. It’s for those who’ve tried other treatments without success. People with osteoarthritis, rheumatoid arthritis, or arthritis from injury might find relief with TSA.
| Condition | Description | Suitability for TSA |
|---|---|---|
| Osteoarthritis | Wear and tear of the joint cartilage | High |
| Rheumatoid Arthritis | Autoimmune disease causing joint inflammation | Moderate to High |
| Post-Traumatic Arthritis | Arthritis following a traumatic injury | Moderate to High |
What is Reverse Total Shoulder Arthroplasty?
Reverse Total Shoulder Arthroplasty (RTSA) is a new way to fix shoulders. It’s for people with complex shoulder problems. This method is different from traditional Total Shoulder Arthroplasty (TSA) and offers hope for those who can’t have TSA.
The Reversed Ball-and-Socket Design
The key feature of Reverse TSA is its ball-and-socket design. Unlike the natural shoulder or TSA, the ball is on the scapula and the socket on the humerus. This change affects how the shoulder works.
How Reverse TSA Changes Shoulder Biomechanics
Reverse TSA changes how forces move in the shoulder. It lets the deltoid muscle help, improving movement and stability. This is good for people with certain shoulder problems.
This method helps those with irreparable rotator cuff tears. It uses the deltoid to improve shoulder function. This is great for those who have lost a lot of rotator cuff function.
The Role of the Deltoid Muscle in Reverse TSA
In Reverse TSA, the deltoid muscle is key. Without a working rotator cuff, the deltoid does the heavy lifting. This design helps the deltoid muscle make the shoulder move better.
| Aspect | Traditional TSA | Reverse TSA |
|---|---|---|
| Ball-and-Socket Configuration | Anatomical (Ball on Humerus) | Reversed (Ball on Scapula) |
| Primary Indications | Osteoarthritis, Avascular Necrosis | Cuff Tear Arthropathy, Massive Rotator Cuff Tears |
| Role of Deltoid Muscle | Secondary | Primary for Shoulder Mobility |
Knowing about Reverse TSA is important for doctors and patients. It helps in making the right choice for treatment. This leads to better care and results.
Total Shoulder Replacement vs Reverse: The 7 Key Differences
There are key differences between total shoulder replacement and reverse total shoulder arthroplasty. These differences are based on their design and how they work. Knowing these differences helps doctors choose the best surgery for each patient.
1. Anatomical Configuration
Total Shoulder Arthroplasty (TSA) replaces the damaged shoulder with an artificial one that looks like the real thing. On the other hand, Reverse Total Shoulder Arthroplasty changes the shoulder’s anatomy. It flips the ball and socket, affecting how the shoulder moves.
Key differences in anatomical configuration include:
- The positioning of the ball and socket components
- The design of the glenoid and humeral components
- The impact on surrounding soft tissues
2. Biomechanical Principles
The biomechanics of TSA and reverse TSA are different. TSA tries to keep the shoulder’s natural movement. Reverse TSA, on the other hand, uses the deltoid muscle to help with movement because the rotator cuff is weak.
The main biomechanical differences are:
- Dependence on the rotator cuff for stability
- Role of the deltoid muscle in shoulder movement
- Impact on joint stability and mobility
3. Surgical Technique Variations
The way TSA and reverse TSA are done differs because of their design and the problems they solve. Reverse TSA might need more exposure and special techniques for the glenoid and humerus.
4. Patient Selection Criteria
Choosing the right patient for TSA or reverse TSA is very important. The decision depends on the rotator cuff’s health, arthritis, and the patient’s overall health.
Key considerations for patient selection include:
- The presence and severity of rotator cuff tears
- The extent of glenohumeral arthritis
- The patient’s age, activity level, and expectations
Primary Indications for Traditional Total Shoulder Arthroplasty
Traditional total shoulder arthroplasty (TSA) is a proven treatment for many shoulder problems. It’s recommended for those with specific shoulder issues that haven’t gotten better with other treatments.
Osteoarthritis with Intact Rotator Cuff
Osteoarthritis is a disease that wears down joints, affecting life quality. If the rotator cuff is okay, TSA is often chosen. It fixes the shoulder’s anatomy, improving function and easing pain.
Research shows TSA works best for those with osteoarthritis and a healthy rotator cuff. It beats other shoulder replacement methods in these cases.
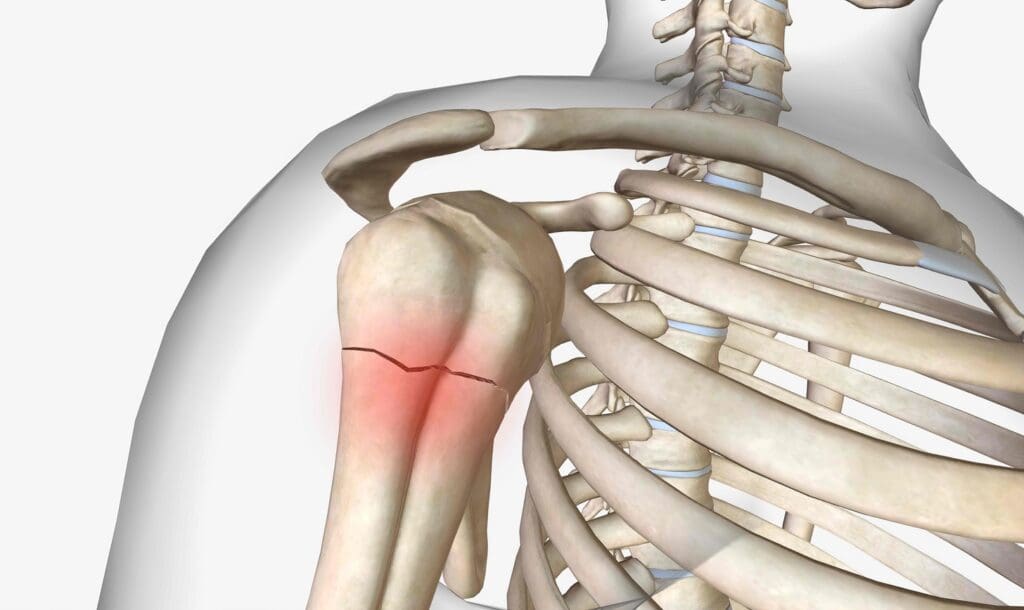
Post-Traumatic Arthritis
Post-traumatic arthritis happens after a shoulder injury, like a fracture. TSA is for those with this type of arthritis who are in pain and can’t move well. It aims to fix joint mechanics and ease pain.
“The use of traditional TSA in post-traumatic arthritis has been shown to provide significant improvements in pain and function, allowing patients to return to their daily activities.”
Avascular Necrosis
Avascular necrosis is when bone tissue dies from lack of blood. In the shoulder, it can cause the humeral head to collapse. TSA is a good option for advanced cases where other treatments have failed.
A study in the Journal of Shoulder and Elbow Surgery found TSA helps with pain and improves function in avascular necrosis patients.
Rheumatoid Arthritis (Early Stages)
Rheumatoid arthritis is an autoimmune disease that damages joints. Early on, TSA can be a good choice, even with significant damage but a healthy rotator cuff.
| Condition | Treatment Outcome | Key Benefits |
|---|---|---|
| Osteoarthritis with Intact Rotator Cuff | Improved function and pain reduction | Restores natural anatomy, effective pain relief |
| Post-Traumatic Arthritis | Significant pain relief and functional improvement | Restores joint mechanics, improves quality of life |
| Avascular Necrosis | Reliable pain relief and functional improvement | Effective for advanced cases, improves joint function |
| Rheumatoid Arthritis (Early Stages) | Effective in managing joint destruction | Preserves joint function, reduces pain |
We’ve looked at when traditional total shoulder arthroplasty is the best choice. It’s effective for many shoulder problems. Knowing this helps doctors pick the best treatment for their patients.
Primary Indications for Reverse Total Shoulder Replacement
Reverse Total Shoulder Arthroplasty has greatly helped patients with tough shoulder problems. It’s for those with severe rotator cuff damage or complex shoulder issues. These cases often can’t be fixed with regular shoulder surgery.
Rotator Cuff Tear Arthropathy
Rotator cuff tear arthropathy is a serious condition. It combines severe arthritis with a big rotator cuff tear. This causes a lot of pain and makes it hard to move the shoulder.
Research shows Reverse TSA can really help. It can ease pain and improve shoulder function for these patients.
Massive Irreparable Rotator Cuff Tears
Those with big rotator cuff tears often have chronic pain and can’t move their shoulder well. Reverse TSA is a good option for them. It can help improve shoulder function and lessen pain.
“Reverse shoulder arthroplasty has been shown to be effective in treating patients with massive rotator cuff tears, providing significant improvements in pain and function.”
Failed Previous Shoulder Replacement
If shoulder replacement surgery didn’t work out, Reverse TSA might be a second chance. It’s for those who had bad results or complications from their first surgery.
| Condition | Treatment Outcome with Reverse TSA |
|---|---|
| Rotator Cuff Tear Arthropathy | Significant pain relief and functional improvement |
| Massive Irreparable Rotator Cuff Tears | Restoration of shoulder function and pain reduction |
| Failed Previous Shoulder Replacement | Revision surgery with potentially better results |
Complex Proximal Humerus Fractures in Elderly Patients
Elderly patients with complex shoulder fractures face a tough treatment challenge. Reverse TSA is now a viable option. It allows for early movement and rehabilitation.
In summary, Reverse Total Shoulder Arthroplasty is key for treating complex shoulder issues. This includes rotator cuff tear arthropathy, big rotator cuff tears, failed shoulder replacements, and complex fractures in the elderly. Knowing these uses helps doctors choose the right treatment for patients, leading to better results.
The Surgical Procedure: What to Expect
Understanding shoulder replacement surgery is key. Knowing what happens during the procedure helps reduce anxiety. It also prepares patients for what’s to come.
Preoperative Preparation
Before TSA or reverse TSA, thorough preparation is needed. We check the patient’s health and any conditions that might affect surgery or recovery. Patients are advised to disclose all medications they are currently taking, as some may need to be adjusted or discontinued before the surgery.
We also do blood work and imaging studies. This helps us understand the patient’s shoulder anatomy and the extent of the condition.
“A well-prepared patient is a key factor in the success of shoulder replacement surgery.” – Orthopedic Surgeon
Traditional TSA Surgical Approach
The traditional TSA approach makes an incision to access the shoulder joint. The deltoid muscle is retracted or partially detached for exposure. The humeral head is then removed and replaced with a prosthetic component, and the glenoid is resurfaced with a glenoid component.
The surgical technique can vary based on the patient’s anatomy and the surgeon’s preference. The goal is to restore the shoulder joint’s natural mechanics.
Reverse TSA Surgical Approach
The reverse TSA approach is more complex due to the unique implant design. The procedure reverses the shoulder’s anatomy by placing the ball component on the glenoid and the socket component on the humerus. This reversal requires a thorough understanding of the shoulder biomechanics and precise surgical technique.
| Aspect | Traditional TSA | Reverse TSA |
|---|---|---|
| Surgical Approach | Deltoid retraction or partial detachment | Similar to traditional TSA, with additional considerations for the reversed anatomy |
| Component Placement | Humeral head replacement and glenoid resurfacing | Reversal of ball and socket components |
Immediate Post-Operative Care
After surgery, patients are monitored in the recovery room for any complications. Pain management is a priority, and we use various methods to ensure comfort.
Patients are advised to keep their arm in a sling to immobilize the shoulder and aid healing. We also start discussing rehabilitation, including physical therapy, for a smooth recovery.
By understanding the procedure and what to expect, patients can better prepare for their journey. This leads to a more successful outcome.
Recovery and Rehabilitation Comparison
Recovery and rehabilitation are key parts of the shoulder replacement journey. They differ between TSA and Reverse TSA. It’s important for patients to understand these differences for their post-operative care and rehabilitation.
Physical Therapy Protocols for Traditional TSA
For Traditional TSA, physical therapy starts soon after surgery. It focuses on gentle exercises to keep the shoulder flexible and strengthen the muscles. Early mobilization is key to avoid stiffness and aid healing.
As patients get better, therapy gets tougher. It aims to improve shoulder function and stability. The first phase of rehab for Traditional TSA lasts 6-12 weeks. During this time, patients do exercises tailored to their needs and progress. Following the therapy plan is essential for the best results.
Physical Therapy Protocols for Reverse TSA
Reverse TSA rehab focuses on stabilizing the shoulder and strengthening the deltoid muscle. The deltoid’s role is critical for Reverse TSA success. The deltoid’s function is key for the procedure’s success.
Therapy for Reverse TSA starts early, usually a few days after surgery. It includes exercises for range of motion, strengthening, and functional activities. Patients are closely monitored to adjust their rehab as needed.
Timeline for Return to Activities
The time to get back to normal activities varies between TSA and Reverse TSA. Traditional TSA patients can start with light activities in 3-6 months. Full recovery might take up to a year. Being patient and following rehab is important for the best outcome.
Reverse TSA recovery takes longer, with big improvements in 6-9 months. Full recovery can take up to a year or more, depending on individual factors and the procedure’s complexity.
Long-Term Activity Restrictions
Both TSA and Reverse TSA have long-term activity restrictions. These are to ensure the implant lasts long and the tissues stay healthy. High-impact activities are generally discouraged for patients with either type of shoulder replacement.
For Traditional TSA, avoid heavy lifting and repetitive overhead motions. For Reverse TSA, some activities that stress the implant or the deltoid should be avoided. Patients should follow their surgeon’s specific guidelines on activity levels and restrictions.
Complications and Risks: A Comparative Analysis
It’s important to know the possible complications and risks of Total Shoulder Arthroplasty (TSA) and Reverse TSA. Both surgeries help treat shoulder problems but have different risks.
Common Complications in Traditional TSA
Traditional TSA is usually successful but can have complications. These include:
- Rotator Cuff Failure: This is a common issue because the rotator cuff is key to TSA’s success.
- Implant Loosening: The implant can loosen over time, needing another surgery.
- Glenoid Wear: Wear on the glenoid can cause pain and less function.
Common Complications in Reverse TSA
Reverse TSA also has its own complications, such as:
- Dislocation: The reversed design can raise the risk of dislocation, mainly early on.
- Scapular Notching: This happens when the humeral component hits the scapula, causing pain and limited movement.
- Acromial Stress Fracture: The stress on the acromion can cause fractures.
Infection and Nerve Injury Risks in Both Procedures
Both TSA and Reverse TSA share risks common to surgeries, including:
- Infection: There’s a risk of infection with both, but we take careful steps to avoid it.
- Nerve Injury: Nerve injury is a risk with both, leading to numbness, weakness, or other symptoms.
Patients should talk to their healthcare provider about these risks. This helps them make a well-informed decision about their treatment.
Outcomes and Success Rates
When looking at Total Shoulder Arthroplasty (TSA) and reverse TSA, it’s key to check the outcomes and success rates. Knowing these details helps patients choose the best treatment for them.
Pain Relief Expectations
Both TSA and reverse TSA help a lot with pain for those with shoulder issues. More than 90% of patients see a big drop in pain after surgery. But, how much pain relief you get can depend on your condition and if there are any problems.
Functional Improvement Metrics
How well you can move your shoulder after surgery is very important. We use scores like the Constant-Murley and the American Shoulder and Elbow Surgeons (ASES) score to check this. Reverse TSA often shows big improvements in these scores, which is great for people with rotator cuff problems.
| Metric | TSA | Reverse TSA |
|---|---|---|
| Constant-Murley Score | 70-80 | 60-70 |
| ASES Score | 85-95 | 80-90 |
Patient Satisfaction Comparison
How happy patients are after surgery is a big sign of success. Both TSA and reverse TSA make most patients very happy, with satisfaction rates over 85%. What makes patients happy includes how much pain they feel, how well they can move, and if there are no big problems.
Longevity of Implants
How long implants last is important, mainly for younger people. Both TSA and reverse TSA implants last well, but how long they last can vary. At 10 years, studies show that 80% to 90% of implants are doing well for both procedures.
In summary, both TSA and reverse TSA have good results, with lots of pain relief, better movement, and high happiness rates. The right choice for you depends on your specific situation and what your shoulder needs.
Cost Considerations and Insurance Coverage
When thinking about shoulder replacement surgery, cost and insurance are key. Patients face a choice between total shoulder arthroplasty (TSA) and reverse total shoulder arthroplasty (reverse TSA). Knowing the costs is vital.
Comparative Costs of TSA vs Reverse TSA
The prices for TSA and reverse TSA differ a lot. Reverse TSA usually costs more because it’s more complex and needs special implants. The main reasons for the price gap are the implants, surgery time, and hospital stay. Research shows reverse TSA can be 10-20% pricier than TSA.
Insurance Coverage Considerations
Insurance for TSA and reverse TSA varies by provider. Most plans cover both, but how much they cover can vary. Patients should check their insurance and any costs they might have to pay out of pocket. Getting pre-approval and showing medical need is often needed.
- Check your insurance provider’s policy on TSA and reverse TSA.
- Understand the pre-approval process and required documentation.
- Be aware of any out-of-pocket expenses, including deductibles and co-pays.
Long-Term Economic Impact
Looking at TSA and reverse TSA costs, the long-term effects are important. Reverse TSA might cost more upfront but could save money later due to its durability. On the other hand, TSA might need more surgeries, which could even out the initial cost.
We suggest talking to your doctor and a financial advisor. They can help you choose the best option for your budget and health.
Conclusion: Making the Right Choice for Your Shoulder Condition
Choosing between Total Shoulder Arthroplasty (TSA) and Reverse Total Shoulder Arthroplasty can be tough. We’ve looked at the main differences and when to use each. This should help you decide.
Understanding your needs is key to making the right choice. TSA is best for those with osteoarthritis and a healthy rotator cuff. On the other hand, Reverse TSA is for those with a torn rotator cuff or a big tear that can’t be fixed.
Talking to a healthcare professional is very important. They will look at your shoulder, medical history, and how you live. This helps them suggest the best treatment. Knowing the differences between TSA and Reverse TSA helps you make a smart choice. It’s the first step to getting your shoulder moving better and feeling less pain.
FAQ
What is the main difference between total shoulder arthroplasty (TSA) and reverse total shoulder arthroplasty?
TSA mimics the natural shoulder joint. Reverse TSA flips this, with the ball on the scapula and the socket on the humerus.
What are the typical indications for traditional total shoulder arthroplasty?
TSA is for those with osteoarthritis, post-traumatic arthritis, avascular necrosis, or early rheumatoid arthritis. The rotator cuff must be intact.
When is reverse total shoulder arthroplasty preferred?
Reverse TSA is best for rotator cuff tears, massive tears, failed shoulder replacements, or complex fractures in the elderly.
How do the surgical approaches differ between TSA and reverse TSA?
TSA and reverse TSA start with a similar approach. But TSA needs precise anatomy, while reverse TSA focuses on the deltoid muscle and biomechanics.
What can I expect during recovery from TSA or reverse TSA?
Recovery includes a period of rest and physical therapy. TSA and reverse TSA have different recovery times. Reverse TSA might need a slower return to activities.
Are there different complications associated with TSA and reverse TSA?
Yes, TSA risks rotator cuff issues, while reverse TSA faces dislocation or scapular notching risks.
How do the outcomes and success rates compare between TSA and reverse TSA?
Both offer pain relief and improved function. TSA gives more natural movement, but reverse TSA is better for severe rotator cuff issues.
What are the cost considerations for TSA versus reverse TSA?
TSA and reverse TSA costs vary. Reverse TSA might be pricier due to specialized implants and techniques.
Will insurance cover the costs of TSA or reverse TSA?
Insurance coverage varies by plan and condition. Always check with your provider for details.
What is the longevity of TSA and reverse TSA implants?
Implant longevity depends on age, activity, and implant type. Modern implants aim for long-term use, but exact lifespans vary.
Can I undergo TSA or reverse TSA if I have had previous shoulder surgery?
Previous surgery doesn’t always mean you can’t have TSA or reverse TSA. It depends on the surgery type and current shoulder condition.
What is the role of physical therapy in the recovery from TSA or reverse TSA?
Physical therapy is key for both procedures. It helps regain motion, strength, and function. Therapy plans may differ between TSA and reverse TSA.
References
- Liu, H., Huang, C.-T., Yu, H., Wang, Y., Wang, D., & Long, Z. (2022). Total shoulder arthroplasty versus reverse total shoulder arthroplasty: Outcome comparison in osteoarthritis patients with or without concurrent rotator cuff deficiency. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC9371544 PMC
- Bas Pieter Hartel, T. D. Alta, M. E. Sewnath, & W. J. Willems. (2015). Difference in clinical outcome between total shoulder arthroplasty and reverse shoulder arthroplasty used in hemiarthroplasty revision surgery. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4528286/ PMC





