Last Updated on December 3, 2025 by Bilal Hasdemir
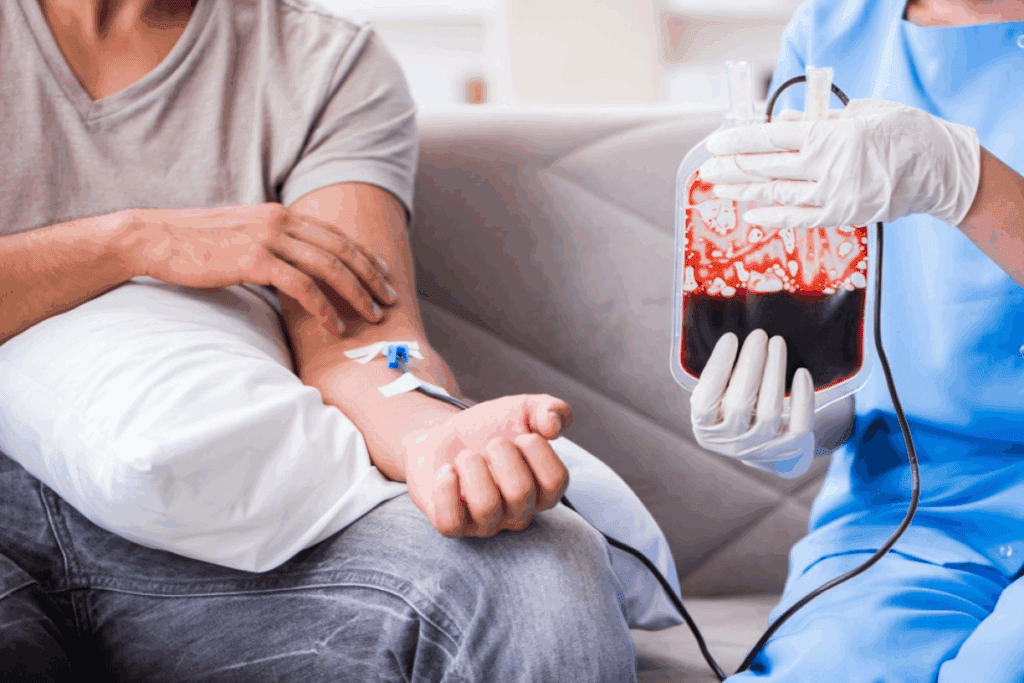
Blood transfusions are a key medical procedure. They involve moving blood or blood parts into someone’s blood flow. This is important in many medical treatments. Listing five critical clinical scenarios and blood parameter thresholds that indicate the need for a red cell Transfusion.
We will look at what a blood transfusion is and why it matters. This will help us understand its uses and when it’s needed.
Definition of Blood Transfusion
A blood transfusion is when blood or blood products are put into a patient’s blood. This can be whole blood, red blood cells, platelets, or plasma. It depends on what the patient needs.
The blood types must match to avoid bad reactions. The goal is to fix the patient’s blood levels. This helps the body get oxygen and recover from sickness or injury.
| Blood Component | Description | Clinical Use |
| Red Blood Cells | Cells that carry oxygen throughout the body | To increase oxygen delivery in cases of anemia or blood loss |
| Platelets | Cells that help the blood to clot | To prevent or treat bleeding in patients with low platelet counts |
| Plasma | The liquid portion of blood that carries proteins and nutrients | To replace clotting factors or provide albumin in critically ill patients |
Importance in Medical Treatments
Blood transfusions are vital in many medical situations. They help in surgeries, trauma care, and managing some diseases. They help restore blood, improve oxygen, and aid in recovery.
Knowing about blood transfusions shows their critical role in healthcare. They are essential for surgeries and emergency care. Blood transfusions are a key part of modern medicine.
Key Indications for Blood Transfusion
Blood transfusions are a key part of medical care. Knowing when they are needed is vital for doctors. We follow guidelines to decide if a transfusion is right, making sure patients get the best care.
Overview of Five Main Reasons
There are several reasons to transfuse blood. These include:
- Severe bleeding from injuries or surgery
- Anemia caused by diseases or not enough nutrients
- Surgical procedures that might lose a lot of blood
- Chronic conditions like hemophilia or other bleeding disorders
- Emergency situations where quick blood replacement is needed
Emergency Situations
In emergencies, blood transfusions are urgent. We quickly assess and act to save lives. Emergency blood transfusions are key in:
- Traumatic injuries with a lot of blood loss
- Severe bleeding after childbirth
- Gastrointestinal bleeding
Knowing these reasons helps doctors decide on blood transfusions. They weigh the benefits against the risks.
Anemia and Transfusion Needs
Understanding anemia is key to knowing when blood transfusions are needed. Anemia means not enough healthy red blood cells to carry enough oxygen. This is a big deal in healthcare.
What is Anemia?
Anemia is not a disease but a sign of something else. It can be caused by iron or vitamin lack, chronic diseases, or genetic issues. Low hemoglobin levels are a key sign of anemia. It can really affect a person’s life.
To diagnose anemia, doctors do blood tests. They check hemoglobin levels and the size and color of red blood cells. Knowing the cause and type of anemia helps decide the best treatment. Sometimes, blood transfusions are needed to increase red blood cells.
Types of Anemia Requiring Transfusion
Not every anemia needs a blood transfusion, but some severe ones do. For example:
- Severe iron deficiency anemia might need a transfusion if it’s sudden or if the patient is having surgery.
- Anemia caused by chronic diseases, like cancer or HIV/AIDS, may need transfusions to help tissues get enough oxygen.
- Sickle cell disease often requires transfusions to lower the risk of serious problems.
Deciding to transfuse depends on how severe the anemia is, the patient’s symptoms, and their health. Hemoglobin levels are very important in this choice. Lower levels mean a bigger need for transfusion.
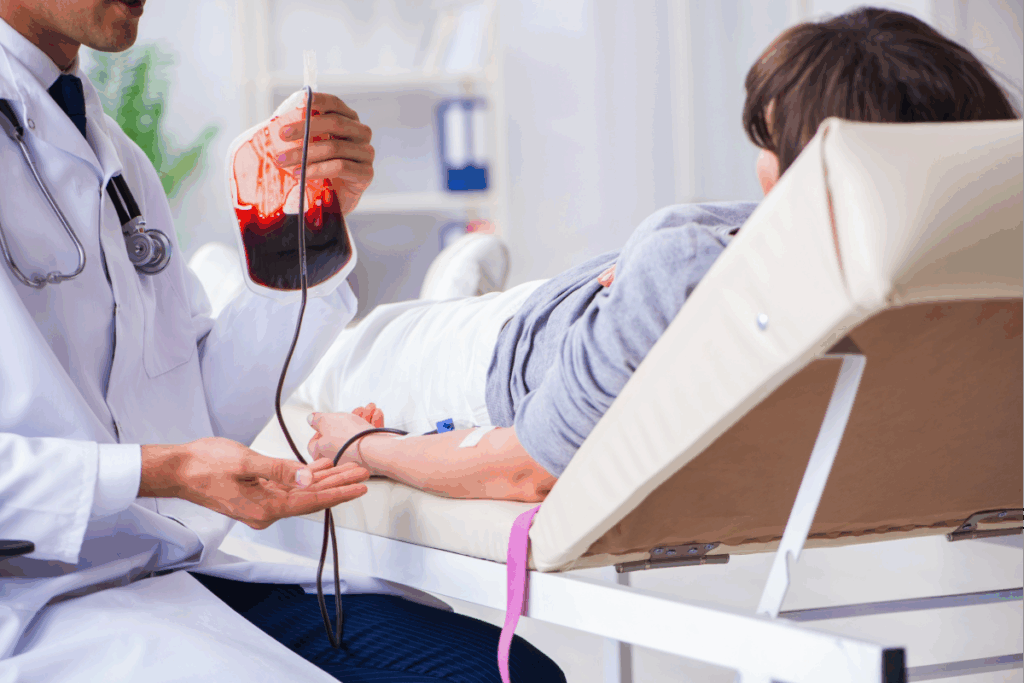
Surgery and Blood Loss
Surgery can cause a lot of blood loss, making blood transfusions very important. We know that surgeries, whether planned or urgent, come with risks. It’s key to manage blood loss to keep patients safe.
Big blood loss during surgery can harm vital organs. So, planning for blood transfusions is a big part of getting ready for surgery.
Common Surgical Procedures
Some surgeries are more likely to cause a lot of blood loss. These include:
- Orthopedic surgeries, like hip replacements or spinal fusions, because they’re complex and involve a lot of blood vessels.
- Cardiovascular surgeries, like CABG, which might need blood transfusions because of the risk of bleeding during the surgery.
- Neurosurgeries, such as tumor removals or aneurysm repairs, where precision is key and blood loss can be big.
The American Society of Anesthesiologists says, “Blood transfusion is a key part of patient care in surgeries with a lot of blood loss.”
Planning for Blood Transfusion in Surgery
Planning for blood transfusions in surgery involves several steps:
- Preoperative assessment to find out who might lose a lot of blood.
- Type and screen to know the patient’s blood type and check for antibodies that could make transfusions hard.
- Intraoperative monitoring to quickly spot and handle blood loss.
| Surgical Procedure | Average Blood Loss | Transfusion Likelihood |
| Orthopedic Surgery | 500-1000 ml | High |
| Cardiovascular Surgery | 200-500 ml | Moderate to High |
| Neurosurgery | 100-300 ml | Moderate |
By knowing the risks of blood loss in different surgeries and planning ahead, we can lower risks and get the best results for our patients.
Trauma Cases and Blood Transfusion
In trauma care, blood transfusions are a lifesaver. They can greatly improve patient outcomes. Trauma cases need quick medical help, and blood transfusions are key in managing severe blood loss.
Types of Trauma Requiring Immediate Transfusion
Several trauma types need immediate blood transfusions, including:
- Severe injuries from accidents or violence, leading to significant blood loss.
- Penetrating trauma, such as gunshot or stab wounds, which can cause major vascular damage.
- Blunt trauma, resulting from falls or vehicle collisions, potentially causing internal bleeding.
These situations require quick action to keep the patient stable and prevent further decline.
Protocols for Trauma Patients
For trauma patients, clear protocols are vital for effective care. We follow established guidelines that include:
- Rapid assessment of the patient’s condition to determine the need for blood transfusion.
- Activation of the hospital’s massive transfusion protocol when necessary, ensuring timely availability of blood products.
- Close monitoring of the patient’s vital signs and response to the transfusion.
By sticking to these protocols, we can offer the best care for trauma patients and boost their recovery chances.
Chronic Conditions and Transfusions
Blood transfusions are key in managing chronic conditions. They greatly improve the lives of patients. We’ll look at how they help, focusing on hemophilia and other blood disorders.
Hemophilia and Blood Disorders
Hemophilia is a genetic disorder that makes it hard for the body to form blood clots. There are two main types: Hemophilia A and Hemophilia B. These types lack different clotting factors. To stop bleeding, patients with hemophilia need blood transfusions, or clotting factor transfusions.
When Transfusion Becomes Necessary
Patients with chronic conditions like hemophilia need transfusions for big bleeding episodes or before surgery. The choice to transfuse depends on the condition’s severity, inhibitors, and the patient’s health.
Important factors in managing chronic conditions with transfusions include:
- The type and severity of the condition
- The presence of inhibitors or other complicating factors
- The patient’s medical history and current health status
For those with hemophilia, regular clotting factor transfusions help a lot. They reduce bleeding episodes, making life better.
Transfusion Reactions to Monitor
It’s important to know and spot transfusion reactions to keep patients safe. Blood transfusions save lives but can sometimes cause bad reactions. These reactions need quick action and care.
Recognizing Adverse Reactions
Transfusion reactions can be different in how bad they are and how they show up. You might see hemolytic reactions, febrile non-hemolytic reactions, or allergic reactions. Symptoms can be mild, like itching or urticaria, or very serious, like fever, chills, or even shock.
Doctors and nurses must watch patients closely during and after transfusions. Spotting symptoms early is key to handling them well. We use both watching the patient and lab tests to catch reactions fast.
Reporting and Managing Reactions
If a transfusion reaction is thought of, stop the transfusion right away and check the patient. We have a set plan to deal with the reaction, which includes:
- Checking the patient’s vital signs and how they’re doing.
- Telling the blood bank and the healthcare team.
- Looking into what caused the reaction.
- Starting the right treatment based on the reaction’s type and how bad it is.
Handling transfusion reactions well needs teamwork among healthcare workers. We stress the need for documentation and communication. This ensures everyone knows what’s going on.
By understanding and handling transfusion reactions, we can lower risks. This helps make sure patients get the best care when they get blood transfusions.
Ethical Considerations in Transfusion
Ethical considerations are key in blood transfusions, affecting patient care and results. The choice to have a blood transfusion is not just medical. It also involves ethical thoughts. Healthcare providers aim to follow the rules of autonomy, beneficence, non-maleficence, and justice in transfusions.
The informed consent process is vital in blood transfusions. It means telling patients about the risks, benefits, and other options. This way, patients can make choices based on full information. Informed consent builds trust between patients and healthcare teams.
Autologous vs. Allogeneic Transfusion
Choosing between autologous and allogeneic transfusions is important. Autologous transfusion uses the patient’s own blood, collected before surgery. It lowers the chance of complications and infections. Allogeneic transfusion, using donated blood, is lifesaving but carries risks like immune reactions and infections.
- Autologous Transfusion: It has fewer risks of immune reactions and infections. But, it needs planning and isn’t for all patients or surgeries.
- Allogeneic Transfusion: It’s more common and can save lives. But, it has risks like graft-versus-host disease and needs careful blood type matching.
Choosing between autologous and allogeneic transfusions involves weighing benefits and risks. We must also think about the patient’s wishes and values. The ethical side includes fair blood distribution and ethical blood donation sources.
In summary, blood transfusion ethics cover informed consent, the choice between autologous and allogeneic transfusions, and respecting patient autonomy. As transfusion medicine evolves, we must stick to these ethical standards for the best patient outcomes.
Blood Type Compatibility
Matching the donor’s blood type with the recipient’s is key to safe transfusions. It stops bad reactions from happening. These reactions happen when the immune system doesn’t like the blood.
Importance of Blood Matching
Blood matching stops serious reactions that could be deadly. Proper blood typing and cross-matching are important steps. Healthcare providers do these to make sure the blood is safe.
We have a system to figure out blood types. It includes the ABO and Rh systems. The ABO system has four types: A, B, AB, and O. The Rh system says if blood is Rh-positive or Rh-negative.
How Blood Types Affect Transfusions
The donor and recipient’s blood types must match to avoid bad reactions. Incompatible blood transfusions can cause serious problems. These include hemolysis, kidney failure, and even death.
Here’s a simple guide on how blood types work in transfusions:
| Blood Type | Can Receive | Can Donate To |
| A+ | A+, A-, O+, O- | A+, AB+ |
| O- | O- | O-, O+, A-, A+, B-, B+, AB-, AB+ |
| AB+ | All types | AB+ |
Knowing these rules is important for safe transfusions. We must match blood types carefully. This ensures the best results for patients.
Innovations in Blood Transfusion
The field of transfusion medicine is always changing. New technologies and practices are making treatments better. These advancements are key to making transfusions safer, more effective, and easier to get.
Advances in Technology and Practices
New blood transfusion technologies have made a big difference. Automated cell separators can now separate blood components more accurately. This reduces the chance of bad reactions and improves patient care.
The use of artificial intelligence (AI) and machine learning (ML) is also changing transfusion medicine. AI and ML can look at lots of data to predict how patients will react to transfusions. They can also find risks and make transfusion plans better.
Future Directions in Transfusion Medicine
The future of blood transfusions looks exciting. New trends and technologies are emerging. One promising area is synthetic blood substitutes. They could solve blood shortages and make transfusions safer.
Research is also exploring gene editing technologies to change blood cells. This could make transfusions work for more people. It might even make blood typing and matching less important.
We need to keep investing in research to make the most of these new ideas. This way, blood transfusions can stay at the top of patient care. They will offer safe, effective, and tailored treatments for those who need them.
Best Practices for Transfusion Safety
Blood transfusion safety is key in healthcare. It needs strict rules and constant learning. Keeping patients safe during blood transfusions means following strict guidelines, training healthcare workers, and keeping up with new transfusion medicine.
Protocols to Ensure Patient Safety
We follow strict rules to keep transfusions safe. These rules help lower risks. They include:
- Verifying patient identity and blood type compatibility
- Conducting thorough checks on blood products before transfusion
- Monitoring patients closely during and after transfusion
By sticking to these rules, we greatly lower the chance of bad reactions. This ensures patients get safe and effective blood transfusions.
Education and Training for Healthcare Providers
Healthcare providers need constant learning for blood transfusions. We offer detailed training. It covers the latest in transfusion safety and medicine. This includes:
- Regular workshops and seminars on transfusion safety
- Updates on new technologies and practices in blood transfusion
- Training on recognizing and managing transfusion reactions
| Best Practice | Description | Benefit |
| Patient Identification | Verifying patient identity before transfusion | Reduces risk of transfusion errors |
| Blood Product Checks | Conducting thorough checks on blood products | Ensures safety and quality of blood products |
| Monitoring During Transfusion | Closely monitoring patients during transfusion | Enables prompt response to adverse reactions |
| Ongoing Education | Providing continuous training for healthcare providers | Enhances knowledge and skills in transfusion safety |
Conclusion: The Lifesaving Role Page URL Path of Blood Transfusions
Blood transfusions are key in saving lives in many medical situations. We’ve looked at when they’re needed, like for anemia, surgery, trauma, and chronic diseases.
The need for matching blood types, following safety rules, and thinking about ethics is also important. As we keep improving in transfusion medicine, blood transfusions will stay a big part of healthcare.
Understanding the role of blood transfusions shows how complex and detailed this medical treatment is. It highlights how important they are in helping patients and saving lives.
FAQ
What is a blood transfusion?
A blood transfusion is when blood or blood parts are given to a patient. This is to replace lost blood or to boost certain blood cells.
Why are blood transfusions necessary?
Blood transfusions are needed for many medical reasons. These include severe bleeding, anemia, blood disorders, and during surgeries or trauma.
What are the main reasons for blood transfusions?
The main reasons include emergency situations like trauma. Also, surgical procedures with a lot of blood loss, anemia, and blood disorders like hemophilia. Conditions needing specific blood components also require transfusions.
What types of anemia require blood transfusions?
Anemia types needing transfusions include severe iron deficiency anemia. Also, anemia from chronic diseases and bone marrow failure or certain cancers.
How is the need for a blood transfusion determined in cases of anemia?
The need for a transfusion in anemia is based on how severe it is. It’s often measured by hemoglobin levels. Symptoms like shortness of breath, fatigue, or dizziness also play a role.
What is the threshold for hemoglobin levels that necessitates a blood transfusion?
The threshold for hemoglobin levels for a transfusion varies. It depends on the patient’s condition. Generally, below 7-8 g/dL is considered for stable patients. But, it can be higher in certain cases or for specific conditions.
How are blood transfusions planned and executed in surgical contexts?
In surgeries, transfusions are planned based on expected blood loss. The patient’s preoperative hemoglobin level and surgery type also matter. Execution involves monitoring blood loss and vital signs during surgery.
What role do blood transfusions play in trauma care?
Blood transfusions are key in trauma care. They quickly replace lost blood. This helps maintain blood pressure and ensures tissues get enough oxygen, improving survival chances.
How are chronic conditions like hemophilia managed with blood transfusions?
Chronic conditions like hemophilia are managed with transfusions. They replace missing clotting factors. This is done through specific blood components like fresh frozen plasma or cryoprecipitate to prevent or treat bleeding.
What are common transfusion reactions, and how are they managed?
Common reactions include allergic reactions, febrile non-hemolytic transfusion reactions, and hemolytic transfusion reactions. Management involves stopping the transfusion and assessing the patient. Treatment is based on the reaction type.
Why is blood type compatibility important for transfusions?
Blood type compatibility is key to avoid hemolytic transfusion reactions. These occur when the immune system reacts to incompatible blood. Ensuring compatibility involves testing the patient’s blood type and matching it with the donor blood.
What are the ethical considerations in blood transfusions?
Ethical considerations include getting informed consent from the patient. Discussing risks and benefits of transfusion is also important. Autologous and allogeneic transfusions have different ethical implications.
What advancements are being made in blood transfusion practices?
Advancements include improved blood component therapy and better testing for infectious diseases. Artificial blood substitutes are also being developed. These aim to enhance safety and availability.
How is transfusion safety maintained?
Transfusion safety is maintained through strict protocols. This includes proper identification of blood samples and units. Screening for infectious diseases and monitoring for reactions are also key. Education and training for healthcare providers are essential.
What is the significance of platelet transfusions?
Platelet transfusions are important for patients with low platelets or platelet dysfunction. They help prevent or treat bleeding. The decision to transfuse platelets depends on the platelet count and the patient’s condition.
When are red blood cell (RBC) transfusions indicated?
RBC transfusions are indicated for patients with significant anemia or blood loss. They aim to improve oxygen delivery to tissues. The decision is based on hemoglobin levels, symptoms, and the underlying cause.
References
National Institutes of Health. Evidence-Based Medical Insight. Retrieved from https://www.nhlbi.nih.gov/health/blood-transfusion





