Last Updated on November 26, 2025 by Bilal Hasdemir

An Abdominal Aortic Aneurysm (AAA) is a serious condition. It occurs when the aorta, the main blood vessel, becomes enlarged, which can be very dangerous.
Early detection and proper treatment of AAA are crucial to prevent a rupture, which can be life-threatening. Understanding the risks, diagnosis methods, and available treatment options is essential for managing this condition.
At Liv Hospital, patient care for AAA is a top priority. They follow the best practices from around the world to provide effective treatment of AAA and help patients recover safely.
Key Takeaways
- Understanding what AAA is and its risks.
- The importance of timely detection and intervention.
- Overview of diagnosis methods for AAA.
- Available treatment options for abdominal aortic aneurysm.
- The role of patient-centered care in managing AAA.
- Liv Hospital’s approach to globally competitive AAA care.
Understanding Abdominal Aortic Aneurysm (AAA)

Abdominal Aortic Aneurysm (AAA) is when the aorta in the belly gets too big. This can cause serious health problems if not treated right. It happens when the aorta gets bigger than 3 cm.
Definition and Anatomy
AAA means the aorta in the belly gets too big, bigger than 3 cm. The aorta is a key blood vessel. It brings blood to the belly, pelvis, and legs.
The aorta has three layers: intima, media, and adventitia. Damage to these layers, like from atherosclerosis, can cause an aneurysm.
The “Triple A” Medical Terminology
“Triple A” is a short way to say Abdominal Aortic Aneurysm. It’s used by doctors and patients alike.
Knowing the medical terms for AAA helps doctors and patients talk about it. It makes it easier to understand the risks and how to manage it.
Prevalence and Risk Factors
AAA is a big health problem, mostly for older people. It’s more common in men than women. The main risks are:
- Atherosclerosis: Plaque buildup in arteries weakens the aorta.
- Smoking: It damages the aorta and affects blood flow.
- Advanced Age: Risk goes up after 65.
- Male Sex: Men are more likely to get AAA.
- Family History: Having a family history of AAA increases risk.
Knowing these risks helps find and treat AAA early. Screening and awareness are key to spotting and helping those at risk.
How AAA Develops in the Body

AAA development starts with changes in the aortic wall. It moves from a normal state to an aneurysm. We need to understand how this happens.
Normal Aortic Function
The aorta is the biggest artery, carrying blood from the heart. It has three layers: intima, media, and adventitia. The media layer has elastic fibers and smooth muscle cells. This makes the aorta stretch and shrink with each heartbeat.
Pathophysiology of Aneurysm Formation
An AAA forms when the aortic wall’s proteins break down. This is due to inflammation and enzymes breaking down the wall. The weakened wall can’t handle blood pressure, causing it to bulge.
The balance between enzymes and their blockers is key. Too many enzymes, often from inflammation, can damage the wall further.
“The pathogenesis of abdominal aortic aneurysm involves a complex interplay of genetic, environmental, and biomechanical factors.”
Source: A leading vascular surgery journal
Progression of AAA Disease
AAA disease gets worse as the aneurysm grows. How fast it grows varies. Smoking, high blood pressure, and COPD can speed it up.
| Factor | Influence on AAA Progression |
| Smoking | Increases expansion rate |
| Hypertension | Contributes to wall stress |
| COPD | Associated with faster growth |
Watching how AAA grows is important. It helps decide when to act. Doctors use scans to check the size and growth of the aneurysm.
Key Fact #1: Size Matters in AAA Diagnosis
Checking the size of an AAA is key in vascular medicine. It affects how well a patient will do and what treatment they need. Doctors look at the size to see if there’s a risk of rupture and what treatment is best.
Standard Measurement Criteria
Doctors use imaging like ultrasound, CT scans, or MRI to measure an AAA. They look at the maximum diameter of the aneurysm. This is important because it shows the risk of rupture.
They measure from the outer wall to the outer wall of the aorta. This gives a clear size of the aneurysm.
Significance of AAA 4.5 cm
An AAA of 4.5 cm is considered moderate. It’s big enough to need watching but might not need surgery right away. The plan for a 4.5 cm AAA includes:
- Regular ultrasound or CT scans to check growth
- Working on risk factors like quitting smoking and controlling blood pressure
- Talking about the risks and benefits of surgery versus waiting
Growth Rate Considerations
The growth rate of an AAA is also key. Faster-growing aneurysms are at higher risk. Doctors compare measurements over time to see how fast it’s growing.
Things that can affect growth include:
- The size of the aneurysm when first found
- High blood pressure
- Smoking
- Family history of AAA
Knowing the size and growth rate helps doctors plan the best treatment for each patient.
Key Fact #2: Primary Causes of Abdominal Aortic Aneurysms
It’s important to know what causes abdominal aortic aneurysms. These conditions are complex and come from several factors.
Atherosclerosis as a Leading Cause
Atherosclerosis is the main reason for abdominal aortic aneurysms. It happens when plaque builds up in the arteries, making the aortic wall weak. Atherosclerosis affects many blood vessels and can cause aneurysms in the abdominal aorta.
Genetic and Connective Tissue Disorders
Genetic and connective tissue disorders also cause AAA. Conditions like Marfan syndrome and Ehlers-Danlos syndrome weaken the aortic wall. This shows how genetics play a big role in AAA.
Traumatic and Inflammatory Factors
Trauma and inflammation can also lead to AAA. Trauma can damage the aortic wall directly. Inflammation, like vasculitis, can make the wall weak and inflamed.
| Cause | Description | Impact on AAA Formation |
| Atherosclerosis | Buildup of plaque in arterial walls | Weakening of the aortic wall |
| Genetic and Connective Tissue Disorders | Defects in connective tissue proteins | Aortic wall weakening |
| Traumatic and Inflammatory Factors | Direct damage or inflammation of the aortic wall | Aortic wall weakening and aneurysm formation |
Knowing the main causes helps in diagnosing and treating abdominal aortic aneurysms. Understanding these factors is key to creating effective treatments.
Key Fact #3: Diagnostic Approaches for AAA
It’s important to know how to diagnose AAA early. This involves using different imaging techniques and screening based on risk factors.
Imaging Techniques for Detection
There are several ways to find AAA, each with its own benefits. Ultrasound is often the first choice because it’s safe and doesn’t use radiation. Computed Tomography (CT) scans give detailed pictures and are great for planning surgery.
The right imaging method depends on the patient’s health and the aneurysm’s size and location.
- Ultrasound: Great for first checks and follow-ups.
- CT scans: Good for detailed images and planning surgery.
- MRI: Used for detailed checks without radiation.
Visible Signs on Diagnostic Tests
Tests can show signs of AAA, like its size and shape. They also check for any problems like leaks or ruptures.
For example, a CT scan might show an AAA as a widened part of the aorta. Knowing the size and shape helps doctors decide on treatment.
- Size measurement: Important for knowing the risk of rupture.
- Morphological assessment: Helps plan surgery or other treatments.
Screening Recommendations
Screening for AAA depends on age, sex, and risk factors. Men between 65 and 75 who have smoked are usually screened once.
Those with a family history of AAA or other risks might need to be screened earlier or more often.
Doctors should look at each person’s risk and suggest the right screening.
Key Fact #4: Risk Assessment for Aneurysm Rupture
It’s key to check if an aneurysm might burst. This helps doctors decide the best treatment for abdominal aortic aneurysms (AAA). Several things can affect this risk, and doctors must look at them all to care for patients well.
Size-Related Risk Factors
The size of an aneurysm is very important. Bigger aneurysms are more likely to burst. For example, aneurysms over 5.5 cm are at high risk and often need quick action.
A study on avoiding missing AAA diagnosis says, “aneurysm size is a big factor in rupture risk” Doctors use scans like ultrasound or CT to measure aneurysm size.
Growth Rate Concerns
The rate at which an aneurysm grows is also key. Fast-growing aneurysms are more dangerous. If it grows more than 0.5 cm a year, it’s seen as risky.
“Fast-growing aneurysms are a warning sign for rupture,” say vascular health experts. Keeping an eye on aneurysm size is vital to adjust treatment plans.
Additional Risk Modifiers
Other things can also affect rupture risk. These include things like high blood pressure, smoking, and family history of AAA. For instance, someone with a family history of AAA and high blood pressure might be at higher risk, even with a small aneurysm.
A study found that high blood pressure is a big risk factor for aneurysm rupture. Managing these risks through lifestyle changes and medicine can lower the chance of rupture.
Key Fact #5: Treatment of AAA: When Intervention Is Necessary
Deciding when to treat AAA is complex. It depends on the aneurysm’s size, how fast it’s growing, and the patient’s health. Each treatment plan is unique, based on many factors.
Watchful Waiting Approach
For small aneurysms, less than 4.5 cm, a watchful waiting approach is often used. This means regular checks with tests like ultrasound or CT scans. Patients are also told how to manage their health to slow the disease.
- Regular ultrasound or CT scans to monitor aneurysm size
- Lifestyle modifications to reduce risk factors
- Management of hypertension and other cardiovascular risks
Indications for Surgical Intervention
Surgery is usually needed for aneurysms 4.5 cm or larger or those growing fast. The decision also looks at the patient’s health and symptoms.
- Aneurysm size: 4.5 cm or larger
- Rapid growth rate
- Presence of symptoms
Emergency vs. Elective Procedures
When an aneurysm ruptures, emergency surgery is urgent to save lives. For aneurysms that don’t cause symptoms but need treatment, elective repair is planned. Elective surgeries are safer than emergency ones.
Choosing between open surgery and EVAR depends on the patient’s health and anatomy. Knowing when to use each method is key to the best treatment for AAA.
Key Fact #6: Surgical Options for AAA Repair
Surgery is key in treating Abdominal Aortic Aneurysms. It’s often the best way to stop the aneurysm from rupturing and to save lives.
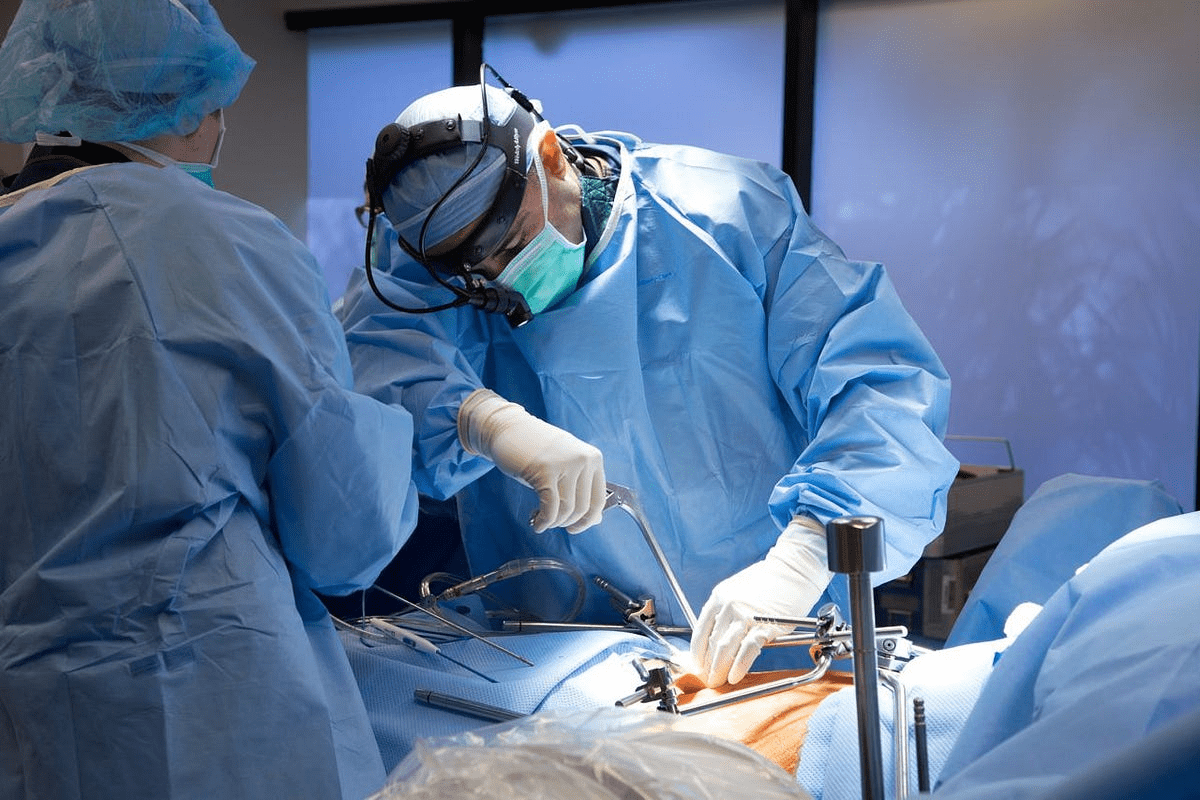
Open Surgical Repair Technique
Open surgery is a common way to fix AAAs. It involves cutting open the belly to reach the aorta. The bad part of the aorta is replaced with a man-made tube, or graft. This method needs a big cut and is more invasive than endovascular repair.
Key steps in open surgical repair include:
- Administering general anesthesia to ensure patient comfort during the procedure.
- Making a midline abdominal incision to access the aorta.
- Clamping the aorta above and below the aneurysm to allow for graft placement.
- Sewing the synthetic graft into place to replace the diseased aorta.
Recovery and Outcomes
Recovering from open surgery takes a long time. Patients often need to stay in the ICU for close watch. They might spend days or weeks in the hospital and need months to fully get better.
Factors influencing recovery include:
- The patient’s overall health and presence of comorbidities.
- The size and complexity of the aneurysm.
- The surgical team’s experience with the procedure.
Potential Complications
Open surgery is effective for AAA but has risks. These can include infection, bleeding, and heart problems.
Possible complications of open surgical repair:
| Complication | Description |
| Infection | Risk of infection at the surgical site or within the graft. |
| Bleeding | Potential for significant blood loss during or after surgery. |
| Cardiovascular Events | Risk of heart attack, stroke, or other cardiovascular complications. |
Knowing about these risks helps manage patient hopes and improve care after surgery.
Key Fact #7: Endovascular Aneurysm Repair (EVAR)
Endovascular Aneurysm Repair (EVAR) is changing how we treat Abdominal Aortic Aneurysms (AAA). It’s a new way to fix these problems with less harm. This method is getting a lot of attention for its quick recovery and fewer side effects compared to old surgery methods.
Stent Graft Procedure
The EVAR method uses a stent graft to block the aneurysm from blood. This is done through small cuts in the groin. The stent is guided by special images to the right spot in the aorta.
A vascular surgeon says, “The stent graft procedure is a big step forward for AAA patients. It’s safer and has fewer problems than old surgery.”
“The use of EVAR has significantly improved patient outcomes in AAA management.”
Advantages of Minimally Invasive Approach
EVAR is less invasive, which means it has big benefits. Patients recover faster, feel less pain, and face fewer risks. This makes EVAR a good choice for those at high risk or who want a less invasive option.
- Shorter hospital stays
- Less risk of infection
- Fewer postoperative complications
Long-term Monitoring Requirements
Even with its benefits, EVAR needs ongoing checks. This is to make sure the stent graft works well and catches any problems early. Regular scans are needed to watch the aneurysm and the stent graft.
Studies show, “Keeping an eye on patients after EVAR is key. It helps spot and handle any late problems.”
Comparing Treatment Approaches: Open Surgery vs. EVAR
Choosing between open surgery and EVAR for AAA is a big decision. Each method has its own benefits and things to think about. The right choice depends on the patient’s health, the aneurysm’s details, and what’s expected in the long run.
Patient Selection Criteria
Choosing the right treatment for AAA starts with looking at the patient. Age, health problems, aneurysm size, and shape are key. For example, EVAR might be better for those with serious health issues because it’s less invasive.
- Age and Comorbidities: Older patients or those with many health issues might do better with EVAR.
- Aneurysm Characteristics: The size, shape, and where the aneurysm is can help decide between surgery and EVAR.
Recovery Time Differences
Recovery times are different for open surgery and EVAR. Open surgery means a longer stay in the hospital and a longer recovery. EVAR, being less invasive, leads to shorter hospital stays and quicker recovery.
“The minimally invasive nature of EVAR reduces the risk of complications and promotes faster recovery, making it a preferable choice for many patients.” – Expert
Long-term Outcomes and Survival Rates
When looking at long-term results and survival rates, both open surgery and EVAR can be good choices. But, the risks and survival chances can vary between the two.
| Treatment Approach | Short-term Mortality | Long-term Survival |
| Open Surgery | Higher | Comparable to EVAR |
| EVAR | Lower | Comparable to Open Surgery |
In conclusion, picking between open surgery and EVAR for AAA is a detailed decision. It’s important to understand the differences in patient selection, recovery times, and long-term results. This helps make the best choice for each patient.
Conclusion: The Future of AAA Management
The way we manage Abdominal Aortic Aneurysm (AAA) is changing. This is thanks to new imaging tech and treatment methods. It’s important to know about stomach aneurysms and their impact on blood vessels.
Research and better vascular health are at the heart of AAA’s future. Finding and treating AAA early can stop it from rupturing. New treatments like endovascular aneurysm repair (EVAR) have made managing AAA much better.
Good AAA care needs a team effort. It involves surgery and non-surgical methods. By focusing on vascular health and using the latest in AAA management, doctors can give patients the best care.
FAQ
What is an abdominal aortic aneurysm (AAA)?
An abdominal aortic aneurysm is a swelling of the main blood vessel. It leads from the heart to the abdomen. It can be life-threatening if it ruptures.
What does AAA stand for in medical terminology?
AAA stands for Abdominal Aortic Aneurysm. It’s also known as the “Triple A” condition.
What are the primary causes of abdominal aortic aneurysms?
AAA is caused by atherosclerosis, genetic disorders, and trauma. Inflammation also plays a role.
How is AAA diagnosed?
Doctors use ultrasound, CT scans, and MRI to diagnose AAA. They also screen high-risk individuals.
What is the significance of an AAA measuring 4.5 cm?
An AAA of 4.5 cm is significant. It’s near the surgical threshold. Regular monitoring is needed to track its growth.
What are the risk factors for aneurysm rupture?
Risk factors include size, growth rate, and smoking. High blood pressure also increases the risk.
What are the treatment options for AAA?
Treatment options are watchful waiting, open surgery, and EVAR. The choice depends on the aneurysm’s size and growth rate.
What is the difference between open surgery and EVAR for AAA repair?
Open surgery requires a large incision. EVAR uses a stent graft, which is less invasive. Recovery times and outcomes differ.
What is the importance of long-term monitoring after EVAR?
Long-term monitoring after EVAR is key. It helps detect complications like endoleaks. It ensures the repair’s effectiveness.
Can AAA be prevented?
Some risk factors can’t be prevented. But, a healthy lifestyle, managing blood pressure, and quitting smoking can reduce risk.
What is the future of AAA management?
AAA management will see advances in imaging and screening. New treatments and strategies will improve patient outcomes.
Reference
- Lin, J. (2023). Status of diagnosis and therapy of abdominal aortic aneurysm: A comprehensive review. Journal of Vascular Surgery Research. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10416641/