Congenital ptosis, also known as congenital blepharoptosis, is a condition where the upper eyelid is lower than normal at birth. It affects about one in 842 babies. If not treated, it can cause serious vision problems.The ultimate guide to the treatment of congenital ptosis. Learn the best options, from observation to surgery, to protect your child’s vision.
It’s important to know the causes, symptoms, and ptosis treatment options. We’ll look at how to manage this condition. This includes watching closely and using advanced surgery.
At top hospitals like Liv Hospital, families get the care they need. Our team works hard to fix eyelid function and look. We aim to make things normal again.
Key Takeaways
- Congenital ptosis affects approximately one in 842 births.
- Untreated congenital ptosis can lead to serious vision complications.
- Modern treatment approaches range from observation to surgical techniques.
- Effective management requires understanding the condition’s causes and symptoms.
- Personalized care is available at leading medical institutions.
Understanding Congenital Ptosis

Congenital ptosis is a condition where the upper eyelid droops at birth. It’s also known as congenital blepharoptosis. This condition affects how people see and can impact their daily life.
Definition and Prevalence
Congenital ptosis means the upper eyelid falls at birth. It can happen in one or both eyes. Most cases, about 70%, affect one eye, while 30% affect both.
This condition is rare but not well-documented. It’s important to understand it to help those affected.
Anatomical Considerations
The eyelid’s anatomy is complex. It involves muscles and structures that control its movement. The levator palpebrae superioris muscle is key in lifting the eyelid.
In congenital ptosis, this muscle is often affected. Myogenic dysgenesis, where muscle tissue is replaced, weakens it. This weakness causes the eyelid to droop.
- Presence at birth
- Drooping of the upper eyelid
- Unilateral or bilateral occurrence
- Involvement of the levator palpebrae superioris muscle
- Myogenic dysgenesis as a primary cause
Causes and Mechanisms of Congenital Ptosis
It’s important to know why congenital ptosis happens. This condition makes the eyelid droop. It’s not just a simple issue but a complex one with many causes.
Congenital ptosis often comes from muscle problems. The main muscle involved is the levator palpebrae superioris. Myogenic dysgenesis is a big cause. It changes the muscle into fibrous and fatty tissues.
Myogenic Dysgenesis
Myogenic dysgenesis is the main reason for congenital ptosis. It makes the levator muscle weak. This is because it turns into fibrotic tissue. The eyelid can’t lift properly because of this.
The exact reasons for myogenic dysgenesis are not known. But, it’s thought to be caused by genetics and how the muscle develops in the womb. Studies show that problems during fetal growth might lead to this condition.
Neurologic and Neuromuscular Factors
Neurologic and neuromuscular issues also cause congenital ptosis. Problems with the nerves or the connection between nerves and muscles can stop the eyelid from moving right.
Neurologic problems like third cranial nerve palsy or Horner syndrome can affect the eyelid muscles. Rarely, neuromuscular disorders like myasthenia gravis can also cause ptosis in babies.
Knowing the cause of ptosis is key to treating it. Doctors can then plan the best treatment based on whether it’s myogenic, neurologic, or neuromuscular.
Clinical Presentation and Types
Congenital ptosis can show up in one eye or both, with different levels of severity. Knowing how it presents is key to picking the right treatment. It also helps us understand how it might affect vision.
Unilateral vs. Bilateral Ptosis
Congenital ptosis can happen in one eye (unilateral) or both (bilateral). Unilateral ptosis is more common and can make the eyes look different. This might cause some people to worry about how they look. Bilateral ptosis is less common but can really affect how well you see and develop.
It’s important to know if ptosis is in one or both eyes. This helps doctors decide the best way to treat it. It also helps them think about any possible problems.
Severity Classification
The severity of congenital ptosis is measured by the margin reflex distance (MRD1). This measures how far the upper eyelid is from the light reflex on the cornea. This helps doctors figure out how bad the ptosis is and what treatment is best.
Severity | MRD1 Measurement | Clinical Implication |
Mild | > 2 mm | Minimal impact on vision; may not require surgical intervention. |
Moderate | 0 to 2 mm | May cause some visual obstruction; surgical correction is often considered. |
Severe | < 0 mm | Significant visual obstruction; surgical intervention is usually necessary. |
Complications Associated with Untreated Ptosis
Not treating congenital ptosis can cause serious problems. These include amblyopia and refractive errors. It’s key to understand these issues to see why early treatment is so important.
Amblyopia (Lazy Eye)
Amblyopia, or “lazy eye,” happens when one eye’s vision is reduced. This is because the visual pathway in the brain didn’t develop right. Untreated congenital ptosis can block the visual path, stopping the brain from getting clear images from the affected eye. This can cause permanent vision loss if not treated early in childhood.
Refractive Errors
Untreated congenital ptosis can also lead to refractive errors. The drooping eyelid can press on the cornea or change the eye’s shape. This might cause astigmatism or other vision problems. These issues can make seeing harder and might need glasses or other treatments.
Abnormal Head Posture
Children with untreated congenital ptosis often tilt their head to see better. They might tilt it back or turn it to one side. This helps them see more, but it can cause long-term problems with muscles and facial growth.
It’s clear that not treating congenital ptosis early can lead to big problems. Quick action can prevent these issues and help eyes develop properly.
When to Seek Medical Attention
Knowing when to get medical help is key in managing congenital ptosis. As parents, it’s important to watch for signs that mean a doctor visit is needed.
Warning Signs in Infants
Infants with congenital ptosis may show signs that need quick medical check-ups. These include:
- A droopy eyelid that is noticeable at birth or develops within the first few months of life
- Difficulty opening the eye or keeping it open
- Abnormal head posture, such as tilting the head back to see
- Vision problems, including squinting or covering one eye
Watching for these signs and telling a healthcare provider can lead to early diagnosis and treatment.
Developmental Milestones
Keeping track of developmental milestones is important. It helps see how congenital ptosis affects an infant’s growth. Key milestones include:
Age | Expected Developmental Milestones |
0-3 months | Responds to visual stimuli, tracks moving objects |
4-6 months | Improve in tracking objects, start to show preference for certain visuals |
7-12 months | Demonstrate more complex visual behaviors, such as recognizing familiar faces |
If there are significant delays or difficulties in achieving these milestones, it is important to talk to a healthcare provider.
Emergency Situations
While congenital ptosis is usually not urgent, some situations need quick action. These include:
- Sudden worsening of ptosis
- Double vision or difficulty moving the eye
- Eye pain or redness
- Changes in vision, such as blurred vision
If your child shows any of these symptoms, seek medical attention immediately. Quick action can prevent problems and improve results.
Being alert to the signs and symptoms of congenital ptosis and knowing when to get medical help is critical. It ensures your child gets the best care possible.
Diagnosis and Assessment Process
Diagnosing congenital ptosis requires a detailed approach. This includes a physical exam and specialized tests. We know that getting the diagnosis right is key to finding the right treatment.
Physical Examination
The first step is a thorough physical exam. We check the eyelid’s position and function. We also measure the margin-reflex distance (MRD) and levator function. These details help us understand how severe the ptosis is and what treatment is needed.
Key components of the physical examination include:
- Eyelid position and movement assessment
- Measurement of margin-reflex distance (MRD)
- Evaluation of levator function
- Assessment for any associated ocular or systemic conditions
Specialized Tests
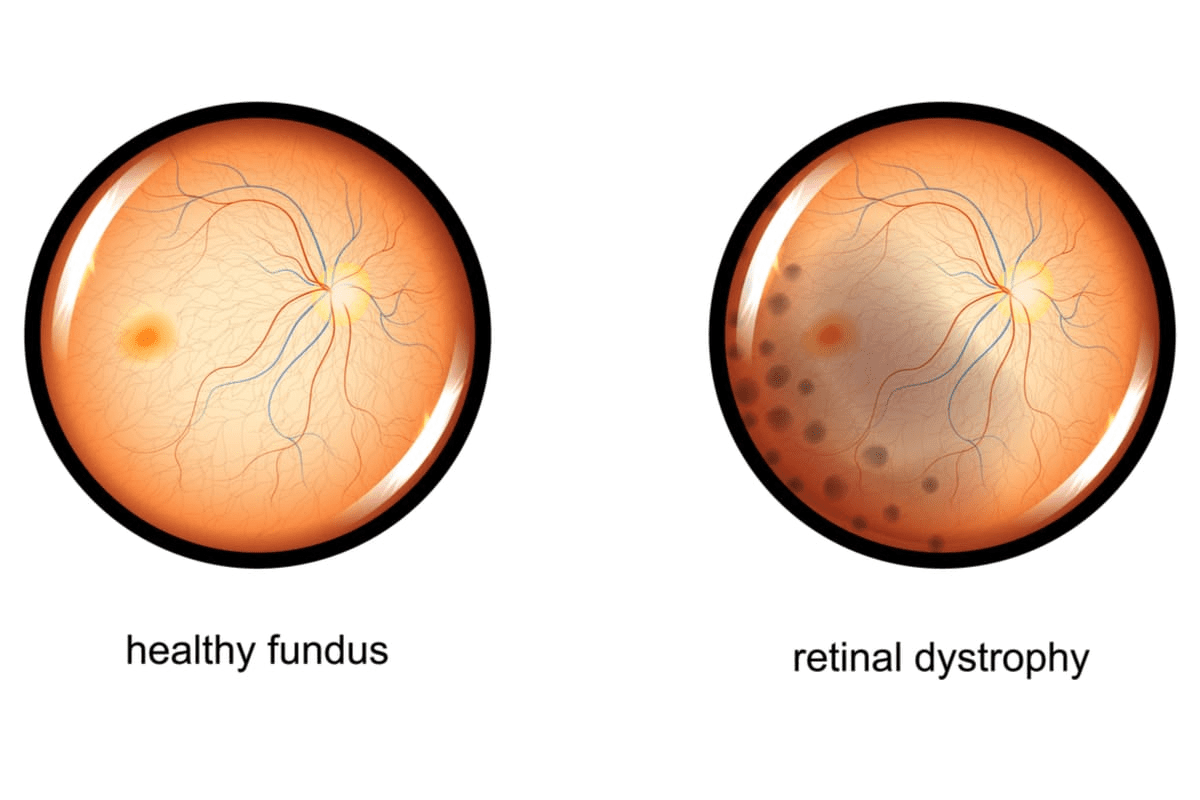
Specialized tests are also used to fully understand the condition. These tests include visual field testing and slit-lamp examination. They help us see how ptosis affects vision and the eye’s structure.
Test | Purpose |
Visual Field Testing | Assesses the impact of ptosis on the field of vision |
Slit-Lamp Examination | Evaluates the anterior segment of the eye for any abnormalities |
Eyelid Function Tests | Provides detailed information on levator function and eyelid movement |
Differential Diagnosis
Differential diagnosis is important. It helps us rule out other conditions that might look like congenital ptosis. We look at possibilities like acquired ptosis and blepharophimosis syndrome.
Accurate differential diagnosis ensures that the treatment plan is tailored to the specific needs of the patient.
By combining the results from the physical exam, specialized tests, and differential diagnosis, we get a full picture of the patient’s condition. This helps us create a treatment plan that works best for them.
Treatment of Congenital Ptosis: Decision-Making Factors
Treating congenital ptosis isn’t the same for everyone. It depends on the child’s age, how severe the ptosis is, and how it affects their vision. We look at all these factors carefully to decide the best treatment.
Age Considerations
The child’s age is very important when deciding on treatment for congenital ptosis. Young children might need different treatments than older ones. For example, very young kids might need to avoid treatments that could cause lazy eye.
As kids get older, we keep checking how well they can see and their eye health. We think about their age and how it affects their vision when planning treatment.
Severity Assessment
The severity of congenital ptosis is also key in deciding treatment. Mild cases might not affect vision much, but severe cases can block vision and cause lazy eye.
We measure the margin-reflex distance (MRD1) to see how bad the ptosis is. This tells us how much it affects the child’s vision.
Visual Function Impact
How much congenital ptosis affects a child’s vision is very important. If it blocks vision, it can cause lazy eye, which can lead to permanent vision loss if not treated.
We check how the ptosis affects the child’s daily life and happiness. This helps us decide how quickly and what kind of treatment they need.
Factor | Description | Impact on Treatment |
Age | The child’s age and developmental stage | Influences the timing and type of treatment |
Severity | The degree of ptosis as measured by MRD1 | Determines the need for surgical intervention |
Visual Function | The impact of ptosis on the child’s vision and daily activities | Affects the urgency and approach to treatment |
Non-Surgical Management Options
We have many non-surgical ways to manage congenital ptosis. These options are great for mild cases or when surgery isn’t needed right away.
Observation Protocol
For mild congenital ptosis, an observation protocol might be suggested. This means regular visits to an eye specialist. They watch the condition closely to prevent it from getting worse or causing problems like amblyopia (lazy eye).
At these visits, the specialist checks the ptosis, vision, and eye health. This way, they can act quickly if the condition gets worse or if other issues pop up.
Ptosis Crutches and Eyelid Tape
Ptosis crutches and eyelid tape are non-surgical options for some. Ptosis crutches are devices on glasses that lift the eyelid. Eyelid tape temporarily lifts the lid. These are good for kids because they’re easy to use and can be changed as needed.
Vision Therapy
Vision therapy also helps with congenital ptosis. It’s a series of exercises to improve eye movement, focus, and coordination. This therapy is great for kids with congenital ptosis who might have developed bad habits to see better.
Vision therapy can make other treatments, like surgery or non-surgery, work better. It helps improve vision overall.
Surgical Treatment Approaches
There are many surgical options for treating congenital ptosis. We look at several things before deciding on surgery. These include how severe the ptosis is, the patient’s health, and their age.
Frontalis Sling Procedure
The frontalis sling procedure is a common treatment for congenital ptosis. It’s used when the levator muscle doesn’t work well. The procedure uses a sling to connect the eyelid to the frontalis muscle.
This connection helps the eyelid lift better when the forehead moves. It’s very helpful for those with severe ptosis.
Levator Resection
Levator resection is another way to treat congenital ptosis. It shortens the levator muscle to lift the eyelid better. How much of the muscle is shortened depends on the ptosis and muscle function.
This surgery helps the eyelid open better. It’s a big help for patients with ptosis.
Müller’s Muscle Resection
Müller’s muscle resection targets the Müller’s muscle, which helps lift the eyelid. It’s often used for mild to moderate ptosis.
Removing part of Müller’s muscle improves the eyelid’s position. This makes the eye look more even.
Whitnall’s Sling
Whitnall’s sling is a type of sling procedure. It uses the Whitnall’s ligament to support the eyelid. This method provides natural and stable support.
It’s a good choice for patients with certain anatomical features. The Whitnall’s sling procedure is very effective for them.
Post-Operative Care and Recovery
After congenital ptosis surgery, proper care is key for healing. We guide you through each step of recovery. It’s as important as the surgery itself.
Immediate Aftercare
The first days are critical. Rest and avoid hard activities to prevent issues. Keep your head elevated to reduce swelling. Use ice packs as told by your doctor to lessen bruising.
Watch for signs of infection closely. Look for more redness, swelling, or discharge. Call your doctor right away if you see anything odd.
Long-Term Follow-Up
Regular check-ups are vital to see how the surgery is doing. We check on healing and make any needed changes.
We also check the child’s vision and eye alignment. Sticking to the follow-up schedule is key for the best results.
Managing Complications
Complications are rare but knowing them helps manage them. Issues like infection, undercorrection, overcorrection, and scarring can happen.
- Infection can be treated with antibiotics. It’s important to take all the medicine as directed.
- Undercorrection or overcorrection might need more surgery. We talk about the risks and benefits during follow-ups.
- Eyelid scarring can be lessened with right wound care and massage. Your doctor will show you how.
Living with Congenital Ptosis
Living with congenital ptosis is more than physical. It also affects a child’s mind and how they interact with others. Kids with this condition face special challenges that change their daily life and how they connect with others.
Psychological and Social Aspects
Congenital ptosis can hurt a child’s self-esteem and confidence. It’s vital for parents and caregivers to offer emotional support and teach coping skills.
Teasing or feeling self-conscious about their look can affect social interactions. Building resilience and promoting a positive self-image is key for their emotional health.
Support Resources for Families
Families dealing with congenital ptosis can find help. Connecting with other families who face similar issues can offer emotional support and advice.
- Support groups, online or in-person, create a sense of community.
- Professional counseling helps families deal with the emotional side of the condition.
- Educational resources help families make informed decisions about their child’s care.
School Accommodations
Children with congenital ptosis might need special help in school. Working together with parents, educators, and healthcare providers is essential to find and use these accommodations.
Accommodation | Description | Benefit |
Seating adjustments | Placing the child in a seat that minimizes the impact of ptosis on their vision or comfort. | Improves the child’s ability to focus and participate in class. |
Visual aids | Providing additional visual materials or assistive technology to support learning. | Enhances the child’s understanding and engagement with the curriculum. |
Understanding the wide effects of congenital ptosis and using available support can help families. This way, children can thrive despite the challenges they face.
Conclusion
Understanding and managing congenital ptosis is complex. It involves knowing its definition, causes, and symptoms. We’ve looked at different treatments, from non-surgical methods to surgery, and the care needed after surgery.
A congenital ptosis conclusion shows the importance of early diagnosis and treatment. This is to avoid long-term vision problems and keep eyes healthy. The right treatment depends on how severe the condition is and its effect on vision.
Healthcare teams play a big role in helping people with congenital ptosis. They can greatly improve a person’s life. It’s key to have a team of ophthalmologists, pediatricians, and other specialists working together. This ensures the best care for patients.
FAQ
What is congenital ptosis?
Congenital ptosis is when a child is born with a droopy eyelid. It can affect one or both eyes. This happens because the muscles that move the eyelid are weak or not fully developed.
How common is congenital ptosis?
Congenital ptosis is rare, affecting a small number of people. It’s one of the more common eyelid issues at birth.
What are the causes of congenital ptosis?
The main cause is myogenic dysgenesis. This is when the levator palpebrae superioris muscle doesn’t develop fully. Other factors like neurologic and neuromuscular issues can also cause it.
Can congenital ptosis correct itself?
Sometimes, mild ptosis might get better on its own. But this doesn’t happen often. Most cases need medical help to avoid problems and improve the child’s condition.
What are the complications of untreated congenital ptosis?
If left untreated, congenital ptosis can cause serious issues. These include amblyopia (lazy eye), vision problems, and abnormal head posture. These can really affect a child’s vision and development.
How is congenital ptosis diagnosed?
Doctors use a detailed physical exam and special tests to diagnose it. They also look at other possible conditions to make sure they have the right diagnosis.
What are the treatment options for congenital ptosis?
Treatment can range from non-surgical methods like watching it, using ptosis crutches, and vision therapy. Surgery, like the frontalis sling procedure, levator resection, or Müller’s muscle resection, might be needed for more severe cases.
When is surgery necessary for congenital ptosis?
Surgery is often needed for severe cases or when it affects a child’s vision a lot. The decision to have surgery depends on the child’s age and health.
What is the success rate of ptosis surgery?
The success of ptosis surgery varies. It depends on the type of surgery and the individual case. But, most surgeries do improve eyelid position and function a lot.
How can families cope with congenital ptosis?
Families can get support from doctors and resources for similar conditions. They can also make changes in school to meet their child’s needs.
Are there any long-term effects of congenital ptosis treatment?
With the right treatment, most kids with congenital ptosis see big improvements. It’s important to follow up long-term to manage any issues and ensure the best results.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/21496927/