At Liv Hospital, we know how a perforated tympanic membrane affects a person’s life and hearing. This issue, also known as a ruptured eardrum, can come from injuries, infections, or long-term ear problems. Every year, about 150,000 people get tympanoplasties, showing how big of a deal it is.
Many people with a perforated tympanic membrane don’t show symptoms, which can lead to it being overlooked. The reasons for this problem are varied, including infections, injuries, and problems caused by medical treatments. Knowing the causes and treatment options is key to managing it well.
For more details on treatments, including surgery and non-surgical methods, check out Medical organization’s guide on ruptured eardrums. We aim to give top-notch, patient-focused care to those with tympanic membrane perforation.
Key Takeaways
- Understanding the causes of tympanic membrane perforation is key to managing it.
- Treatment choices depend on the severity and cause of the perforation.
- There are surgical and non-surgical options, like tympanoplasty and patching the eardrum.
- It’s important to take care of your ears while they heal.
- Antibiotic drops might be given to treat infections that cause perforations.
Understanding Tympanic Eardrum Perforation

A perforation of the tympanic membrane is a serious issue. It can happen due to infection, trauma, or medical procedures. The eardrum is key to our hearing, passing sound vibrations to the inner ear. When it’s perforated, hearing loss, discomfort, and infection risk increase.
Common Causes of Tympanic Membrane Perforation
The main reason for tympanic membrane perforation (TMP) is acute or chronic otitis media. Infection can cause changes in the middle ear pressure. Traumatic TMPs happen from direct or indirect forces.
Infection is the top cause of TMP. Otitis media, an infection of the middle ear, can perforate the eardrum. This can be acute or chronic, with chronic being more likely to cause a perforation.
Trauma is another big cause. A direct hit to the ear, sudden loud noise, or something inserted into the ear canal can cause a perforation. Changes in air pressure, like during flights or diving, can also lead to TMP.
Medical procedures can also cause TMP. For example, inserting tympanostomy tubes to treat ear infections can sometimes lead to perforation.
| Cause | Description | Examples |
| Infection | Acute or chronic otitis media leading to eardrum perforation | Middle ear infections |
| Trauma | Direct or indirect mechanical forces causing eardrum damage | Blow to the ear, loud noise, foreign object |
| Iatrogenic | Perforation resulting from medical procedures | Tympanostomy tube insertion |
Types and Classification of Perforations
Tympanic membrane perforations are classified by location, size, and cause. Knowing these classifications helps choose the right treatment.
Central perforations happen in the middle of the eardrum, often due to chronic otitis media. Marginal perforations are at the edge and can be harder to treat because of their location.
The size of the perforation varies, from small to large. Larger ones can cause more hearing loss and might need surgery.
Perforations can be caused by trauma, medical procedures, or infection. Each type affects treatment and outcome differently.
Diagnosis and Assessment Process

Diagnosing a tympanic membrane perforation involves several steps. We use clinical exams and audiological tests to see how damaged the ear is and if it can heal.
Clinical Examination Techniques
Our first step is a clinical exam. Otoscopic examination lets us see the tympanic membrane. We check the size and location of the perforation. This helps us understand the middle ear’s condition and look for infections or other issues.
At times, we need a closer look. This might involve video otoscopy or other tools. They give us a better view of the middle ear and its structures.
Audiological Evaluation
Audiological tests are key to diagnosing. Pure-tone audiometry checks hearing levels. Tympanometry looks at the tympanic membrane’s movement and middle ear reflexes. These tests tell us how well the middle ear is working.
Factors Affecting Healing
Several things affect a perforation’s chance to heal on its own. The size and location of the perforation matter. So does any underlying condition that might slow healing. Large perforations or those covering a big part of the tympanic membrane might not heal by themselves.
We also look at the patient’s overall health. Things like middle ear infections or Eustachian tube dysfunction can affect healing. Knowing these factors helps us choose the best treatment for each patient.
Conclusion: Prognosis and Prevention
Managing tympanic membrane perforation (TMP) well is key to avoid problems and get the best results. People with TMP, including central TM perforation, should stay away from water while healing to avoid infections.
The outlook for simple TMP cases is usually good, with little chance of serious problems or lasting hearing loss. But, those who get their TM to perforate again or have other health issues face higher risks.
It’s vital to take good care of yourself after treatment and keep up with follow-ups. By following treatment plans and avoiding infections, you can lower the chance of hearing problems later on.
In short, with the right care and follow-up, people with TMP can get better and avoid serious issues.
FAQ
What are the common causes of tympanic membrane perforation?
The most frequent cause is a middle ear infection, where fluid pressure bursts the membrane. Other causes include acoustic trauma from loud noises, sudden air pressure changes (barotrauma), and physical injury, such as inserting objects too far into the ear canal.
What are the symptoms of tympanic membrane perforation?
Common symptoms include sudden ear pain that may subside quickly, followed by drainage that is clear, bloody, or pus-filled. You may also experience tinnitus (ringing), a spinning sensation (vertigo), and muffled or decreased hearing in the affected ear.
How is tympanic membrane perforation diagnosed?
A doctor diagnoses a perforation using an otoscope to look into the ear canal and see the tear directly. They may also use a pressure test called tympanometry or a hearing test (audiometry) to determine how the rupture has affected your ability to hear.
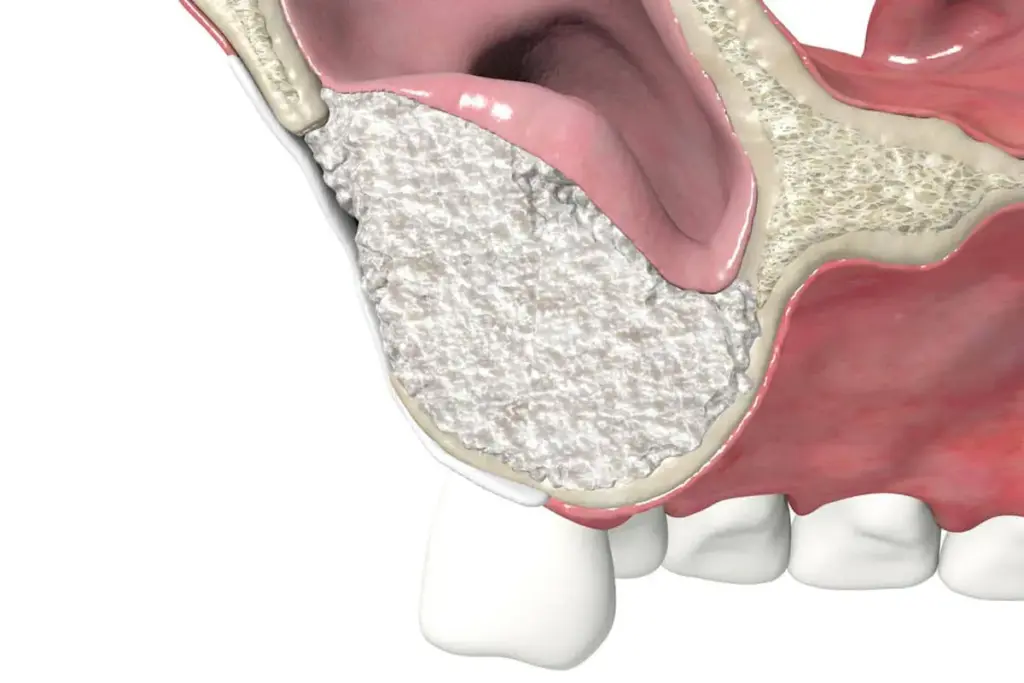
What are the treatment options for tympanic membrane perforation?
Small perforations usually heal on their own, though a doctor might apply a paper patch to assist the process. For larger or persistent holes, a surgical procedure called a tympanoplasty is performed to graft a small piece of tissue over the opening.
What is the prognosis for patients with tympanic membrane perforation?
The prognosis is excellent, with most eardrums healing within weeks to a few months. Hearing typically returns to normal once the membrane is intact, provided there was no significant damage to the tiny bones behind the eardrum.
How can complications be prevented?
The most critical step is to keep the ear strictly dry by using waterproof plugs while showering to prevent bacteria from entering the middle ear. You should also avoid blowing your nose forcefully, as the resulting pressure can interfere with the healing tissue.
What is the risk of reperforation after surgical repair?
Surgical repair has a high success rate, often exceeding 80%. However, the risk of a new tear exists if you experience a subsequent ear infection, severe pressure changes, or chronic Eustachian tube dysfunction that creates a vacuum in the middle ear.
Yes, most small-to-medium ruptures heal spontaneously because the eardrum tissue has a natural regenerative capacity. Even so, a medical professional should monitor the healing to ensure an infection doesn’t develop and to confirm the hole has fully closed.What is tympanic membrane perforation?
A tympanic membrane perforation is a hole or tear in the thin tissue that separates your ear canal from your middle ear, commonly known as a ruptured eardrum. It is responsible for converting sound waves into nerve impulses and protecting the middle ear from bacteria and water.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK557887/[3