Anemia is a condition that affects nearly a quarter of the world’s population, according to the World Health Organization. This staggering prevalence shows how important it is to know about anemia and its types.
We will look at the different kinds of anemia. This condition means not having enough healthy red blood cells. Understanding anemia is key for finding and treating it right.
By exploring the four main types, we hope to give a detailed look at this complex condition.
Key Takeaways
- Anemia affects a significant portion of the global population.
- There are four main kinds of anemia, each with distinct characteristics.
- Understanding anemia is crucial for effective diagnosis and treatment.
- The condition is characterized by a lack of healthy red blood cells.
- Diagnosis and treatment vary based on the kind of anemia.
Understanding Anemia and Its Impact on Health
Anemia is a group of diseases that can harm your health. It makes it hard for your body to carry oxygen to tissues. This leads to many health problems.
Definition and Basic Pathophysiology
Anemia means you have fewer red blood cells or less hemoglobin. Hemoglobin is a protein in red blood cells that carries oxygen. It’s about how different causes reduce red blood cells or their function.
Medical experts say, “Anemia is not a diagnosis, but a sign of a problem that needs to be found and treated.”
“Anemia is not a diagnosis, but a sign of a problem that needs to be found and treated.”
Medical Expert
There are many reasons for anemia, like blood loss, less red blood cell making, or more red blood cell destruction. Knowing these reasons helps doctors diagnose and treat anemia well.
How Anemia Affects the Body
Anemia can really affect your body. You might feel fatigue, weakness, and shortness of breath. This is because your tissues don’t get enough oxygen.
Anemia’s effects go beyond just physical health. It can make you less productive, reduce your ability to exercise, and hurt your thinking. So, it’s important to find and treat anemia quickly to lessen its impact.
Doctors can create better treatment plans by knowing the different anemia types and their effects. This helps improve patient care and outcomes.
The Four Main Types of Anemia Explained
It’s important to know about the different kinds of anemia. Anemia affects millions worldwide and can have a big impact on health.
Classification System Based on Underlying Mechanisms
We divide anemia into four main types. These are based on why it happens: blood loss, less red blood cell production, red blood cell destruction, and genetic reasons. Each type needs a different way to be treated.
- Anemia due to blood loss: This can happen from sudden or ongoing blood loss.
- Anemia due to decreased red blood cell production: It can be caused by problems in the bone marrow, not enough nutrients, or long-term diseases.
- Anemia due to destruction of red blood cells: This is when red blood cells break down too fast.
- Anemia due to genetic factors: This includes inherited conditions that affect red blood cells.
|
Type of Anemia |
Underlying Cause |
Examples |
|---|---|---|
|
Anemia due to Blood Loss |
Acute or chronic blood loss |
Surgery, trauma, gastrointestinal bleeding |
|
Anemia due to Decreased RBC Production |
Bone marrow dysfunction, nutritional deficiencies |
Iron deficiency, vitamin B12 deficiency, bone marrow failure |
|
Anemia due to Destruction of RBCs |
Intrinsic or extrinsic hemolytic mechanisms |
Autoimmune hemolytic anemia, sickle cell disease |
|
Anemia due to Genetic Factors |
Hereditary conditions affecting RBCs |
Thalassemia, hereditary spherocytosis |
Global Prevalence and Demographics
Anemia types vary worldwide, influenced by nutrition, genetics, and wealth. For example, iron deficiency anemia is common where iron is scarce. Genetic anemias like sickle cell disease are found in certain areas.
Knowing these patterns helps in fighting anemia. We need to think about these factors when planning how to prevent and treat anemia.
Type1: Anemia Due to Blood Loss
Blood loss, whether sudden or gradual, is a common cause of anemia. This happens when the body loses more red blood cells than it can make. This leads to a lack of oxygen in tissues and organs.
Acute Hemorrhagic Anemia
Acute hemorrhagic anemia is caused by sudden and significant blood loss. This can happen due to trauma, surgery, or severe injury. The immediate effect is a drop in blood volume, which can cause shock if not treated quickly.
Chronic Blood Loss Conditions
Chronic blood loss anemia develops over time due to ongoing bleeding. Common causes include gastrointestinal ulcers, menstrual disorders, and cancers. The gradual loss of blood can lead to iron deficiency, as the body’s iron stores are depleted to replace lost red blood cells.
Diagnostic Approach for Blood Loss Anemia
Diagnosing blood loss anemia involves finding the source of the bleeding. For acute cases, the diagnosis is often clear, given the sudden onset of symptoms after a traumatic event or surgery. For chronic cases, tests may include:
- Complete Blood Count (CBC) to check the level of anemia
- Iron studies to check for iron deficiency
- Endoscopy to look at the gastrointestinal tract for bleeding sources
- Imaging studies to find other possible sources of blood loss
In conclusion, anemia due to blood loss is a serious health issue that needs quick diagnosis and treatment. Knowing the causes, whether sudden or ongoing, is key for effective treatment.
Type2: Anemia Due to Decreased Red Blood Cell Production
Anemia caused by fewer red blood cells is a big problem. It happens when the bone marrow doesn’t make enough red blood cells. This can be due to many reasons.
Bone Marrow Dysfunction
Bone marrow problems are a key reason for fewer red blood cells. The bone marrow makes red blood cells, and any issues here can cause anemia. Conditions like aplastic anemia, where the bone marrow can’t make blood cells, really affect red blood cell production. Also, diseases like cancer or fibrosis in the bone marrow can stop red blood cells from being made.
Nutritional Deficiency Causes
Nutrient shortages are also a big factor in anemia. Iron, vitamin B12, and folate are key for making red blood cells. Not having enough of these can stop red blood cells from being made, leading to anemia. For example, iron deficiency anemia happens when there’s not enough iron to make hemoglobin, a key part of red blood cells.
Chronic Disease Impact on RBC Production
Chronic diseases can really hurt red blood cell production, causing anemia. Diseases like chronic kidney disease, chronic infections, and inflammatory diseases can mess with red blood cell making. Anemia of chronic disease is common when chronic inflammation stops iron from being used right and reduces red blood cell making. Knowing how chronic diseases affect red blood cell production is key to managing anemia well.
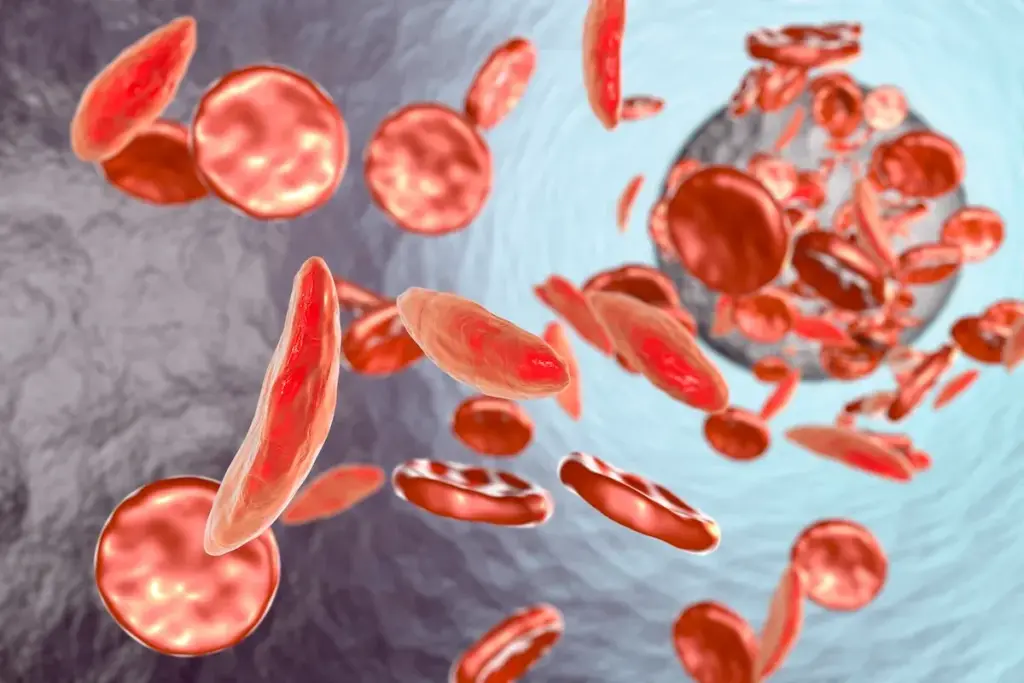
Type3: Anemia Due to Destruction of Red Blood Cells
Hemolytic anemia happens when red blood cells are destroyed too early. This can be due to problems inside the cells or from outside factors. If not treated, it can cause serious health problems.
Intrinsic Hemolytic Mechanisms
Intrinsic hemolytic mechanisms are problems inside the red blood cells. These can affect the cell membrane, how the cell works, or the hemoglobin. For example, hereditary spherocytosis makes the cell membrane weak, leading to early destruction.
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is another cause. It makes red blood cells more likely to break down when exposed to certain stressors.
Extrinsic Hemolytic Factors
Extrinsic factors are outside conditions that destroy red blood cells. These can include autoimmune disorders, infections, and some medications. Autoimmune hemolytic anemia, for instance, occurs when the immune system attacks the body’s own red blood cells.
Certain infections, like malaria, can also cause hemolytic anemia. They directly damage and destroy red blood cells.
Laboratory Findings in Hemolytic Anemia
Lab tests are key in diagnosing hemolytic anemia. They look for signs like high lactate dehydrogenase (LDH) levels and low haptoglobin levels. LDH is a marker of red blood cell breakdown, and haptoglobin binds to free hemoglobin from broken cells.
A blood smear can show signs of hemolysis, like schistocytes or spherocytes. The reticulocyte count is also high because the bone marrow tries to replace lost red blood cells.
|
Laboratory Test |
Typical Finding in Hemolytic Anemia |
|---|---|
|
Lactate Dehydrogenase (LDH) |
Elevated |
|
Haptoglobin |
Decreased |
|
Reticulocyte Count |
Elevated |
|
Peripheral Blood Smear |
Presence of schistocytes or spherocytes |
Knowing the causes and lab findings of hemolytic anemia is crucial. It helps doctors diagnose and treat it properly. By figuring out if the problem is inside the cells or from outside, they can choose the right treatment.
Type4: Anemia Due to Genetic Factors
We know that genetic anemia is a complex group of disorders. They come from inherited problems in making or working of red blood cells. These issues can greatly affect the lives of those who have them.
Hereditary RBC Membrane Disorders
Hereditary red blood cell membrane disorders are conditions with protein problems in the red blood cell membrane. These issues can cause anemia because red blood cells break down early. Examples include hereditary spherocytosis and hereditary elliptocytosis, where red blood cells are shaped wrong and break down easily.
Hemoglobin Structure Abnormalities
Hemoglobin structure abnormalities, or hemoglobinopathies, happen when genes for hemoglobin mutate. This leads to abnormal hemoglobin that can’t carry oxygen well, causing anemia. Sickle cell disease is a known example, where abnormal hemoglobin makes red blood cells sickle-shaped under stress.
Enzyme Deficiencies Affecting RBC Function
Certain enzyme deficiencies can harm red blood cell function, causing anemia. For example, glucose-6-phosphate dehydrogenase (G6PD) deficiency makes red blood cells break down easily. This is because the enzyme G6PD is either missing or doesn’t work right, making cells more prone to oxidative stress.
It’s important to understand the different types of genetic anemia. This helps healthcare providers give the right care and treatment. By knowing the causes, they can improve patient outcomes.
Iron Deficiency Anemia: Most Common Among All Types of Anemia
Iron deficiency anemia is mainly caused by not getting enough iron. This can be due to needing more iron, or losing blood over time. We will look into these reasons more closely.
Causes and Risk Factors
The main reasons for iron deficiency anemia are:
- Not getting enough iron from food
- Needing more iron during pregnancy or with certain health issues
- Loosing blood regularly due to menstruation, ulcers, or cancer
Risk factors that increase the chance of getting iron deficiency anemia include:
- Eating a poor diet
- Having health conditions like celiac disease
- Being a woman of childbearing age
Clinical Manifestations and Diagnosis
Symptoms of iron deficiency anemia can vary. They often include feeling very tired, weak, and pale. You might also have shortness of breath.
To diagnose iron deficiency anemia, doctors use several methods. They check your overall health, do blood tests like a complete blood count (CBC), and sometimes more tests to find the cause.
Treatment Strategies and Prevention
Treatment for iron deficiency anemia usually involves taking iron supplements. It also means changing your diet to eat more iron. Doctors will also try to find and fix the reason you’re losing iron.
Prevention tips include eating foods high in iron and vitamin C. Vitamin C helps your body absorb iron better. Also, avoid drinking tea and coffee with meals because they can block iron absorption.
Vitamin Deficiency Anemia: B12 and Folate Deficiencies
Lack of vitamins like B12 and folate can cause anemia. This shows how important it is to eat a balanced diet. Anemia happens when the body doesn’t have enough red blood cells or when the red blood cells don’t carry enough oxygen.
Pathophysiology of B12 Deficiency
Vitamin B12 is key for making red blood cells. Without enough B12, the body can’t make DNA for cell division. This leads to big, abnormal red blood cells that can’t carry oxygen well.
Causes of Vitamin B12 Deficiency:
- Dietary deficiency: People who don’t eat meat or animal products often lack B12.
- Malabsorption: Diseases like celiac or Crohn’s can stop the body from absorbing B12.
- Pernicious anemia: An autoimmune disease that stops the stomach from absorbing B12.
Folate Deficiency Mechanisms
Folate, or vitamin B9, is also vital for making red blood cells. Not having enough folate can cause anemia, just like B12 deficiency. It leads to big, abnormal red blood cells.
Causes of Folate Deficiency:
- Inadequate dietary intake: Not eating enough foods rich in folate.
- Increased requirement: Pregnancy and certain health issues raise folate needs.
- Malabsorption: Some small intestine problems can block folate absorption.
Diagnostic Criteria and Treatment Approaches
To find vitamin deficiency anemia, doctors use blood tests like CBC and vitamin level tests. Treatment usually means taking supplements of the missing vitamin.
|
Deficiency |
Diagnostic Test |
Treatment |
|---|---|---|
|
Vitamin B12 |
Serum vitamin B12 level |
Vitamin B12 injections or oral supplements |
|
Folate |
Serum folate level |
Folic acid oral supplements |
Knowing about vitamin deficiency anemia is key to treating it. By fixing the vitamin shortage, doctors can help patients get better and feel healthier.
Megaloblastic and Pernicious Anemia
It’s important to know about megaloblastic and pernicious anemia to treat them well. These blood disorders have unique causes and symptoms.
Characteristics of Megaloblastic Anemia
Megaloblastic anemia happens when DNA synthesis is blocked. This is often because of a lack of vitamin B12 or folate. As a result, red blood cells grow too big and can’t work right.
The main signs of megaloblastic anemia are:
- Macrocytic anemia (large red blood cells)
- Megaloblastic changes in the bone marrow
- Potential neurological symptoms, especially in B12 deficiency
Pernicious Anemia: Autoimmune Mechanisms
Pernicious anemia is caused by an autoimmune attack. It happens when the immune system attacks the stomach’s parietal cells. These cells make intrinsic factor, needed for B12 absorption.
This attack leads to:
- Less intrinsic factor made
- Worse B12 absorption
- Megaloblastic anemia develops
Long-term Management Strategies
Managing megaloblastic and pernicious anemia needs long-term plans. These plans aim to fix the underlying issues and avoid future problems.
|
Condition |
Management Strategy |
|---|---|
|
Megaloblastic Anemia |
Supplementation with vitamin B12 or folate, dietary adjustments |
|
Pernicious Anemia |
Lifelong vitamin B12 injections or oral supplements, monitoring for complications |
Knowing the unique traits and treatment plans for these anemias helps doctors give better care. This leads to better health outcomes for patients.
Hemolytic Anemia: Premature Destruction of Red Blood Cells
Hemolytic anemia happens when red blood cells are destroyed too early. This can be due to many reasons. It’s important to find and treat it quickly to improve life quality.
Autoimmune Hemolytic Anemia Subtypes
Autoimmune hemolytic anemia (AIHA) is when the immune system attacks its own red blood cells. There are two main types: warm autoimmune hemolytic anemia and cold agglutinin disease. Warm autoimmune hemolytic anemia happens at normal body temperature. Cold agglutinin disease occurs at cooler temperatures, like below 37°C.
Non-Immune Hemolytic Mechanisms
Non-immune hemolytic anemia can be caused by infections, medicines, or damage to red blood cells. For example, some infections can directly harm red blood cells. Some medicines can also cause hemolysis by changing the red blood cell membrane or triggering an immune response.
- Infections such as malaria can cause hemolytic anemia.
- Certain medications, including some antibiotics and anti-cancer drugs, can lead to hemolysis.
- Mechanical heart valves can cause mechanical damage to red blood cells.
Therapeutic Approaches and Prognosis
Treatment for hemolytic anemia depends on the cause and how severe it is. For AIHA, corticosteroids are often used first to reduce the immune system’s attack. Sometimes, immunosuppressive therapy is needed to further control the immune system. For non-immune causes, treating the underlying issue is crucial. This might mean changing medicines, managing infections, or addressing other health problems.
The outlook for people with hemolytic anemia varies. It depends on the cause, how well treatment works, and any other health issues. With the right care, many people can live active lives despite hemolytic anemia.
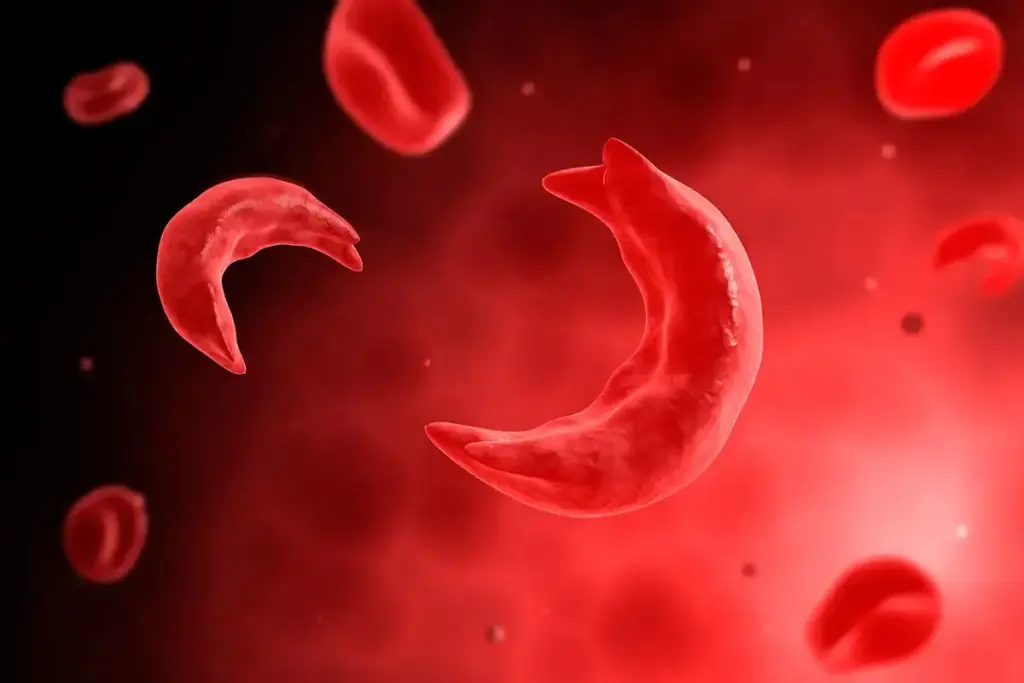
Sickle Cell Anemia: A Serious Genetic Blood Disorder
Sickle cell anemia is a serious condition where the body makes abnormal hemoglobin. This leads to red blood cells that can bend into a sickle shape. This shape makes it hard for the cells to move through blood vessels, causing health problems.
Molecular Basis and Inheritance Patterns
The cause of sickle cell anemia is a mutation in the HBB gene. This mutation makes hemoglobin S (HbS), which can cause red blood cells to sickle. People need to inherit two defective HBB genes to have the disease.
Clinical Manifestations and Complications
The symptoms of sickle cell anemia can differ from person to person. Common issues include pain episodes, anemia, infections, and a higher risk of stroke. Over time, it can also damage organs like the spleen, kidneys, and heart.
Here’s a table showing some key symptoms and complications:
|
Complication |
Description |
|---|---|
|
Sickle Cell Crises |
Episodes of pain due to vaso-occlusion by sickled red blood cells |
|
Anemia |
Chronic anemia due to reduced red blood cell lifespan |
|
Infections |
Increased susceptibility to infections, particularly pneumococcal infections |
|
Stroke |
Increased risk of stroke due to vaso-occlusion in cerebral vessels |
Current Treatment Options and Research Advances
Managing sickle cell anemia includes pain management, preventive measures, and sometimes blood transfusions or bone marrow transplants. Hydroxyurea can help reduce painful crises and may lower the need for blood transfusions.
New treatments are being researched, like gene therapy to fix the genetic defect. Advances in care and new treatments are helping improve life for those with sickle cell anemia.
Thalassemia: Spectrum of Genetic Disorders
Thalassemias are a group of genetic disorders that affect hemoglobin production. This is a key protein in red blood cells. “Thalassemia is a complex condition that requires a comprehensive management approach,” say experts in hematology.
Alpha Thalassemia Variants and Severity
Alpha thalassemia can vary from a silent carrier state to Hemoglobin Bart’s hydrops fetalis syndrome. This severe form affects all four genes, leading to severe anemia and often fetal demise without prenatal intervention.
Beta Thalassemia Classification
Beta thalassemia major, or Cooley’s anemia, is the most severe form. It requires lifelong transfusions. Beta thalassemia intermedia is milder, where patients may need occasional transfusions.
“The management of beta thalassemia major has evolved significantly with the advent of regular transfusion therapy and iron chelation,” says a highlight of the importance of comprehensive care.
Management Strategies Across the Lifespan
Regular transfusions keep hemoglobin levels up. Iron chelation therapy is key to prevent iron overload. “Early diagnosis and appropriate management can significantly improve the quality of life for individuals with thalassemia,” says a highlight of the need for timely intervention.
Aplastic Anemia: When Bone Marrow Fails
Aplastic anemia is a rare condition where the bone marrow doesn’t make enough blood cells. This can cause fatigue, infections, and bleeding problems.
Acquired vs. Inherited Forms
Aplastic anemia can be either acquired or inherited. The acquired form is more common. It can be caused by toxins, certain medications, viral infections, or autoimmune disorders. Inherited aplastic anemia is less common and linked to genetic disorders.
Key differences between acquired and inherited aplastic anemia:
|
Characteristics |
Acquired |
Inherited |
|---|---|---|
|
Cause |
Toxins, medications, infections |
Genetic disorders |
|
Age of Onset |
Variable |
Often in childhood |
|
Family History |
Typically absent |
May be present |
Clinical Presentation and Diagnostic Workup
Symptoms of aplastic anemia include fatigue, weakness, infections, and bleeding. Doctors diagnose it with a detailed medical history, physical exam, and lab tests. These include a complete blood count (CBC) and bone marrow biopsy.
“Early diagnosis is crucial for effective management of aplastic anemia.”
“The diagnosis of aplastic anemia is based on the presence of pancytopenia and a hypocellular bone marrow.” –
Aplastic Anemia Foundation
Treatment Options from Supportive Care to Transplantation
Treatment for aplastic anemia varies based on the condition’s severity and cause. Supportive care includes blood transfusions and antibiotics to manage symptoms. Immunosuppressive therapy can help some patients, while others may need a bone marrow transplant.
- Supportive care: Blood transfusions, antibiotics
- Immunosuppressive therapy
- Bone marrow transplantation
Dealing with aplastic anemia can be tough, but the right treatment can help many patients live active lives. Our team is dedicated to giving comprehensive care and support during treatment.
Diagnosing Various Kinds of Anemia
To diagnose anemia, we use many tests and evaluations. We’ll look at how we find out what kind of anemia someone has. This includes basic tests and special ones for certain types.
Initial Laboratory Evaluation
The first step is to run some tests. These tests check the blood for red cells, hemoglobin, and more. They help us see if someone has anemia and how bad it is.
These tests can tell us a lot. For example, if the red cells are small, it might mean the person doesn’t have enough iron.
|
Laboratory Test |
Purpose |
Relevance to Anemia Diagnosis |
|---|---|---|
|
Complete Blood Count (CBC) |
Assess RBC count, hemoglobin, and hematocrit |
Provides initial diagnosis and severity assessment |
|
Reticulocyte Count |
Evaluate bone marrow activity |
Helps differentiate between production and destruction causes |
Specialized Testing for Specific Anemia Types
After the first tests, we might need more to find out the exact type of anemia. For example, tests for iron can show if someone has iron deficiency anemia. Tests for B12 and folate can help with megaloblastic anemia.
We also use special tests for other types. For instance, hemoglobin electrophoresis can spot sickle cell disease. And tests like LDH and haptoglobin can help with hemolytic anemia.
Differential Diagnosis Challenges
Figuring out what kind of anemia someone has can be tough. Symptoms and test results can look similar for different types. We have to look at the patient’s history, physical exam, and test results to make the right diagnosis.
In some cases, we might need a bone marrow biopsy. This helps us diagnose things like aplastic anemia or myelodysplastic syndromes. By using our knowledge and test results, we can create a treatment plan that fits the patient’s needs.
Comprehensive Treatment Approaches for Different Types of Anemia
Managing anemia well means using a treatment plan that fits the type of anemia. Each type needs a different way to fix the problem at its root.
Nutritional Interventions and Supplements
Many cases of anemia come from not getting enough nutrients. So, changing what you eat and taking supplements is key. For example, iron supplements help with iron deficiency anemia. An iron-rich diet is also important.
Vitamin B12 and folate deficiencies need supplements too. These vitamins are vital for our bodies.
- Iron Supplements: Essential for treating iron deficiency anemia.
- Vitamin B12 Injections: Used for pernicious anemia and vitamin B12 deficiency.
- Folate Supplements: Necessary for treating folate deficiency anemia.
Pharmacological Management Strategies
Medicines are also important in treating anemia. For instance, erythropoiesis-stimulating agents (ESAs) help make more red blood cells. This is for anemia caused by chronic disease or chemotherapy.
- ESAs for anemia associated with chronic kidney disease or cancer treatment.
- Immunosuppressive therapy for aplastic anemia and some cases of hemolytic anemia.
- Chelation therapy for patients with transfusional iron overload.
Advanced Therapies for Severe Cases
For very severe anemia, doctors might use more advanced treatments. Blood transfusions can help in urgent cases. Bone marrow transplantation is an option for severe aplastic anemia or genetic anemias.
- Blood Transfusions: Used in acute cases or for patients requiring immediate increase in red blood cell count.
- Bone Marrow Transplantation: A potentially curative option for severe aplastic anemia and some genetic disorders.
By using a treatment plan that matches the anemia type and cause, doctors can greatly improve patient results.
Prevention Strategies and Living with Chronic Anemia
To reduce anemia, we need good prevention strategies. We’ll look at how to prevent anemia, especially through nutrition. We’ll also talk about screening for those at risk and improving life for those with chronic anemia.
Nutritional Approaches to Prevention
Nutrition is key in preventing anemia, especially iron deficiency anemia. It’s important to get enough iron, vitamin B12, and folate. Eating foods rich in iron like red meat, beans, and fortified cereals helps prevent iron deficiency anemia.
Vitamin C boosts iron absorption. So, eating foods high in vitamin C, like citrus fruits, with iron-rich foods is good. But, tea and coffee can lower iron absorption, so drink them in small amounts.
Screening Recommendations for High-Risk Groups
It’s important to find and help those at high risk for anemia early. Pregnant women, young children, and people with chronic diseases are at higher risk. Regular checks can catch anemia early, preventing serious problems.
Screening uses a complete blood count (CBC) test. This test checks blood components, like hemoglobin levels. Finding anemia early through screening helps improve treatment outcomes.
|
High-Risk Group |
Screening Recommendation |
|---|---|
|
Pregnant Women |
Routine CBC during prenatal visits |
|
Young Children |
CBC at ages 1 and 2, or as recommended by pediatrician |
|
Individuals with Chronic Diseases |
Regular CBC as part of disease management |
Quality of Life Considerations for Chronic Anemia
Managing chronic anemia improves life quality. This means making lifestyle changes, like pacing activities and eating well. Regular doctor visits are also key to managing the condition.
Support from loved ones and groups is also vital. Sharing experiences and advice helps emotionally and practically in managing anemia.
Conclusion
It’s important to know about the different kinds of anemia. This knowledge helps in diagnosing and treating the condition. Anemia is complex, with many causes, and needs a detailed approach to manage.
We’ve looked at the four main types of anemia. These include anemia from blood loss, less red blood cell production, red blood cell destruction, and genetic issues. Each type has its own causes, symptoms, and treatments.
Knowing the specific anemia type helps doctors create better treatment plans. This improves patients’ lives and outcomes. Treatments include nutrition, medicines, and advanced therapies.
Managing anemia well helps reduce symptoms and tackles the root causes. This lowers the risk of serious problems and boosts health. As we learn more about anemia, we can offer better care to people everywhere.
FAQ
What are the main types of anemia?
Anemia can be caused by blood loss, less red blood cell production, or red blood cell destruction. It can also be due to genetic factors.
What is iron deficiency anemia?
Iron deficiency anemia happens when the body doesn’t have enough iron. This is needed to make hemoglobin.
What causes vitamin deficiency anemia?
Vitamin deficiency anemia is caused by not having enough B12 or folate. These vitamins are key for making red blood cells.
What is hemolytic anemia?
Hemolytic anemia is when red blood cells are destroyed too quickly. This can be due to many reasons.
What is sickle cell anemia?
Sickle cell anemia is a genetic disorder. It affects how hemoglobin is made, causing red blood cells to break down.
What is thalassemia?
Thalassemia is a genetic disorder that affects hemoglobin production. It leads to anemia and other health issues.
What is aplastic anemia?
Aplastic anemia is when the bone marrow can’t make enough blood cells. This includes red blood cells.
How is anemia diagnosed?
Doctors use lab tests like complete blood counts to diagnose anemia. They also do special tests to find the cause.
What are the treatment options for anemia?
Treatment for anemia depends on the type and cause. It can include nutrition changes, supplements, medicines, and advanced treatments.
Can anemia be prevented?
Yes, some anemia types can be prevented. This can be done through good nutrition, screenings, and early detection.
How does anemia affect quality of life?
Anemia can greatly affect your life if not treated well. It can make daily activities hard and lower your overall well-being.
What are the different kinds of anemia diseases?
Anemia diseases include iron deficiency, vitamin deficiency, sickle cell, hemolytic, aplastic, and thalassemia anemia.
Are there various types of anemia?
Yes, anemia types vary based on their causes and mechanisms.
How many types of anemia are there?
There are four main types of anemia. But there are also many subtypes, like megaloblastic and pernicious anemia.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from










