Last Updated on November 27, 2025 by Bilal Hasdemir
Nearly 100,000 Americans have bariatric procedures every year. They are looking for a way to deal with obesity and health problems.
For those with severe obesity, weight loss surgery can be a big change. There are four main surgeries: gastric bypass, sleeve gastrectomy, adjustable gastric band, and biliopancreatic diversion. Each surgery has its own good points and possible dangers.
It’s important to know the differences between these surgeries. This helps you make a good choice.
Key Takeaways
- Gastric bypass is a popular weight loss surgery option.
- Sleeve gastrectomy involves removing a large portion of the stomach.
- Adjustable gastric band is a reversible surgical procedure.
- Biliopancreatic diversion is a complex surgery with significant weight loss.
- Each surgery has its unique benefits and risks.
Understanding Bariatric Surgery
Bariatric surgery is a type of surgery that helps people lose weight. It’s important to know what it is, why it’s done, and how it came to be.
Definition and Purpose
Bariatric surgery, or weight loss surgery, changes the digestive system to help people lose weight. Its main goal is to help those with obesity lose a lot of weight. This can improve their health and make their life better.
It’s for people who can’t lose weight through diet and exercise. The surgery makes the stomach smaller or changes how food moves through the body. This helps people eat less and absorb fewer calories, leading to weight loss.
Historical Development of Weight Loss Surgery
The history of bariatric surgery goes back many years. The first surgeries for weight loss started in the 1950s. These early surgeries focused on bypassing parts of the intestine.
Over time, new methods have been developed. These include gastric bypass, sleeve gastrectomy, and adjustable gastric banding. Each new technique aims to make weight loss surgery safer and more effective.
| Decade | Significant Developments in Bariatric Surgery |
| 1950s | Introduction of intestinal bypass surgeries as the first weight loss surgical procedures. |
| 1970s-80s | Development of gastric bypass surgery, marking a significant shift towards more effective weight loss procedures. |
| 1990s-2000s | Emergence of laparoscopic techniques, reducing recovery time and scarring. |
| 2010s | Advancements in sleeve gastrectomy and other procedures, with a focus on improving safety and efficacy. |
The history of bariatric surgery shows a constant push to make it safer and more effective. As technology and our understanding of obesity grow, so do the options for weight loss surgery.
Obesity and Its Health Implications

Understanding obesity is key, as it’s more than just weight. It’s a complex condition with serious health risks. Obesity is when you have too much body fat, leading to various health problems.
Medical Definition of Obesity
Obesity is often measured by the body mass index (BMI). This is a simple height and weight calculation. A BMI of 30 or higher means you’re obese. But, BMI isn’t perfect because it doesn’t measure body fat or muscle.
Obesity Classification Based on BMI:
| BMI Category | BMI Range | Health Risk |
| Normal weight | 18.5 – 24.9 | Low |
| Overweight | 25 – 29.9 | Moderate |
| Obese | 30 or higher | High |
Health Risks Associated with Severe Obesity
Severe obesity brings many serious health risks. These include heart disease, type 2 diabetes, some cancers, and sleep apnea. These conditions can greatly reduce your quality of life and life expectancy.
When Surgical Intervention Becomes Necessary
Bariatric surgery is for those who have tried other weight loss methods and failed. It’s for people with severe obesity-related health issues. This surgery is not for everyone and needs careful evaluation.
Choosing bariatric surgery means weighing the benefits and risks. It also means making big lifestyle changes after surgery.
Types of Bariatric Surgery: An Overview
Bariatric surgeries are divided into two main types: restrictive and malabsorptive. Knowing these categories helps find the best surgery for weight loss.
Restrictive vs. Malabsorptive Procedures
Restrictive surgeries limit the amount of food the stomach can hold. This reduces calorie intake. Examples are adjustable gastric banding and sleeve gastrectomy. Malabsorptive surgeries, like biliopancreatic diversion with duodenal switch, reduce nutrient absorption to help lose weight.
The main differences are:
- Restrictive procedures limit food intake.
- Malabsorptive procedures change digestion to reduce nutrient absorption.
- Some surgeries, like gastric bypass, mix both restriction and malabsorption.
Evolution of Surgical Techniques
Bariatric surgery has greatly improved over time. Advances in laparoscopic techniques and robotic surgery have made surgeries smaller, less painful, and faster to recover from. New procedures and improved ones offer more choices for patients.
Modern bariatric surgery benefits include:
- Lower risk of complications
- Less invasive surgeries
- Shorter hospital stays
- Quicker return to normal activities
In summary, today’s bariatric surgeries offer many options for those with obesity. Understanding the differences and advancements helps patients choose the right surgery for their weight loss journey.
Gastric Bypass Surgery
The gastric bypass surgery, like Roux-en-Y, is a complex but very effective way to fight severe obesity. It has become popular because it leads to big weight loss.
Roux-en-Y Gastric Bypass Procedure
The Roux-en-Y gastric bypass makes a small pouch from the stomach and connects it to the small intestine. This change limits how much food you can eat and how much your body absorbs.
Key components of the Roux-en-Y procedure include:
- Creation of a small gastric pouch
- Rerouting of the intestine to this pouch
- Reduced food intake and altered nutrient absorption
How Gastric Bypass Works for Weight Loss
Gastric bypass surgery helps with weight loss in two ways: by limiting food intake and by reducing nutrient absorption. The smaller stomach means you can’t eat as much. The changed intestine also means your body absorbs fewer calories and nutrients.
Expected Outcomes and Success Rates
Gastric bypass surgery leads to big weight losses, with many patients seeing a big drop in BMI. The success rate is high, with many people reaching their weight loss goals.
| Weight Loss Metric | Typical Outcome |
| Excess Weight Loss | 60-80% |
| Improvement in Obesity-Related Conditions | Significant improvement or resolution |
| Long-term Weight Maintenance | Generally successful with lifestyle adjustments |
Learning about the Roux-en-Y gastric bypass and its effects on weight loss helps people make better choices for treating obesity.
Sleeve Gastrectomy
For many, sleeve gastrectomy is a life-changing chance to lose a lot of weight and get healthier. This surgery is known for its success in fighting obesity.
The Surgical Procedure in Detail
Sleeve gastrectomy removes a big part of the stomach, leaving a narrow “sleeve” or tube. It’s done laparoscopically, with small cuts and a camera. This surgery can’t be reversed, and the removed stomach part can’t be put back.
“The laparoscopic approach minimizes recovery time and reduces the risk of complications,” says a top bariatric surgeon. The surgery takes about an hour. Most patients go home in a day or two.
Mechanism of Weight Loss with Sleeve Gastrectomy
The main way sleeve gastrectomy helps with weight loss is by making the stomach smaller. This limits how much food you can eat at once, cutting down on calories. It also reduces ghrelin, a hormone that makes you hungry, helping with weight loss.
As notes, “By making the stomach smaller and changing hormone levels, sleeve gastrectomy leads to big weight loss. It’s a simpler surgery compared to others.”
Results and Effectiveness
Research shows sleeve gastrectomy can lead to losing half or more of excess weight in the first year. How well it works depends on many things, like starting weight, health, and following diet and exercise advice after surgery.
A
‘study published in the Journal of the American Medical Association found that patients who underwent sleeve gastrectomy experienced significant improvements in obesity-related conditions, such as type 2 diabetes and hypertension.’
In summary, sleeve gastrectomy is known for helping people lose weight and improve health. It can also help with many obesity-related health problems, making life better for those who have it.
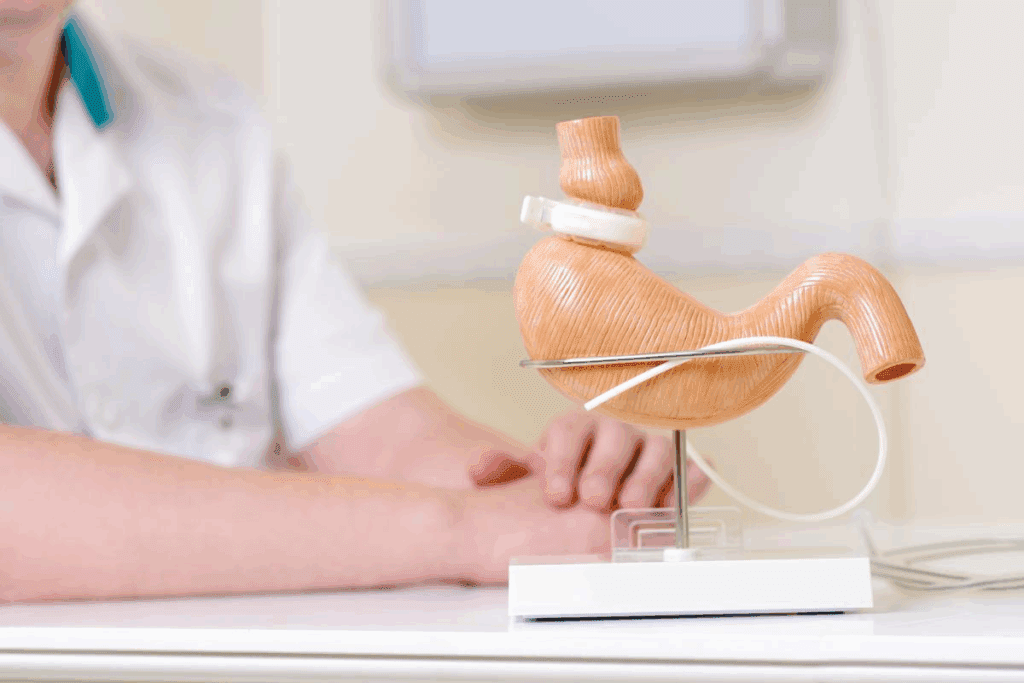
Adjustable Gastric Band
The adjustable gastric band is a unique bariatric surgery option. It’s known for being adjustable and reversible. This method involves placing a band around the upper stomach. It creates a small pouch to limit food intake.
The Banding Procedure Explained
The banding procedure is done laparoscopically, which is a minimally invasive method. The band is placed around the upper stomach. Its tightness can be adjusted after surgery to control food intake.
This adjustability is a big plus. It allows for personalized adjustments based on the patient’s progress and comfort.
A leading bariatric surgeon says, “The adjustable gastric band is a versatile option. It can be tailored to the individual needs of the patient. This makes it an attractive choice for those seeking a reversible weight-loss solution.”
“The key to successful weight loss with the adjustable gastric band lies in its adjustability and the patient’s commitment to lifestyle changes.”
Adjustments and Maintenance Requirements
After surgery, the band’s tightness is adjusted by adding or removing saline solution. This is done through a port under the skin. Regular follow-ups with a healthcare provider are needed to monitor progress and make adjustments.
Proper maintenance and adjustments are keyfor significant weight loss.
- Regular follow-up appointments for band adjustments
- Dietary counseling to ensure proper nutrition
- Monitoring for possible complications
Outcomes and Success Rates
Studies show that the adjustable gastric band can lead to significant weight loss. The amount of weight lost varies among individuals. Success rates are generally high for those who follow post-surgery guidelines and make lifestyle changes.
The outcomes of adjustable gastric banding are promising. Many patients see improvements in health conditions like diabetes and hypertension. But, it’s important to have realistic expectations and understand that results can vary.
Biliopancreatic Diversion with Duodenal Switch
The biliopancreatic diversion with duodenal switch is a very effective but complex bariatric surgery.
This surgery has two main parts. First, a sleeve gastrectomy reduces the stomach size. Then, a duodenal switch changes how food moves through the intestines, cutting down on nutrient absorption.
Complex Surgical Approach
The surgery starts with a sleeve gastrectomy. A big part of the stomach is removed, leaving a narrow sleeve. This limits how much food a person can eat.
The second step is to reroute the intestines. This is done by dividing the small intestine and reconnecting it in a way that food bypasses a lot of it. This reduces calorie and nutrient absorption.
How It Affects Digestion and Nutrient Absorption
This surgery changes how the body digests and absorbs nutrients. The smaller stomach limits food intake. The intestines’ rerouting cuts down on nutrient absorption, mainly fats.
This approach leads to a lot of weight loss. It restricts food intake and reduces calorie absorption.
Results and Long-term Effects
People who have this surgery often lose a lot of weight. This improves health problems linked to obesity.
| Weight Loss Outcome | Percentage of Excess Weight Lost |
| 1 Year Post-Surgery | 70-80% |
| 2 Years Post-Surgery | 80-90% |
| 5 Years Post-Surgery | 70-80% |
But, the surgery needs a lifelong commitment to diet and vitamin supplements. This is to avoid nutritional deficiencies.
Comparing the Four Bariatric Surgery Types
Choosing the right bariatric surgery means looking at the four types. We need to consider how well they work, their risks, and what changes you’ll need to make after surgery. Each surgery has its own benefits and things to watch out for.
Weight Loss Effectiveness Comparison
The success of bariatric surgery in losing weight varies. Gastric Bypass Surgery and Biliopancreatic Diversion with Duodenal Switch often lead to the most weight loss. People can lose a big part of their extra weight.
Here’s a look at how much weight you might lose with each surgery:
| Bariatric Surgery Type | Average Excess Weight Loss |
| Gastric Bypass Surgery | 60-80% |
| Sleeve Gastrectomy | 50-70% |
| Adjustable Gastric Band | 40-60% |
| Biliopancreatic Diversion with Duodenal Switch | 70-90% |
Risk and Complication Profiles
Each surgery comes with its own risks and possible problems. Gastric Bypass Surgery and Biliopancreatic Diversion with Duodenal Switch are more complex. They can lead to nutritional issues and surgical problems.
- Gastric Bypass Surgery: Risk of vitamin deficiencies, internal hernias
- Sleeve Gastrectomy: Risk of leaks, strictures
- Adjustable Gastric Band: Risk of band slippage, erosion
- Biliopancreatic Diversion with Duodenal Switch: Risk of malabsorption, protein deficiency
Lifestyle Adjustments Required Post-Surgery
After surgery, making lifestyle changes is key. You’ll need to follow a strict diet and take nutritional supplements to avoid deficiencies. Also, you should aim to be active every day.
Knowing the differences in weight loss, risks, and lifestyle changes helps you choose the best surgery for you.
Patient Eligibility for Bariatric Surgery
To qualify for bariatric surgery, patients go through a detailed evaluation. This evaluation looks at many health aspects. It’s key to see if a patient is right for the surgery.
BMI Requirements and Guidelines
One main factor is the patient’s Body Mass Index (BMI). A BMI of 40 or higher usually means a patient can get surgery. If a patient’s BMI is 35 or higher, they might qualify if they have obesity-related health issues.
The World Health Organization sets BMI categories. These categories help figure out obesity levels:
| BMI Category | BMI Range |
| Normal weight | 18.5 – 24.9 |
| Overweight | 25 – 29.9 |
| Obesity (Class 1) | 30 – 34.9 |
| Obesity (Class 2) | 35 – 39.9 |
| Obesity (Class 3) | 40 or higher |
Health Conditions and Considerations
Besides BMI, health conditions matter a lot. Issues like type 2 diabetes, high blood pressure, and sleep apnea are looked at closely. How these conditions affect the patient’s health is key to deciding if surgery is a good idea.
Common health conditions considered:
- Type 2 diabetes
- Hypertension
- Sleep apnea
- Joint problems
- Gastroesophageal reflux disease (GERD)
Psychological Evaluation Process
A psychological evaluation is very important. It checks if the patient is mentally ready for surgery and can make lifestyle changes afterward. This usually involves talking to a psychologist or psychiatrist and might include tests to check mental health.
The goals of the psychological evaluation are:
- Check the patient’s motivation and what they expect
- Find any hidden psychological issues
- Look at the patient’s support system
- See if the patient can follow post-surgery advice
Healthcare professionals use these factors to decide if a patient is eligible for bariatric surgery. They also check if the patient will likely benefit from it.
The Decision-Making Process
Deciding on bariatric surgery is complex and involves many factors. It’s a journey that needs careful thought, research, and advice from healthcare experts.
Consulting with Bariatric Specialists
First, talking to bariatric specialists is key. They offer insights into various surgeries like gastric bypass and sleeve gastrectomy. They help understand the benefits and risks of each, guiding towards a well-informed choice.
Patients should ask about the surgeon’s experience and success rates. It’s also important to discuss any worries or fears about the surgery and recovery.
Factors in Choosing the Right Procedure
Choosing the right surgery depends on several factors. These include health, BMI, past surgeries, and personal preferences. For example, those with higher BMIs might find gastric bypass or biliopancreatic diversion more suitable.
- Health status and BMI
- Previous surgical history
- Personal preferences and lifestyle
- Potential risks and complications
It’s important to consider these factors and talk to a specialist to find the best procedure.
Setting Realistic Expectations
Having realistic expectations is essential for success. Bariatric surgery is a tool for weight loss, not a quick fix. It requires a strict dietary regimen and regular exercise post-surgery.
Understanding the surgery’s outcomes and limitations is also key. While it can lead to significant weight loss, maintaining lifestyle changes is critical to avoid future weight gain.
Preoperative Preparation
Preoperative preparation is key for a successful bariatric surgery. It includes many steps to make sure patients are ready physically and emotionally.
Medical Assessments and Testing
Patients must go through detailed medical tests before surgery. These tests check for health risks and overall health.
- Complete blood count (CBC) to check for anemia or infection
- Blood chemistry tests to evaluate liver and kidney function
- Electrocardiogram (ECG) to assess heart health
- Chest X-ray or other imaging tests as required
These tests help doctors understand the patient’s health. They make any needed changes before surgery.
| Test | Purpose |
| Complete Blood Count (CBC) | Checks for anemia or infection |
| Blood Chemistry Tests | Evaluates liver and kidney function |
| Electrocardiogram (ECG) | Assesses heart health |
Dietary Changes Before Surgery
Changing your diet is a big part of getting ready for surgery. Patients usually eat a special diet to make their liver smaller and improve surgery results.
“A well-planned preoperative diet not only reduces surgical risks but also helps patients develop healthier eating habits post-surgery.” – A , Bariatric Surgeon
The diet before surgery includes:
- Reducing calorie intake
- Avoiding high-fat foods
- Increasing protein consumption
- Staying hydrated
Mental and Emotional Preparation
Getting ready mentally and emotionally is just as important as physical preparation. Patients are advised to:
- Attend support groups to connect with others who have undergone similar experiences
- Engage in counseling or therapy to address any emotional concerns
- Set realistic expectations about the outcomes of bariatric surgery
By focusing on both physical and emotional readiness, patients can have a smoother recovery and better results in the long run.
Risks and Complications
It’s important to know the risks and complications of bariatric surgery before deciding. This surgery can help with weight loss, but it’s key to understand the possible risks.
Short-term Surgical Risks
Bariatric surgery, like any surgery, has short-term risks. These can include bleeding, infection, and problems with anesthesia. There’s also a chance of leakage from the surgery site, which can be serious if not treated quickly.
Patients might also have adverse reactions to medicines used during or after surgery. This could include blood clots or breathing problems. Choosing a skilled surgeon and following pre-surgery advice can help lower these risks.
Long-term Health Concerns
Bariatric surgery also has long-term health concerns. Complications like bowel obstruction, hernias, or stomach band issues can occur. Some patients may face metabolic changes or malabsorption problems, which can cause health issues if not managed right.
There’s also a chance of gallstones from quick weight loss. In some cases, more surgery might be needed. Regular check-ups with healthcare providers are key to avoiding these problems.
Nutritional Deficiencies and Management
Nutritional deficiencies are a big worry after bariatric surgery, mainly with malabsorptive procedures. Patients might not get enough vitamins and minerals like vitamin B12, iron, and calcium. Working closely with healthcare teams to manage these through diet and supplements is vital.
Regular blood tests are needed to check nutritional levels. Patients often need to take supplements for life. Eating well and sticking to supplement plans can help avoid nutritional deficiencies.
Postoperative Care and Recovery
After bariatric surgery, postoperative care is key. It helps patients recover and stay healthy in the long run. This time involves watching over the patient, adjusting their diet, and slowly getting back to physical activities.
Hospital Stay and Immediate Recovery
The first part of recovery is the hospital stay. It can last from a few hours to a couple of days. This depends on the surgery type and the patient’s health.
In the hospital, doctors keep an eye on the patient’s health. They manage pain and watch for any problems. Patients are encouraged to move early to prevent blood clots and aid healing.
When patients go home, they get detailed care instructions. These include wound care, managing medications, and follow-up appointments. Following these steps is important to avoid complications and ensure a smooth recovery.
Dietary Progression After Surgery
Starting with a liquid diet, patients gradually move to solid foods. A healthcare provider or nutritionist guides this process. They make sure the patient gets the right nutrients without discomfort.
Patients should eat small meals often and chew well. They should avoid foods that could cause trouble or lead to nutritional issues. Drinking plenty of water is also key.
Physical Activity Guidelines and Recommendations
Physical activity is important in recovery. Rest is needed at first, but patients should start moving more. Short walks can help improve health, aid in weight loss, and lower the risk of problems.
Following the physical activity advice from healthcare professionals is vital. These guidelines are based on the patient’s health and surgery type. Patients should avoid heavy lifting, bending, or hard activities for a while.
Long-term Lifestyle Changes
Success after bariatric surgery depends on big changes in diet and exercise. A healthier lifestyle is key for keeping weight off and improving health.
Nutritional Guidelines and Supplementation
Patients after surgery must follow a strict diet. They should eat small meals often, avoid high-calorie foods, and take vitamins and minerals as told by their doctor.
Nutritional Guidelines:
- Eat protein-rich foods first
- Choose complex carbohydrates
- Avoid sugary drinks and foods high in sugar
- Stay hydrated by drinking plenty of water
| Nutrient | Recommended Daily Intake | Food Sources |
| Protein | 60-80 grams | Lean meats, fish, eggs, dairy |
| Vitamin B12 | 2.4-2.6 mcg | Supplements, fortified foods |
| Iron | 45-60 mg | Red meat, poultry, fish, vitamin C-rich foods |
Supplementation is key to prevent nutritional deficiencies after surgery. Patients should take multivitamins, calcium, vitamin D, and other supplements as their healthcare team advises.
Exercise and Physical Activity Requirements
Regular exercise is essential for keeping weight off and staying healthy after surgery. Start with low-intensity activities like walking. Then, increase the intensity and duration over time.
Exercise Guidelines:
- Start with short walks and gradually increase duration
- Incorporate strength training to build muscle
- Aim for at least 150 minutes of moderate-intensity exercise per week
By eating well and exercising regularly, people can achieve lasting success and live a healthier, more active life after bariatric surgery.
Conclusion
Bariatric surgery is a big decision that needs careful thought. This article has covered the four main types of bariatric surgery. These include Gastric Bypass Surgery, Sleeve Gastrectomy, Adjustable Gastric Band, and Biliopancreatic Diversion with Duodenal Switch.
Each surgery has its own good points and things to watch out for. Knowing these differences is key to making a smart choice. It’s important to talk to bariatric specialists to find the best surgery for you.
In the end, it’s vital to think about the benefits and risks of bariatric surgery. You also need to consider the lifestyle changes you’ll need to make after surgery. By carefully weighing these factors, you can make a good choice and achieve your weight loss goals.
FAQ
What are the four main types of bariatric surgery?
The main types are gastric bypass, sleeve gastrectomy, adjustable gastric banding, and biliopancreatic diversion with duodenal switch.
What is the difference between restrictive and malabsorptive bariatric procedures?
Restrictive procedures, like adjustable gastric banding and sleeve gastrectomy, limit food intake. Malabsorptive procedures, such as gastric bypass and biliopancreatic diversion, change how nutrients are absorbed.
What are the eligibility criteria for bariatric surgery?
You need a BMI of 40 or higher, or 35 with obesity-related health issues. A thorough psychological and medical evaluation is also required.
How do I choose the right bariatric surgery procedure for me?
Talk to a bariatric specialist. Consider your weight loss goals, health, and lifestyle. Discuss the risks and benefits of each procedure.
What are the possible risks and complications of bariatric surgery?
Risks include short-term surgical risks and long-term health concerns. Nutritional deficiencies can be managed with proper care and follow-up.
What kind of lifestyle changes are required after bariatric surgery?
You’ll need to follow nutritional guidelines and take supplements. Regular physical activity is also important for weight loss and health.
How long does it take to recover from bariatric surgery?
The hospital stay is a few days. Full recovery takes several weeks. Follow a specific diet and physical activity guidelines during this time.
Will I need to follow a special diet after bariatric surgery?
Yes, you’ll need to follow a specific diet. This includes a gradual transition to solid foods and a lifelong commitment to healthy eating.
What kind of support is available after bariatric surgery?
You’ll have a team of healthcare professionals. This includes a surgeon, nutritionist, and counselor to support your recovery.
How effective is bariatric surgery for weight loss?
Bariatric surgery can be very effective for weight loss. The amount of weight lost varies by procedure and individual factors.
Are there any alternative weight loss options beside surgery?
Yes, there are non-surgical options. These include diet and exercise, behavioral therapy, and medication. They may be recommended for those not eligible for surgery or who prefer not to have it.
References
- Padwal, R., et al. (2012). Bariatric surgery: A systematic review and network meta-analysis. Cochrane Database of Systematic Reviews. https://www.ncbi.nlm.nih.gov/books/NBK82019/